J Educ Eval Health Prof.
2014;11:1. 10.3352/jeehp.2014.11.1.
Physical therapy students' perceptions of team-based learning in gross anatomy using the Team-Based Learning Student Assessment Instrument
- Affiliations
-
- 1Department of Clinical and Applied Movement Sciences, University of North Florida, Jacksonville, FL, USA. b.livingston@unf.edu
- 2Department of Physical Therapy, University of Florida, College of Public Health & Health Professions, Gainesville, FL, USA.
- KMID: 2380920
- DOI: http://doi.org/10.3352/jeehp.2014.11.1
Abstract
- PURPOSE
The objective of this study was to assess physical therapy student perceptions of team-based learning (TBL) in a graduate level gross anatomy course using the TBL Student Assessment Instrument (TBL-SAI).
METHODS
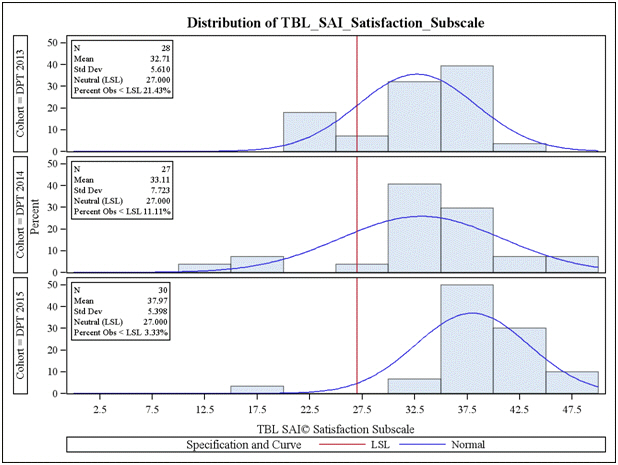
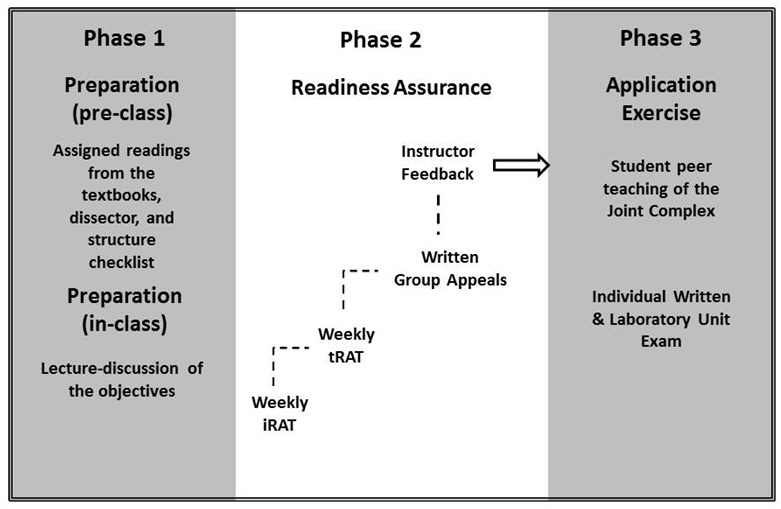
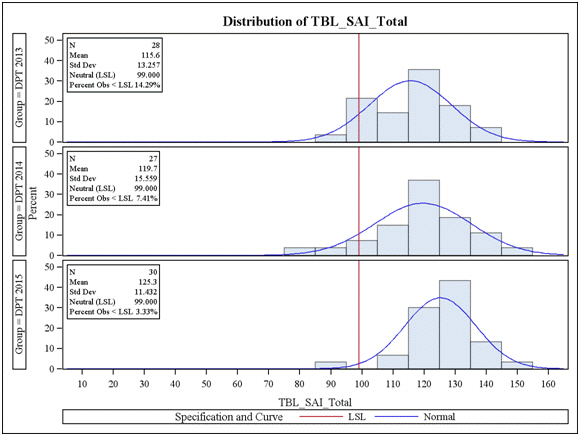
The TBL-SAI was administered to 85 doctor of physical therapy (DPT) students, comprising three cohorts (classes of 2013, 2014, and 2015), who successfully completed a gross anatomy course where TBL was implemented. The TBL-SAI surveys 33 items, each rated from one (strongly disagree) to five (strongly agree) and measures three subscales: students' perceptions of accountability, preference for lecture or TBL, and student satisfaction.
RESULTS
The means for each subscale and the total TBL-SAI score for each cohort fell above the neutral score. The 2015 group (mean, 37.97; 95% confidence interval [CI], 35.67 to 40.26) reported significantly higher satisfaction than that of the 2013 group (mean, 32.71; 95% CI, 30.31 to 35.05) and the 2014 group (mean, 33.11; 95% CI, 30.69 to 35.53). The 2015 group (mean, 125.3; 95% CI, 120.6 to 130.3) also had a significantly higher total score than that of the 2013 group (mean, 115.6; 95% CI, 110.5 to 120.5).
