Management of Crohn's disease in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease
- Affiliations
-
- 1Department of Internal Medicine, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan. jmwong@ntu.edu.tw
- 2Department of Pathology, Taipei City Hospital Renai Branch, Taipei, Taiwan.
- 3Division of Colorectal Surgery, Department of Surgery, Taichung Veterans General Hospital, Taichung, Taiwan.
- 4Division of Colorectal Surgery, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan.
- 5Division of Gastroenterology and Hepatology, Department of Internal Medicine, China Medical University Hospital, Taichung, Taiwan.
- 6Division of General Surgery, Department of Surgery, Shin Kong Wu Ho-Su Memorial Hospital, Taipei, Taiwan.
- 7Department of Internal Medicine, National Cheng Kung University Hospital, National Cheng Kung University College of Medicine, Tainan, Taiwan.
- 8Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Municipal Hsiaokang Hospital, Kaohsiung, Taiwan.
- 9Division of Gastroenterology, Department of Internal Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan.
- 10Division of Colon and Rectal Surgery, Department of Surgery, Mackay Memorial Hospital, Taipei, Taiwan.
- 11Division of Colon and Rectal Surgery, Department of Surgery, Taipei Veterans General Hospital, Taipei, Taiwan.
- 12Department of Surgery, National Yang-Ming University, Taipei, Taiwan.
- 13Department of Internal Medicine, Mackay Memorial Hospital, Taipei, Taiwan.
- 14Department of Pediatrics, National Taiwan University Hospital, Taipei, Taiwan.
- 15Department of Oncology, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan.
- 16Department of Medical Imaging, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan.
- 17Department of Pathology and Forensic Medicine, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan.
- 18Division of Medical Imaging, Department of Radiology, Far Eastern Memorial Hospital, New Taipei City, Taiwan.
- 19Division of Gastroenterology, Department of Internal Medicine, MacKay Memorial Hospital, Taipei, Taiwan.
- 20MacKay Junior College of Medicine, Nursing, and Management, Taipei, Taiwan.
- 21MacKay Medical College, New Taipei City, Taiwan.
- 22Department of Internal Medicine, Far Eastern Memorial Hospital, New Taipei City, Taiwan.
- 23Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan.
- 24Department of Internal Medicine, Kaohsiung Municipal Ta-Tung Hospital, Kaohsiung, Taiwan.
- 25Division of Gastroenterology, Department of Medicine, Taipei City Hospital Renai Branch, Taipei, Taiwan.
- 26Division of Gastroenterology, Department of Internal Medicine, Changhua Christian Hospital, Changhua, Taiwan.
- KMID: 2382373
- DOI: http://doi.org/10.5217/ir.2017.15.3.285
Abstract
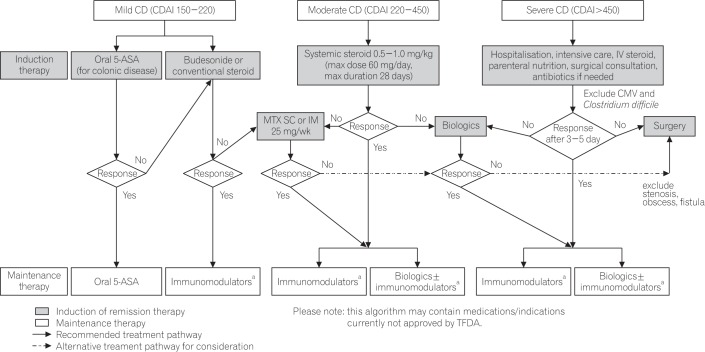
- Crohn's disease (CD) is a chronic relapsing and remitting inflammatory disease of the gastrointestinal tract. CD is rare in Taiwan and other Asian countries, but its prevalence and incidence have been steadily increasing. A steering committee was established by the Taiwan Society of Inflammatory Bowel Disease to formulate statements on the diagnosis and management of CD taking into account currently available evidence and the expert opinion of the committee. Thorough clinical, endoscopic, and histological assessments are required for accurate diagnosis of CD. Computed tomography and magnetic resonance imaging are complementary to endoscopic evaluation for disease staging and detecting complications. The goals of CD management are to induce and maintain remission, reduce the risk of complications, and improve quality of life. Corticosteroids are the mainstay for inducing re-mission. Immunomodulating and biologic therapies should be used to maintain remission. Patients should be evaluated for hepatitis B virus and tuberculosis infection prior to treatment and receive regular surveillance for cancer. These consensus statements are based on current local evidence with consideration of factors, and could be serve as concise and practical guidelines for supporting clinicians in the management of patients with CD in Taiwan.
Keyword
MeSH Terms
-
Adrenal Cortex Hormones
Asian Continental Ancestry Group
Biological Therapy
Consensus*
Crohn Disease*
Diagnosis
Disease Management
Expert Testimony
Gastrointestinal Tract
Hepatitis B virus
Humans
Incidence
Inflammatory Bowel Diseases*
Magnetic Resonance Imaging
Prevalence
Quality of Life
Taiwan*
Tuberculosis
Adrenal Cortex Hormones
Figure
Cited by 4 articles
-
Balloon-Assisted Enteroscopy and Capsule Endoscopy in Suspected Small Bowel Crohn’s Disease
Hsu-Heng Yen, Chen-Wang Chang, Jen-Wei Chou, Shu-Chen Wei
Clin Endosc. 2017;50(5):417-423. doi: 10.5946/ce.2017.142.Epidemiological trend in inflammatory bowel disease in Taiwan from 2001 to 2015: a nationwide populationbased study
Hsu-Heng Yen, Meng-Tzu Weng, Chien-Chih Tung, Yu-Ting Wang, Yuan Ting Chang, Chin-Hao Chang, Ming-Jium Shieh, Jau-Min Wong, Shu-Chen Wei
Intest Res. 2019;17(1):54-62. doi: 10.5217/ir.2018.00096.Treatment of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Eun Mi Song, Soo-Young Na, Sung Noh Hong, Siew Chien Ng, Tadakazu Hisamatsu, Byong Duk Ye
Intest Res. 2023;21(3):339-352. doi: 10.5217/ir.2022.00135.Management of Crohn’s disease in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease updated in 2023
Jia-Feng Wu, Hsu-Heng Yen, Horng-Yuan Wang, Ting-An Chang, Chung-Hsin Chang, Chen-Wang Chang, Te-Hsin Chao, Jen-Wei Chou, Yenn-Hwei Chou, Chiao-Hsiung Chuang, Wen-Hung Hsu, Tzu-Chi Hsu, Tien-Yu Huang, Tsung-I Hung, Puo-Hsien Le, Chun-Che Lin, Chun-Chi Lin, Ching-Pin Lin, Jen-Kou Lin, Wei-Chen Lin, Yen-Hsuan Ni, Ming-Jium Shieh, I-Lun Shih, Chia-Tung Shun, Tzung-Jiun Tsai, Cheng-Yi Wang, Meng-Tzu Weng, Jau-Min Wong, Deng-Chyang Wu, Shu-Chen Wei
Intest Res. 2024;22(3):250-285. doi: 10.5217/ir.2024.00060.
Reference
-
1. Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn's disease. Lancet. 2017; 389:1741–1755. PMID: 27914655.
Article2. Loftus EV Jr. Crohn's disease: why the disparity in mortality? Gut. 2006; 55:447–449. PMID: 16531525.
Article3. Selinger CP, Leong RW. Mortality from inflammatory bowel diseases. Inflamm Bowel Dis. 2012; 18:1566–1572. PMID: 22275300.
Article4. Wei SC, Lin MH, Tung CC, et al. A nationwide populationbased study of the inflammatory bowel diseases between 1998 and 2008 in Taiwan. BMC Gastroenterol. 2013; 13:166. PMID: 24314308.
Article5. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54. PMID: 22001864.
Article6. Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011; 140:1785–1794. PMID: 21530745.
Article7. Kuo CJ, Yu KH, See LC, et al. The trend of inflammatory bowel diseases in Taiwan: a population-based study. Dig Dis Sci. 2015; 60:2454–2462. PMID: 25837597.
Article8. Wang LH, Yang YJ, Cheng WC, Wang WM, Lin SH, Shieh CC. Higher risk for hematological malignancies in inflammatory bowel disease: a nationwide population-based study in Taiwan. Am J Gastroenterol. 2016; 111:1313–1319. PMID: 27296944.
Article9. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn's and colitis epidemiology study. Gastroenterology. 2013; 145:158–165. PMID: 23583432.
Article10. Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn's disease 2016: part 1: diagnosis and medical management. J Crohns Colitis. 2017; 11:3–25. PMID: 27660341.
Article11. Gionchetti P, Dignass A, Danese S, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn's disease 2016: part 2: surgical management and special situations. J Crohns Colitis. 2017; 11:135–149. PMID: 27660342.
Article12. Ooi CJ, Makharia GK, Hilmi I, et al. Asia Pacific consensus statements on Crohn's disease. Part 1: definition, diagnosis, and epidemiology: (Asia Pacific Crohn's Disease Consensus: part 1). J Gastroenterol Hepatol. 2016; 31:45–55. PMID: 25819140.
Article13. Ooi CJ, Makharia GK, Hilmi I, et al. Asia-Pacific consensus statements on Crohn's disease. Part 2: management. J Gastroenterol Hepatol. 2016; 31:56–68. PMID: 25819311.
Article14. Lichtenstein GR, Hanauer SB, Sandborn WJ. Practice Parameters Committee of American College of Gastroenterology. Management of Crohn's disease in adults. Am J Gastroenterol. 2009; 104:465–483. PMID: 19174807.
Article15. Ueno F, Matsui T, Matsumoto T, et al. Evidence-based clinical practice guidelines for Crohn's disease, integrated with formal consensus of experts in Japan. J Gastroenterol. 2013; 48:31–72. PMID: 23090001.
Article16. Lan JY. Achieving and sustaining universal health coverage: fiscal reform of the National Health Insurance in Taiwan. Appl Health Econ Health Policy. DOI: 10.1007/s40258-016-0286-6. [published online ahead of print October 25, 2016].
Article17. Shivananda S, Lennard-Jones J, Logan R, et al. Incidence of inflammatory bowel disease across Europe: is there a difference between north and south? Results of the European Collaborative Study on Inflammatory Bowel Disease (EC-IBD). Gut. 1996; 39:690–697. PMID: 9014768.
Article18. Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016; 14:111–119. PMID: 27175111.
Article19. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280. PMID: 22497584.
Article20. Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol. 2008; 103:3167–3182. PMID: 19086963.
Article21. Kim HJ, Hann HJ, Hong SN, et al. Incidence and natural course of inflammatory bowel disease in Korea, 2006-2012: a nationwide population-based study. Inflamm Bowel Dis. 2015; 21:623–630. PMID: 25647154.
Article22. Asakura K, Nishiwaki Y, Inoue N, Hibi T, Watanabe M, Takebayashi T. Prevalence of ulcerative colitis and Crohn's disease in Japan. J Gastroenterol. 2009; 44:659–665. PMID: 19424654.
Article23. Bernstein CN, Wajda A, Svenson LW, et al. The epidemiology of inflammatory bowel disease in Canada: a population-based study. Am J Gastroenterol. 2006; 101:1559–1568. PMID: 16863561.
Article24. Talley NJ, Abreu MT, Achkar JP, et al. An evidence-based systematic review on medical therapies for inflammatory bowel disease. Am J Gastroenterol. 2011; 106(Suppl 1):S2–S25. PMID: 21472012.
Article25. Gearry RB, Richardson A, Frampton CM, et al. High incidence of Crohn's disease in Canterbury, New Zealand: results of an epidemiologic study. Inflamm Bowel Dis. 2006; 12:936–943. PMID: 17012964.
Article26. Economou M, Trikalinos TA, Loizou KT, Tsianos EV, Ioannidis JP. Differential effects of NOD2 variants on Crohn's disease risk and phenotype in diverse populations: a metaanalysis. Am J Gastroenterol. 2004; 99:2393–2404. PMID: 15571588.
Article27. Strober W, Asano N, Fuss I, Kitani A, Watanabe T. Cellular and molecular mechanisms underlying NOD2 riskassociated polymorphisms in Crohn's disease. Immunol Rev. 2014; 260:249–260. PMID: 24942694.
Article28. Lee GH, Kim CG, Kim JS, Jung HC, Song IS. Frequency analysis of NOD2 gene mutations in Korean patients with Crohn's disease. Korean J Gastroenterol. 2005; 45:162–168. PMID: 15778542.29. Hsiao CH, Wei SC, Wong JM, Lai HS, Chang MH, Ni YH. Pediatric Crohn disease: clinical and genetic characteristics in Taiwan. J Pediatr Gastroenterol Nutr. 2007; 44:342–346. PMID: 17325555.
Article30. Li M, Gao X, Guo CC, Wu KC, Zhang X, Hu PJ. OCTN and CARD15 gene polymorphism in Chinese patients with inflammatory bowel disease. World J Gastroenterol. 2008; 14:4923–4927. PMID: 18756601.
Article31. Yamazaki K, Takazoe M, Tanaka T, Kazumori T, Nakamura Y. Absence of mutation in the NOD2/CARD15 gene among 483 Japanese patients with Crohn's disease. J Hum Genet. 2002; 47:469–472. PMID: 12202985.
Article32. Wei SC, Ni YH, Yang HI, et al. A hospital-based study of clinical and genetic features of Crohn's disease. J Formos Med Assoc. 2011; 110:600–606. PMID: 21930071.
Article33. Yamazaki K, Onouchi Y, Takazoe M, Kubo M, Nakamura Y, Hata A. Association analysis of genetic variants in IL23R, ATG16L1 and 5p13.1 loci with Crohn's disease in Japanese patients. J Hum Genet. 2007; 52:575–583. PMID: 17534574.
Article34. Yang SK, Lee SG, Cho YK, Lim J, Lee I, Song K. Association of TNF-alpha/LTA polymorphisms with Crohn's disease in Koreans. Cytokine. 2006; 35:13–20. PMID: 16931032.
Article35. Zipperlen K, Peddle L, Melay B, Hefferton D, Rahman P. Association of TNF-alpha polymorphisms in Crohn disease. Hum Immunol. 2005; 66:56–59. PMID: 15620462.36. Imhann F, Vich Vila A, Bonder MJ, et al. Interplay of host genetics and gut microbiota underlying the onset and clinical presentation of inflammatory bowel disease. Gut. DOI: 10.1136/gutjnl-2016-312135. [published online ahead of print October 8, 2016].
Article37. Fowler EV, Doecke J, Simms LA, et al. ATG16L1 T300A shows strong associations with disease subgroups in a large Australian IBD population: further support for significant disease heterogeneity. Am J Gastroenterol. 2008; 103:2519–2526. PMID: 18671817.
Article38. Glas J, Konrad A, Schmechel S, et al. The ATG16L1 gene variants rs2241879 and rs2241880 (T300A) are strongly associated with susceptibility to Crohn's disease in the German population. Am J Gastroenterol. 2008; 103:682–691. PMID: 18162085.
Article39. Latiano A, Palmieri O, Valvano MR, et al. Replication of interleukin 23 receptor and autophagy-related 16-like 1 association in adult- and pediatric-onset inflammatory bowel disease in Italy. World J Gastroenterol. 2008; 14:4643–4651. PMID: 18698678.
Article40. Newman WG, Zhang Q, Liu X, Amos CI, Siminovitch KA. Genetic variants in IL-23R and ATG16L1 independently predispose to increased susceptibility to Crohn's disease in a Canadian population. J Clin Gastroenterol. 2009; 43:444–447. PMID: 19276991.
Article41. Roberts RL, Gearry RB, Hollis-Moffatt JE, et al. IL23R R381Q and ATG16L1 T300A are strongly associated with Crohn's disease in a study of New Zealand Caucasians with inflammatory bowel disease. Am J Gastroenterol. 2007; 102:2754–2761. PMID: 17894849.42. Yang SK, Park M, Lim J, et al. Contribution of IL23R but not ATG16L1 to Crohn's disease susceptibility in Koreans. Inflamm Bowel Dis. 2009; 15:1385–1390. PMID: 19334001.
Article43. Zhi J, Zhi FC, Chen ZY, et al. Correlation of the autophagosome gene ATG16L1 polymorphism and inflammatory bowel disease. Nan Fang Yi Ke Da Xue Xue Bao. 2008; 28:649–651. PMID: 18495612.44. Tedesco FJ, Hardin RD, Harper RN, Edwards BH. Infectious colitis endoscopically simulating inflammatory bowel disease: a prospective evaluation. Gastrointest Endosc. 1983; 29:195–197. PMID: 6618115.
Article45. De Hertogh G, Geboes K. Crohn's disease and infections: a complex relationship. MedGenMed. 2004; 6:14.46. Pimentel M, Chang M, Chow EJ, et al. Identification of a prodromal period in Crohn's disease but not ulcerative colitis. Am J Gastroenterol. 2000; 95:3458–3462. PMID: 11151877.
Article47. Fine KD, Schiller LR. AGA technical review on the evaluation and management of chronic diarrhea. Gastroenterology. 1999; 116:1464–1486. PMID: 10348832.
Article48. Mahid SS, Minor KS, Soto RE, Hornung CA, Galandiuk S. Smoking and inflammatory bowel disease: a meta-analysis. Mayo Clin Proc. 2006; 81:1462–1471. PMID: 17120402.
Article49. Moller FT, Andersen V, Wohlfahrt J, Jess T. Familial risk of inflammatory bowel disease: a population-based cohort study 1977-2011. Am J Gastroenterol. 2015; 110:564–571. PMID: 25803400.
Article50. Eglinton TW, Barclay ML, Gearry RB, Frizelle FA. The spectrum of perianal Crohn's disease in a population-based cohort. Dis Colon Rectum. 2012; 55:773–777. PMID: 22706129.
Article51. Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn's disease activity index. National Cooperative Crohn's Disease Study. Gastroenterology. 1976; 70:439–444. PMID: 1248701.52. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987; 317:1625–1629. PMID: 3317057.
Article53. Hyams JS, Ferry GD, Mandel FS, et al. Development and validation of a pediatric Crohn's disease activity index. J Pediatr Gastroenterol Nutr. 1991; 12:439–447. PMID: 1678008.
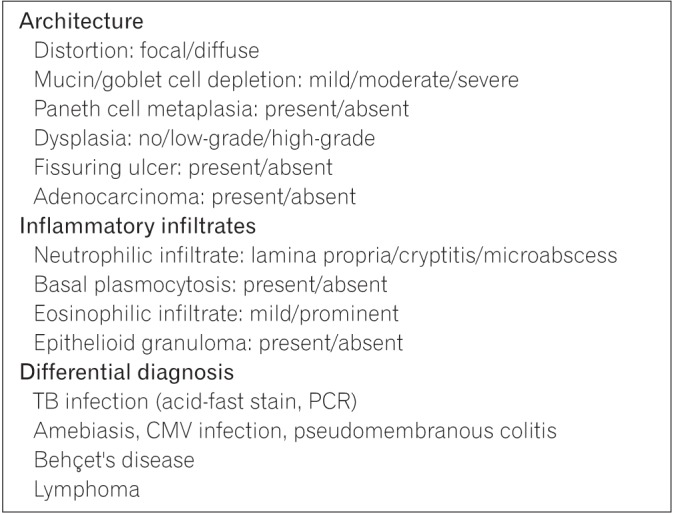
Article54. Magro F, Langner C, Driessen A, et al. European consensus on the histopathology of inflammatory bowel disease. J Crohns Colitis. 2013; 7:827–851. PMID: 23870728.
Article55. Makkar R, Bo S. Colonoscopic perforation in inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2013; 9:573–583. PMID: 24729766.56. Fausel RA, Kornbluth A, Dubinsky MC. The first endoscopy in suspected inflammatory bowel disease. Gastrointest Endosc Clin N Am. 2016; 26:593–610. PMID: 27633590.
Article57. Lee JM, Lee KM. Endoscopic diagnosis and differentiation of inflammatory bowel disease. Clin Endosc. 2016; 49:370–375. PMID: 27484813.
Article58. Mary JY, Modigliani R. Development and validation of an endoscopic index of the severity for Crohn's disease: a prospective multicentre study. Groupe d'Etudes Thérapeutiques des Affections Inflammatoires du Tube Digestif (GETAID). Gut. 1989; 30:983–989. PMID: 2668130.
Article59. Daperno M, D’Haens G, Van Assche G, et al. Development and validation of a new, simplified endoscopic activity score for Crohn's disease: the SES-CD. Gastrointest Endosc. 2004; 60:505–512. PMID: 15472670.
Article60. D'Incà R, Caccaro R. Measuring disease activity in Crohn's disease: what is currently available to the clinician. Clin Exp Gastroenterol. 2014; 7:151–161. PMID: 24876789.61. Weng MT, Wei SC, Lin CC, et al. Seminar report from the 2014 Taiwan Society of Inflammatory Bowel Disease (TSIBD) spring forum (May 24th, 2014): Crohn's disease versus intestinal tuberculosis infection. Intest Res. 2015; 13:6–10. PMID: 25691838.
Article62. Keane J, Gershon S, Wise RP, et al. Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N Engl J Med. 2001; 345:1098–1104. PMID: 11596589.
Article63. Pratap Mouli V, Munot K, Ananthakrishnan A, et al. Endoscopic and clinical responses to anti-tubercular therapy can differentiate intestinal tuberculosis from Crohn's disease. Aliment Pharmacol Ther. 2017; 45:27–36. PMID: 27813111.
Article64. Sakuraba A, Iwao Y, Matsuoka K, et al. Endoscopic and pathologic changes of the upper gastrointestinal tract in Crohn's disease. Biomed Res Int. 2014; 2014:610767. PMID: 24672792.
Article65. Annunziata ML, Caviglia R, Papparella LG, Cicala M. Upper gastrointestinal involvement of Crohn's disease: a prospective study on the role of upper endoscopy in the diagnostic work-up. Dig Dis Sci. 2012; 57:1618–1623. PMID: 22350786.
Article66. Freeman HJ. Application of the Montreal classification for Crohn's disease to a single clinician database of 1015 patients. Can J Gastroenterol. 2007; 21:363–366. PMID: 17571169.
Article67. Witte AM, Veenendaal RA, Van Hogezand RA, Verspaget HW, Lamers CB. Crohn's disease of the upper gastrointestinal tract: the value of endoscopic examination. Scand J Gastroenterol Suppl. 1998; 225:100–105. PMID: 9515760.68. de Melo, Di Palma JA. The role of capsule endoscopy in evaluating inflammatory bowel disease. Gastroenterol Clin North Am. 2012; 41:315–323. PMID: 22500520.
Article69. Dionisio PM, Gurudu SR, Leighton JA, et al. Capsule endoscopy has a significantly higher diagnostic yield in patients with suspected and established small-bowel Crohn's disease: a meta-analysis. Am J Gastroenterol. 2010; 105:1240–1248. PMID: 20029412.
Article70. Triester SL, Leighton JA, Leontiadis GI, et al. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn's disease. Am J Gastroenterol. 2006; 101:954–964. PMID: 16696781.
Article71. Leighton JA, Legnani P, Seidman EG. Role of capsule endoscopy in inflammatory bowel disease: where we are and where we are going. Inflamm Bowel Dis. 2007; 13:331–337. PMID: 17206673.72. Kopylov U, Carter D, Eliakim AR. Capsule endoscopy and deep enteroscopy in irritable bowel disease. Gastrointest Endosc Clin N Am. 2016; 26:611–627. PMID: 27633591.73. Pennazio M, Spada C, Eliakim R, et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2015; 47:352–376. PMID: 25826168.
Article74. Panes J, Bouhnik Y, Reinisch W, et al. Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis. 2013; 7:556–585. PMID: 23583097.
Article75. Feuerbach S. MRI enterography: the future of small bowel diagnostics? Dig Dis. 2010; 28:433–438. PMID: 20926869.
Article76. Migaleddu V, Scanu AM, Quaia E, et al. Contrast-enhanced ultrasonographic evaluation of inflammatory activity in Crohn's disease. Gastroenterology. 2009; 137:43–52. PMID: 19422826.
Article77. Hafeez R, Greenhalgh R, Rajan J, et al. Use of small bowel imaging for the diagnosis and staging of Crohn's disease: a survey of current UK practice. Br J Radiol. 2011; 84:508–517. PMID: 21081570.
Article78. Lee SS, Kim AY, Yang SK, et al. Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology. 2009; 251:751–761. PMID: 19276325.
Article79. Ho IK, Cash BD, Cohen H, et al. Radiation exposure in gastroenterology: improving patient and staff protection. Am J Gastroenterol. 2014; 109:1180–1194. PMID: 24842339.
Article80. Peloquin JM, Pardi DS, Sandborn WJ, et al. Diagnostic ionizing radiation exposure in a population-based cohort of patients with inflammatory bowel disease. Am J Gastroenterol. 2008; 103:2015–2022. PMID: 18564113.
Article81. Jaffe TA, Gaca AM, Delaney S, et al. Radiation doses from small-bowel follow-through and abdominopelvic MDCT in Crohn's disease. AJR Am J Roentgenol. 2007; 189:1015–1022. PMID: 17954634.
Article82. Bressenot A, Geboes K, Vignaud JM, Guéant JL, Peyrin-Biroulet L. Microscopic features for initial diagnosis and disease activity evaluation in inflammatory bowel disease. Inflamm Bowel Dis. 2013; 19:1745–1752. PMID: 23782793.
Article83. Jenkins D, Balsitis M, Gallivan S, et al. Guidelines for the initial biopsy diagnosis of suspected chronic idiopathic inflammatory bowel disease: the British Society of Gastroenterology Initiative. J Clin Pathol. 1997; 50:93–105. PMID: 9155688.
Article84. Walsh AJ, Bryant RV, Travis SP. Current best practice for disease activity assessment in IBD. Nat Rev Gastroenterol Hepatol. 2016; 13:567–579. PMID: 27580684.
Article85. Ott JJ, Stevens GA, Groeger J, Wiersma ST. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine. 2012; 30:2212–2219. PMID: 22273662.
Article86. Rahier JF, Magro F, Abreu C, et al. Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2014; 8:443–468. PMID: 24613021.
Article87. Cheon JH. Understanding the complications of anti-tumor necrosis factor therapy in East Asian patients with inflammatory bowel disease. J Gastroenterol Hepatol. 2017; 32:769–777. PMID: 27723166.
Article88. Loras C, Gisbert JP, Mínguez M, et al. Liver dysfunction related to hepatitis B and C in patients with inflammatory bowel disease treated with immunosuppressive therapy. Gut. 2010; 59:1340–1346. PMID: 20577000.
Article89. Park SH, Yang SK, Lim YS, et al. Clinical courses of chronic hepatitis B virus infection and inflammatory bowel disease in patients with both diseases. Inflamm Bowel Dis. 2012; 18:2004–2010. PMID: 22337144.
Article90. Horsburgh CR Jr, Rubin EJ. Clinical practice: latent tuberculosis infection in the United States. N Engl J Med. 2011; 364:1441–1448. PMID: 21488766.91. Centers for Disease Control, R.O.C. (Taiwan). Tuberculosis diagnosis and treatment guidelines (version 5.1). Updated December 17, 2015. Accessed March 3, 2017. Web sitehttp://www.cdc.gov.tw/professional/info.aspx?treeid=beac9c103df952c4&nowtreeid=6744c19c09435458&tid=B02B73C3D6F15437.92. Summers RW, Switz DM, Sessions JT Jr, et al. National Cooperative Crohn's Disease Study: results of drug treatment. Gastroenterology. 1979; 77:847–869. PMID: 38176.
Article93. Malchow H, Ewe K, Brandes JW, et al. European cooperative Crohn's disease study (ECCDS): results of drug treatment. Gastroenterology. 1984; 86:249–266. PMID: 6140202.
Article94. Tremaine WJ, Schroeder KW, Harrison JM, Zinsmeister AR. A randomized, double-blind, placebo-controlled trial of the oral mesalamine (5-ASA) preparation, Asacol, in the treatment of symptomatic Crohn's colitis and ileocolitis. J Clin Gastroenterol. 1994; 19:278–282. PMID: 7876505.
Article95. Singleton JW, Hanauer SB, Gitnick GL, et al. Mesalamine capsules for the treatment of active Crohn's disease: results of a 16-week trial. Pentasa Crohn's Disease Study Group. Gastroenterology. 1993; 104:1293–1301. PMID: 8482443.
Article96. Lim WC, Wang Y, MacDonald JK, Hanauer S. Aminosalicylates for induction of remission or response in Crohn's disease. Cochrane Database Syst Rev. 2016; 7:CD008870. DOI: 10.1002/14651858.CD008870.pub2. PMID: 27372735.
Article97. Hanauer SB, Strömberg U. Oral Pentasa in the treatment of active Crohn's disease: a meta-analysis of double-blind, placebo-controlled trials. Clin Gastroenterol Hepatol. 2004; 2:379–388. PMID: 15118975.
Article98. Martin F, Sutherland L, Beck IT, et al. Oral 5-ASA versus prednisolone in short term treatment of Crohn's disease: a multicentre controlled trial. Can J Gastroenterol. 1990; 4:452–457.
Article99. Gross V, Andus T, Fischbach W, et al. Comparison between high dose 5-aminosalicylic acid and 6-methylprednisolone in active Crohn's ileocolitis: a multicenter randomized double-blind study. German 5-ASA Study Group. Z Gastroenterol. 1995; 33:581–584. PMID: 7502549.100. Prantera C, Cottone M, Pallone F, et al. Mesalamine in the treatment of mild to moderate active Crohn's ileitis: results of a randomized, multicenter trial. Gastroenterology. 1999; 116:521–526. PMID: 10029609.
Article101. Thomsen OO, Cortot A, Jewell D, et al. A comparison of budesonide and mesalamine for active Crohn's disease. International Budesonide-Mesalamine Study Group. N Engl J Med. 1998; 339:370–374. PMID: 9691103.
Article102. Rezaie A, Kuenzig ME, Benchimol EI, et al. Budesonide for induction of remission in Crohn's disease. Cochrane Database Syst Rev. 2015; (6):CD000296. DOI: 10.1002/14651858.CD000296.pub4. PMID: 26039678.
Article103. Benchimol EI, Seow CH, Steinhart AH, Griffiths AM. Traditional corticosteroids for induction of remission in Crohn's disease. Cochrane Database Syst Rev. 2008; (2):CD006792. DOI: 10.1002/14651858.CD006792.pub2. PMID: 18425970.
Article104. Steinhart AH, Ewe K, Griffiths AM, Modigliani R, Thomsen OO. Corticosteroids for maintenance of remission in Crohn's disease. Cochrane Database Syst Rev. 2003; (4):CD000301. DOI: 10.1002/14651858.CD000301. PMID: 14583917.
Article105. McDonald JW, Wang Y, Tsoulis DJ, MacDonald JK, Feagan BG. Methotrexate for induction of remission in refractory Crohn's disease. Cochrane Database Syst Rev. 2014; (8):CD003459. DOI: 10.1002/14651858.CD003459.pub4. PMID: 25099640.
Article106. Feagan BG, Rochon J, Fedorak RN, et al. Methotrexate for the treatment of Crohn's disease. The North American Crohn's Study Group Investigators. N Engl J Med. 1995; 332:292–297. PMID: 7816064.107. Targan SR, Hanauer SB, van Deventer SJ, et al. A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohn's disease. Crohn's Disease cA2 Study Group. N Engl J Med. 1997; 337:1029–1035. PMID: 9321530.
Article108. Schnitzler F, Fidder H, Ferrante M, et al. Long-term outcome of treatment with infliximab in 614 patients with Crohn's disease: results from a single-centre cohort. Gut. 2009; 58:492–500. PMID: 18832518.
Article109. Hanauer SB, Sandborn WJ, Rutgeerts P, et al. Human anti-tumor necrosis factor monoclonal antibody (adalimumab) in Crohn's disease: the CLASSIC-I trial. Gastroenterology. 2006; 130:323–333. PMID: 16472588.
Article110. Schreiber S, Rutgeerts P, Fedorak RN, et al. A randomized, placebo-controlled trial of certolizumab pegol (CDP870) for treatment of Crohn's disease. Gastroenterology. 2005; 129:807–818. PMID: 16143120.
Article111. Sandborn WJ, Feagan BG, Stoinov S, et al. Certolizumab pegol for the treatment of Crohn's disease. N Engl J Med. 2007; 357:228–238. PMID: 17634458.
Article112. Sandborn WJ, Rutgeerts P, Enns R, et al. Adalimumab induction therapy for Crohn disease previously treated with infliximab: a randomized trial. Ann Intern Med. 2007; 146:829–838. PMID: 17470824.
Article113. Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn's disease. N Engl J Med. 2013; 369:711–721. PMID: 23964933.
Article114. Sands BE, Feagan BG, Rutgeerts P, et al. Effects of vedolizumab induction therapy for patients with Crohn's disease in whom tumor necrosis factor antagonist treatment failed. Gastroenterology. 2014; 147:618–627. PMID: 24859203.
Article115. Sands BE, Sandborn WJ, Van Assche G, et al. Vedolizumab as induction and maintenance therapy for Crohn's disease in patients naïve to or who have failed tumor necrosis factor antagonist therapy. Inflamm Bowel Dis. 2017; 23:97–106. PMID: 27930408.
Article116. Feagan BG, Sandborn WJ, Gasink C, et al. Ustekinumab as induction and maintenance therapy for Crohn's disease. N Engl J Med. 2016; 375:1946–1960. PMID: 27959607.117. Chande N, Patton PH, Tsoulis DJ, Thomas BS, MacDonald JK. Azathioprine or 6-mercaptopurine for maintenance of remission in Crohn's disease. Cochrane Database Syst Rev. 2015; (10):CD000067. DOI: 10.1002/14651858.CD000067.pub3. PMID: 26517527.
Article118. Patel V, Wang Y, MacDonald JK, McDonald JW, Chande N. Methotrexate for maintenance of remission in Crohn's disease. Cochrane Database Syst Rev. 2014; (8):CD006884. DOI: 10.1002/14651858.CD006884.pub3. PMID: 25157445.
Article119. Peyrin-Biroulet L, Deltenre P, de Suray N, et al. Efficacy and safety of tumor necrosis factor antagonists in Crohn's disease: meta-analysis of placebo-controlled trials. Clin Gastroenterol Hepatol. 2008; 6:644–653. PMID: 18550004.
Article120. Behm BW, Bickston SJ. Tumor necrosis factor-alpha antibody for maintenance of remission in Crohn's disease. Cochrane Database Syst Rev. 2008; (1):CD006893. DOI: 10.1002/14651858.CD006893. PMID: 18254120.
Article121. Van Assche G, Magdelaine-Beuzelin C, D'Haens G, et al. Withdrawal of immunosuppression in Crohn's disease treated with scheduled infliximab maintenance: a randomized trial. Gastroenterology. 2008; 134:1861–1868. PMID: 18440315.
Article122. Matsumoto T, Motoya S, Watanabe K, et al. Adalimumab monotherapy and a combination with azathioprine for Crohn's disease: a prospective, randomized trial. J Crohns Colitis. 2016; 10:1259–1266. PMID: 27566367.
Article123. Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med. 2010; 362:1383–1395. PMID: 20393175.
Article124. Kruis W, Nguyen PG, Morgenstern J. Promises and dangers of combination therapy. Dig Dis. 2017; 35:56–60. PMID: 28147380.
Article125. Dignass A, Van Assche G, Lindsay JO, et al. The second European evidence-based consensus on the diagnosis and management of Crohn's disease: current management. J Crohns Colitis. 2010; 4:28–62. PMID: 21122489.
Article126. Aratari A, Papi C, Leandro G, Viscido A, Capurso L, Caprilli R. Early versus late surgery for ileo-caecal Crohn's disease. Aliment Pharmacol Ther. 2007; 26:1303–1312. PMID: 17848181.
Article127. Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013; 7:982–1018. PMID: 24184171.
Article128. Baert F, Moortgat L, Van Assche G, et al. Mucosal healing predicts sustained clinical remission in patients with early-stage Crohn's disease. Gastroenterology. 2010; 138:463–468. PMID: 19818785.
Article129. Hébuterne X, Lémann M, Bouhnik Y, et al. Endoscopic improvement of mucosal lesions in patients with moderate to severe ileocolonic Crohn's disease following treatment with certolizumab pegol. Gut. 2013; 62:201–208. PMID: 22525883.
Article130. Peyrin-Biroulet L, Reinisch W, Colombel JF, et al. Clinical disease activity, C-reactive protein normalisation and mucosal healing in Crohn's disease in the SONIC trial. Gut. 2014; 63:88–95. PMID: 23974954.
Article131. Rutgeerts P, Geboes K, Vantrappen G, Kerremans R, Coenegrachts JL, Coremans G. Natural history of recurrent Crohn's disease at the ileocolonic anastomosis after curative surgery. Gut. 1984; 25:665–672. PMID: 6735250.
Article132. Olaison G, Smedh K, Sjödahl R. Natural course of Crohn's disease after ileocolic resection: endoscopically visualised ileal ulcers preceding symptoms. Gut. 1992; 33:331–335. PMID: 1568651.
Article133. Tytgat GN, Mulder CJ, Brummelkamp WH. Endoscopic lesions in Crohn's disease early after ileocecal resection. Endoscopy. 1988; 20:260–262. PMID: 3168939.
Article134. Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn's disease. Gastroenterology. 1990; 99:956–963. PMID: 2394349.
Article135. Leighton JA, Shen B, Baron TH, et al. ASGE guideline: endoscopy in the diagnosis and treatment of inflammatory bowel disease. Gastrointest Endosc. 2006; 63:558–565. PMID: 16564852.
Article136. Fagan EA, Dyck RF, Maton PN, et al. Serum levels of C-reactive protein in Crohn's disease and ulcerative colitis. Eur J Clin Invest. 1982; 12:351–359. PMID: 6814926.
Article137. Yang DH, Yang SK, Park SH, et al. Usefulness of C-reactive protein as a disease activity marker in Crohn's disease according to the location of disease. Gut Liver. 2015; 9:80–86. PMID: 25170056.
Article138. Kiss LS, Papp M, Lovasz BD, et al. High-sensitivity C-reactive protein for identification of disease phenotype, active disease, and clinical relapses in Crohn's disease: a marker for patient classification? Inflamm Bowel Dis. 2012; 18:1647–1654. PMID: 22081542.
Article139. Bjarnason I, Sherwood R. Fecal calprotectin: a significant step in the noninvasive assessment of intestinal inflammation. J Pediatr Gastroenterol Nutr. 2001; 33:11–13. PMID: 11479401.
Article140. Summerton CB, Longlands MG, Wiener K, Shreeve DR. Faecal calprotectin: a marker of inflammation throughout the intestinal tract. Eur J Gastroenterol Hepatol. 2002; 14:841–845. PMID: 12172403.
Article141. Tibble JA, Sigthorsson G, Foster R, Forgacs I, Bjarnason I. Use of surrogate markers of inflammation and Rome criteria to distinguish organic from nonorganic intestinal disease. Gastroenterology. 2002; 123:450–460. PMID: 12145798.
Article142. Tibble J, Teahon K, Thjodleifsson B, et al. A simple method for assessing intestinal inflammation in Crohn's disease. Gut. 2000; 47:506–513. PMID: 10986210.
Article143. Lin WC, Wong JM, Tung CC, et al. Fecal calprotectin correlated with endoscopic remission for Asian inflammatory bowel disease patients. World J Gastroenterol. 2015; 21:13566–13573. PMID: 26730169.
Article144. Solem CA, Loftus EV Jr, Tremaine WJ, Harmsen WS, Zinsmeister AR, Sandborn WJ. Correlation of C-reactive protein with clinical, endoscopic, histologic, and radiographic activity in inflammatory bowel disease. Inflamm Bowel Dis. 2005; 11:707–712. PMID: 16043984.
Article145. Vermeire S, Van Assche G, Rutgeerts P. C-reactive protein as a marker for inflammatory bowel disease. Inflamm Bowel Dis. 2004; 10:661–665. PMID: 15472532.
Article146. Jürgens M, Mahachie John JM, Cleynen I, et al. Levels of Creactive protein are associated with response to infliximab therapy in patients with Crohn's disease. Clin Gastroenterol Hepatol. 2011; 9:421–427. PMID: 21334460.
Article147. Tibble JA, Sigthorsson G, Bridger S, Fagerhol MK, Bjarnason I. Surrogate markers of intestinal inflammation are predictive of relapse in patients with inflammatory bowel disease. Gastroenterology. 2000; 119:15–22. PMID: 10889150.
Article148. Ferreiro-Iglesias R, Barreiro-de Acosta M, Lorenzo-Gonzalez A, Dominguez-Muñoz JE. Accuracy of consecutive fecal calprotectin measurements to predict relapse in inflammatory bowel disease patients under maintenance with anti-tnf therapy: a prospective longitudinal cohort study. J Clin Gastroenterol. DOI: 10.1097/MCG.0000000000000774. [published onlineahead of print December 14, 2016].149. Sipponen T, Savilahti E, Kolho KL, Nuutinen H, Turunen U, Färkkilä M. Crohn's disease activity assessed by fecal calprotectin and lactoferrin: correlation with Crohn's disease activity index and endoscopic findings. Inflamm Bowel Dis. 2008; 14:40–46. PMID: 18022866.
Article150. Moreno N, Ripollés T, Paredes JM, et al. Usefulness of abdominal ultrasonography in the analysis of endoscopic activity in patients with Crohn's disease: changes following treatment with immunomodulators and/or anti-TNF antibodies. J Crohns Colitis. 2014; 8:1079–1087. PMID: 24613399.
Article151. Paredes JM, Ripollés T, Cortés X, et al. Abdominal sonographic changes after antibody to tumor necrosis factor (anti-TNF) alpha therapy in Crohn's Disease. Dig Dis Sci. 2010; 55:404–410. PMID: 19267199.
Article152. Deepak P, Fletcher JG, Fidler JL, Bruining DH. Computed tomography and magnetic resonance enterography in Crohn's disease: assessment of radiologic criteria and endpoints for clinical practice and trials. Inflamm Bowel Dis. 2016; 22:2280–2288. PMID: 27508513.
Article153. Rimola J, Rodriguez S, García-Bosch O, et al. Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn's disease. Gut. 2009; 58:1113–1120. PMID: 19136510.
Article154. Steward MJ, Punwani S, Proctor I, et al. Non-perforating small bowel Crohn's disease assessed by MRI enterography: derivation and histopathological validation of an MR-based activity index. Eur J Radiol. 2012; 81:2080–2088. PMID: 21924572.
Article155. Makanyanga JC, Pendsé D, Dikaios N, et al. Evaluation of Crohn's disease activity: initial validation of a magnetic resonance enterography global score (MEGS) against faecal calprotectin. Eur Radiol. 2014; 24:277–287. PMID: 24026620.
Article156. Oussalah A, Laurent V, Bruot O, et al. Diffusion-weighted magnetic resonance without bowel preparation for detecting colonic inflammation in inflammatory bowel disease. Gut. 2010; 59:1056–1065. PMID: 20525970.
Article157. Baars JE, Nuij VJ, Oldenburg B, Kuipers EJ, van der Woude CJ. Majority of patients with inflammatory bowel disease in clinical remission have mucosal inflammation. Inflamm Bowel Dis. 2012; 18:1634–1640. PMID: 22069022.
Article158. Kim NK, Senagore AJ, Luchtefeld MA, et al. Long-term outcome after ileocecal resection for Crohn's disease. Am Surg. 1997; 63:627–633. PMID: 9202538.159. Weston LA, Roberts PL, Schoetz DJ Jr, Coller JA, Murray JJ, Rusin LC. Ileocolic resection for acute presentation of Crohn's disease of the ileum. Dis Colon Rectum. 1996; 39:841–846. PMID: 8756837.
Article160. Bass JA, Goldman J, Jackson MA, et al. Pediatric Crohn disease presenting as appendicitis: differentiating features from typical appendicitis. Eur J Pediatr Surg. 2012; 22:274–278. PMID: 22648194.
Article161. Hsu WF, Wu CS, Wu JM, Chung CS. Ileal Crohn's disease with perforation misdiagnosed as ruptured appendicitis: a case report. J Formos Med Assoc. 2013; 112:652–653. PMID: 23962876.
Article162. Han H, Kim H, Rehman A, Jang SM, Paik SS. Appendiceal Crohn's disease clinically presenting as acute appendicitis. World J Clin Cases. 2014; 2:888–892. PMID: 25516865.
Article163. Chachu KA, Osterman MT. How to diagnose and treat IBD mimics in the refractory IBD patient who does not have IBD. Inflamm Bowel Dis. 2016; 22:1262–1274. PMID: 26891261.
Article164. Goldstein NS, Leon-Armin C, Mani A. Crohn's colitis-like changes in sigmoid diverticulitis specimens is usually an idiosyncratic inflammatory response to the diverticulosis rather than Crohn's colitis. Am J Surg Pathol. 2000; 24:668–675. PMID: 10800985.
Article165. Mukherjee K, Rinker EB, Kressin MK, Tarpley JL, Muldoon RL. Small bowel diverticulitis masquerading as Crohn's disease. Am Surg. 2013; 79:E246–E248. PMID: 23815990.
Article166. Garcia JC, Persky SE, Bonis PA, Topazian M. Abscesses in Crohn's disease: outcome of medical versus surgical treatment. J Clin Gastroenterol. 2001; 32:409–412. PMID: 11319312.
Article167. Gervais DA, Hahn PF, O'Neill MJ, Mueller PR. Percutaneous abscess drainage in Crohn disease: technical success and short- and long-term outcomes during 14 years. Radiology. 2002; 222:645–651. PMID: 11867780.
Article168. Feagins LA, Holubar SD, Kane SV, Spechler SJ. Current strategies in the management of intra-abdominal abscesses in Crohn's disease. Clin Gastroenterol Hepatol. 2011; 9:842–850. PMID: 21679776.
Article169. Müller-Wille R, Iesalnieks I, Dornia C, et al. Influence of percutaneous abscess drainage on severe postoperative septic complications in patients with Crohn's disease. Int J Colorectal Dis. 2011; 26:769–774. PMID: 21286921.
Article170. Zerbib P, Koriche D, Truant S, et al. Pre-operative management is associated with low rate of post-operative morbidity in penetrating Crohn's disease. Aliment Pharmacol Ther. 2010; 32:459–465. PMID: 20497144.
Article171. Shen B, Patel S, Lian L. Natural history of Crohn's disease in patients who underwent intentional restorative proctocolectomy with ileal pouch-anal anastomosis. Aliment Pharmacol Ther. 2010; 31:745–753. PMID: 20047579.
Article172. Reese GE, Lovegrove RE, Tilney HS, et al. The effect of Crohn's disease on outcomes after restorative proctocolectomy. Dis Colon Rectum. 2007; 50:239–250. PMID: 17180251.
Article173. Aberra FN, Lewis JD, Hass D, Rombeau JL, Osborne B, Lichtenstein GR. Corticosteroids and immunomodulators: post-operative infectious complication risk in inflammatory bowel disease patients. Gastroenterology. 2003; 125:320–327. PMID: 12891531.
Article174. Tzivanakis A, Singh JC, Guy RJ, Travis SP, Mortensen NJ, George BD. Influence of risk factors on the safety of ileocolic anastomosis in Crohn's disease surgery. Dis Colon Rectum. 2012; 55:558–562. PMID: 22513434.
Article175. Yamamoto T, Allan RN, Keighley MR. Risk factors for intra-abdominal sepsis after surgery in Crohn's disease. Dis Colon Rectum. 2000; 43:1141–1145. PMID: 10950014.
Article176. Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sandborn WJ, Loftus EV Jr. Surgery in a population-based cohort of Crohn's disease from Olmsted County, Minnesota (1970-2004). Am J Gastroenterol. 2012; 107:1693–1701. PMID: 22945286.
Article177. Reese GE, Nanidis T, Borysiewicz C, Yamamoto T, Orchard T, Tekkis PP. The effect of smoking after surgery for Crohn's disease: a meta-analysis of observational studies. Int J Colorectal Dis. 2008; 23:1213–1221. PMID: 18762954.
Article178. Van Assche G, Dignass A, Reinisch W, et al. The second European evidence-based consensus on the diagnosis and management of Crohn's disease: special situations. J Crohns Colitis. 2010; 4:63–101. PMID: 21122490.179. Caprilli R, Taddei G, Viscido A. In favour of prophylactic treatment for post-operative recurrence in Crohn's disease. Ital J Gastroenterol Hepatol. 1998; 30:219–225. PMID: 9675663.180. McLeod RS, Wolff BG, Steinhart AH, et al. Prophylactic mesalamine treatment decreases postoperative recurrence of Crohn's disease. Gastroenterology. 1995; 109:404–413. PMID: 7615189.
Article181. Carla-Moreau A, Paul S, Roblin X, Genin C, Peyrin-Biroulet L. Prevention and treatment of postoperative Crohn's disease recurrence with anti-TNF therapy: a meta-analysis of controlled trials. Dig Liver Dis. 2015; 47:191–196. PMID: 25488057.
Article182. Coelho J, Beaugerie L, Colombel JF, et al. Pregnancy outcome in patients with inflammatory bowel disease treated with thiopurines: cohort from the CESAME study. Gut. 2011; 60:198–203. PMID: 21115547.
Article183. Alstead EM, Ritchie JK, Lennard-Jones JE, Farthing MJ, Clark ML. Safety of azathioprine in pregnancy in inflammatory bowel disease. Gastroenterology. 1990; 99:443–446. PMID: 2365192.
Article184. Francella A, Dyan A, Bodian C, Rubin P, Chapman M, Present DH. The safety of 6-mercaptopurine for childbearing patients with inflammatory bowel disease: a retrospective cohort study. Gastroenterology. 2003; 124:9–17. PMID: 12512024.
Article185. Nørgård B, Pedersen L, Fonager K, Rasmussen SN, Sørensen HT. Azathioprine, mercaptopurine and birth outcome: a population-based cohort study. Aliment Pharmacol Ther. 2003; 17:827–834. PMID: 12641505.
Article186. Mahadevan U, Kane S, Sandborn WJ, et al. Intentional infliximab use during pregnancy for induction or maintenance of remission in Crohn's disease. Aliment Pharmacol Ther. 2005; 21:733–738. PMID: 15771759.
Article187. Katz JA, Antoni C, Keenan GF, Smith DE, Jacobs SJ, Lichtenstein GR. Outcome of pregnancy in women receiving infliximab for the treatment of Crohn's disease and rheumatoid arthritis. Am J Gastroenterol. 2004; 99:2385–2392. PMID: 15571587.
Article188. Vesga L, Terdiman JP, Mahadevan U. Adalimumab use in pregnancy. Gut. 2005; 54:890.
Article189. Mishkin DS, Van Deinse W, Becker JM, Farraye FA. Successful use of adalimumab (Humira) for Crohn's disease in pregnancy. Inflamm Bowel Dis. 2006; 12:827–828. PMID: 16917239.
Article190. Coburn LA, Wise PE, Schwartz DA. The successful use of adalimumab to treat active Crohn's disease of an ileoanal pouch during pregnancy. Dig Dis Sci. 2006; 51:2045–2047. PMID: 17009112.
Article191. Rahimi R, Nikfar S, Rezaie A, Abdollahi M. Pregnancy outcome in women with inflammatory bowel disease following exposure to 5-aminosalicylic acid drugs: a meta-analysis. Reprod Toxicol. 2008; 25:271–275. PMID: 18242053.
Article192. Silverman DA, Ford J, Shaw I, Probert CS. Is mesalazine really safe for use in breastfeeding mothers? Gut. 2005; 54:170–171.
Article193. Ost L, Wettrell G, Björkhem I, Rane A. Prednisolone excretion in human milk. J Pediatr. 1985; 106:1008–1011. PMID: 3998938.
Article194. Gardiner SJ, Gearry RB, Roberts RL, Zhang M, Barclay ML, Begg EJ. Exposure to thiopurine drugs through breast milk is low based on metabolite concentrations in mother-infant pairs. Br J Clin Pharmacol. 2006; 62:453–456. PMID: 16995866.
Article195. Mottet C, Juillerat P, Pittet V, et al. Pregnancy and breastfeeding in patients with Crohn's disease. Digestion. 2007; 76:149–160. PMID: 18239407.
Article196. Barclay AR, Russell RK, Wilson ML, Gilmour WH, Satsangi J, Wilson DC. Systematic review: the role of breastfeeding in the development of pediatric inflammatory bowel disease. J Pediatr. 2009; 155:421–426. PMID: 19464699.
Article197. Ruemmele FM, Veres G, Kolho KL, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn's disease. J Crohns Colitis. 2014; 8:1179–1207. PMID: 24909831.198. Byron MA, Jackson J, Ansell BM. Effect of different corticosteroid regimens on hypothalamic-pituitary-adrenal axis and growth in juvenile chronic arthritis. J R Soc Med. 1983; 76:452–457. PMID: 6864717.
Article199. Markowitz J, Grancher K, Kohn N, Lesser M, Daum F. A multicenter trial of 6-mercaptopurine and prednisone in children with newly diagnosed Crohn's disease. Gastroenterology. 2000; 119:895–902. PMID: 11040176.
Article200. Jaspers GJ, Verkade HJ, Escher JC, de Ridder L, Taminiau JA, Rings EH. Azathioprine maintains first remission in newly diagnosed pediatric Crohn's disease. Inflamm Bowel Dis. 2006; 12:831–836. PMID: 16954801.
Article201. Fuentes D, Torrente F, Keady S, et al. High-dose azathioprine in children with inflammatory bowel disease. Aliment Pharmacol Ther. 2003; 17:913–921. PMID: 12656694.
Article202. Turner D, Grossman AB, Rosh J, et al. Methotrexate following unsuccessful thiopurine therapy in pediatric Crohn's disease. Am J Gastroenterol. 2007; 102:2804–2812. PMID: 18042110.
Article203. Hyams J, Crandall W, Kugathasan S, et al. Induction and maintenance infliximab therapy for the treatment of moderateto-severe Crohn's disease in children. Gastroenterology. 2007; 132:863–873. PMID: 17324398.
Article204. Ruemmele FM, Lachaux A, Cézard JP, et al. Efficacy of infliximab in pediatric Crohn's disease: a randomized multicenter open-label trial comparing scheduled to on demand maintenance therapy. Inflamm Bowel Dis. 2009; 15:388–394. PMID: 19023899.
Article205. Hyams JS, Griffiths A, Markowitz J, et al. Safety and efficacy of adalimumab for moderate to severe Crohn's disease in children. Gastroenterology. 2012; 143:365–374. PMID: 22562021.
Article206. Hyams JS, Lerer T, Griffiths A, et al. Long-term outcome of maintenance infliximab therapy in children with Crohn's disease. Inflamm Bowel Dis. 2009; 15:816–822. PMID: 19107783.
Article207. Smith R, Hicks D, Tomljanovich PI, Lele SB, Rajput A, Dunn KB. Adenocarcinoma arising from chronic perianal Crohn's disease: case report and review of the literature. Am Surg. 2008; 74:59–61. PMID: 18274431.
Article208. Shwaartz C, Munger JA, Deliz JR, et al. Fistula-associated anorectal cancer in the setting of Crohn's disease. Dis Colon Rectum. 2016; 59:1168–1173. PMID: 27824702.
Article209. Laukoetter MG, Mennigen R, Hannig CM, et al. Intestinal cancer risk in Crohn's disease: a meta-analysis. J Gastrointest Surg. 2011; 15:576–583. PMID: 21152994.
Article210. Winkler R, Wittmer A, Heusermann U. Cancer and Crohn's disease. Z Gastroenterol. 2002; 40:569–576. PMID: 12297980.211. Thomas M, Bienkowski R, Vandermeer TJ, Trostle D, Cagir B. Malignant transformation in perianal fistulas of Crohn's disease: a systematic review of literature. J Gastrointest Surg. 2010; 14:66–73. PMID: 19826882.
Article212. Annese V, Beaugerie L, Egan L, et al. European evidence-based consensus: inflammatory bowel disease and malignancies. J Crohns Colitis. 2015; 9:945–965. PMID: 26294789.
Article213. Elriz K, Carrat F, Carbonnel F, et al. Incidence, presentation, and prognosis of small bowel adenocarcinoma in patients with small bowel Crohn's disease: a prospective observational study. Inflamm Bowel Dis. 2013; 19:1823–1826. PMID: 23702807.214. Biancone L, Zuzzi S, Ranieri M, et al. Fistulizing pattern in Crohn's disease and pancolitis in ulcerative colitis are independent risk factors for cancer: a single-center cohort study. J Crohns Colitis. 2012; 6:578–587. PMID: 22398047.
Article215. Jess T, Horváth-Puhó E, Fallingborg J, Rasmussen HH, Jacobsen BA. Cancer risk in inflammatory bowel disease according to patient phenotype and treatment: a Danish populationbased cohort study. Am J Gastroenterol. 2013; 108:1869–1876. PMID: 23978954.
Article216. Long MD, Herfarth HH, Pipkin CA, Porter CQ, Sandler RS, Kappelman MD. Increased risk for non-melanoma skin cancer in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2010; 8:268–274. PMID: 20005977.217. Singh H, Nugent Z, Demers AA, Bernstein CN. Increased risk of nonmelanoma skin cancers among individuals with inflammatory bowel disease. Gastroenterology. 2011; 141:1612–1620. PMID: 21806945.
Article218. Kotlyar DS, Lewis JD, Beaugerie L, et al. Risk of lymphoma in patients with inflammatory bowel disease treated with azathioprine and 6-mercaptopurine: a meta-analysis. Clin Gastroenterol Hepatol. 2015; 13:847–858. PMID: 24879926.
Article219. Kotlyar DS, Osterman MT, Diamond RH, et al. A systematic review of factors that contribute to hepatosplenic T-cell lymphoma in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2011; 9:36–41. PMID: 20888436.
Article220. Ariyaratnam J, Subramanian V. Association between thiopurine use and nonmelanoma skin cancers in patients with inflammatory bowel disease: a meta-analysis. Am J Gastroenterol. 2014; 109:163–169. PMID: 24419479.
Article221. Long MD, Martin CF, Pipkin CA, Herfarth HH, Sandler RS, Kappelman MD. Risk of melanoma and nonmelanoma skin cancer among patients with inflammatory bowel disease. Gastroenterology. 2012; 143:390–399. PMID: 22584081.
Article222. Peyrin-Biroulet L, Khosrotehrani K, Carrat F, et al. Increased risk for nonmelanoma skin cancers in patients who receive thiopurines for inflammatory bowel disease. Gastroenterology. 2011; 141:1621–1628. PMID: 21708105.
Article223. Rieder F, Latella G, Magro F, et al. European Crohn's and colitis organisation topical review on prediction, diagnosis and management of fibrostenosing Crohn's disease. J Crohns Colitis. 2016; 10:873–885. PMID: 26928961.
Article224. Spinelli A, Correale C, Szabo H, Montorsi M. Intestinal fibrosis in Crohn's disease: medical treatment or surgery? Curr Drug Targets. 2010; 11:242–248. PMID: 19916949.
Article225. Van Assche G, Geboes K, Rutgeerts P. Medical therapy for Crohn's disease strictures. Inflamm Bowel Dis. 2004; 10:55–60. PMID: 15058528.
Article226. Bettenworth D, Gustavsson A, Atreja A, et al. A pooled analysis of efficacy, safety, and long-term outcome of endoscopic balloon dilation therapy for patients with stricturing Crohn's disease. Inflamm Bowel Dis. 2017; 23:133–142. PMID: 28002130.227. Bemelman WA, Allez M. The surgical intervention: earlier or never? Best Pract Res Clin Gastroenterol. 2014; 28:497–503. PMID: 24913388.228. Latella G, Cocco A, Angelucci E, et al. Clinical course of Crohn's disease first diagnosed at surgery for acute abdomen. Dig Liver Dis. 2009; 41:269–276. PMID: 18955023.229. de Buck van Overstraeten A, Wolthuis A, D'Hoore A. Surgery for Crohn's disease in the era of biologicals: a reduced need or delayed verdict? World J Gastroenterol. 2012; 18:3828–3832. PMID: 22876034.230. Bobanga ID, Bai S, Swanson MA, et al. Factors influencing disease recurrence after ileocolic resection in adult and pediatric onset Crohn's disease. Am J Surg. 2014; 208:591–596. PMID: 25110291.
Article231. Yamazaki Y, Ribeiro MB, Sachar DB, Aufses AH Jr, Greenstein AJ. Malignant colorectal strictures in Crohn's disease. Am J Gastroenterol. 1991; 86:882–885. PMID: 2058631.232. Lovasz BD, Lakatos L, Golovics PA, et al. Risk of colorectal cancer in Crohn's disease patients with colonic involvement and stenosing disease in a population-based cohort from Hungary. J Gastrointestin Liver Dis. 2013; 22:265–268. PMID: 24078982.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Seminar Report From the 2014 Taiwan Society of Inflammatory Bowel Disease (TSIBD) Spring Forum (May 24th, 2014): Crohn's Disease Versus Intestinal Tuberculosis Infection
- Balloon-Assisted Enteroscopy and Capsule Endoscopy in Suspected Small Bowel Crohn's Disease
- Chemoprevention of Colitis-Associated Dysplasia or Cancer in Inflammatory Bowel Disease
- An unusual cause of distal duodenal bleeding
- Should Asian inflammatory bowel disease patients need routine thromboprophylaxis?