CONCLUSION
The physical therapy students reported an overall positive experience in using TBL to learn gross anatomy in terms of accountability, preference for learning mode, and satisfaction. This positive experience with TBL was accompanied by their successful academic performance. Given the traits and learning preferences in this generation of graduate students, TBL could be a teaching method that is received positively elsewhere and results in successful academic performance and learning.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Evaluation of team-based learning in a doctor of physical therapy curriculum in the United States
Donald H. Lein, John D. Lowman, Christopher A. Eidson, Hon K. Yuen, Sun Huh
J Educ Eval Health Prof. 2017;14:3. doi: 10.3352/jeehp.2017.14.3.Perceptions of team-based learning using the Team-Based Learning Student Assessment Instrument: an exploratory analysis amongst pharmacy and biomedical students in the United Kingdom
Prabha Parthasarathy, Bugewa Apampa, Andrea Manfrin, Sun Huh
J Educ Eval Health Prof. 2019;16:23. doi: 10.3352/jeehp.2019.16.23.
Reference
-
1. Michaelsen LK, Sweet M. The essential elements of team-based learning. New Dir Teach Learn. 2008; 2008:7–27. http://dx.doi.org/10.1002/tl.330.
Article2. Haidet P, O'Malley KJ, Richards B. An initial experience with "team learning" in medical education. Acad Med. 2002; 77:40–44.
Article3. McInerney MJ, Fink LD. Team-based learning enhances long-term retention and critical thinking in an undergraduate microbial physiology course. Microbiol Educ. 2003; 4:3–12.
Article4. Thompson BM, Schneider VF, Levine RE, McMahon KK, Perkowski LC, Richards BF. Team-based learning at ten medical schools: two years later. Med Educ. 2007; 41:250–257. http://dx.doi.org/ 10.1111/j.1365-2929.2006.02684.x.
Article5. Vasan NS, DeFouw DO, Compton S. A survey of student perceptions of team-based learning in anatomy curriculum: Favorable views unrelated to grades. Anat Sci Educ. 2009; 2:150–155. http://dx.doi.org/10.1002/ase.91.
Article6. Perskyy AM. The impact of team-based learning on a foundational pharmacokinetics course. Am J Pharm Educ. 2012; 76:31. http://dx.doi.org/10.5688/ajpe76231.7. Searle NS, Haidet P, Kelly PA, Schneider VF, Seidel CL, Richards BF. Team learning in medical education: Initial experiences at ten institutions. Acad Med. 2003; 78(10 suppl):S55–S58.
Article8. Mangold K. Educating a new generation: teaching baby boomer faculty about millennial students. Nurse Educ. 2007; 32:21–23.9. Wilson M, Gerber L. How generational theory can improve teaching: strategies for working with the millennials. Curr Teach Learn. 2008; 1:29–44.10. Tohmatsu DT. Who are the millennials? a.k.a. generation y [Internet]. Deloitte Development LLC; 2008 [cited 2013 Sep 9]. Available from http://www.deloitte.com/assets/Dcom-UnitedStates/Local%20Assets/Documents/us_consulting_hc_millennials_110608.pdf.11. Billings D. Teaching learners from varied generations. J Contin Educ Nurs. 2004; 35:104–105.
Article12. Tai BC, Koh WP. Does team learning motivate students' engagement in an evidence-based medicine course? Ann Acad Med Singapore. 2008; 37:1019–1023.13. Tan NC, Kandiah N, Chan YH, Umapathi T, Lee SH, Tan K. A controlled study of team-based learning for undergraduate clinical neurology education. BMC Med Educ. 2011; 11:91. http://dx.doi.org/10.1186/1472-6920-11-91.
Article14. Shankar N, Roopa R. Evaluation of a modified team based learning method for teaching general embryology to 1st year medical graduate students. Indian J Med Sci. 2009; 63:4–12. http://dx.doi.org/10.4103/0019-5359.49076.15. Kelly PA, Haidet P, Schneider V, Searle N, Seidel CL, Richards BF. A comparison of in-class learner engagement across lecture, problem-based learning, and team learning using the STROBE classroom observation tool. Teach Learn Med. 2005; 17:112–118. http://dx.doi.org/10.1207/s15328015tlm1702_4.
Article16. Addo-Atuah J. Performance and perceptions of pharmacy students using team-based learning (TBL) within a global health course. Inov Pharm. 2011; 2:37.
Article17. Mennenga HA. Development and psychometric testing of the team-based learning student assessment instrument. Nurse Educ. 2012; 37:168–172. http://dx.doi.org/10.1097/NNE.0b013e31825a87cc.
Article18. Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. Baltimore, MD: Lippincott Williams & Wilkins;2010.19. Netter FH. Atlas of human anatomy. Philadelphia, PA: Sauders Elesevier;2011.20. Senesac CR, Bishop M. Finley's interactive cadaveric dissection guide. Sudbury, MA: Jones and Bartlett;2010.21. Hofer RE, Nikolaus OB, Pawlina W. Using checklists in a gross anatomy laboratory improves learning outcomes and dissection quality. Anat Sci Educ. 2011; 4:249–255. http://dx.doi.org/10.1002/ase.243.
Article22. Latman NS, Lanier R. Gross anatomy course content and teaching methodology in allied health: clinicians' experiences and recommendations. Clin Anat. 2001; 14:152–157. http://dx.doi.org/10.1002/1098-2353(200103).
Article23. Kuh G. What we're learning about student engagement from NSSE: benchmarks for effective educational practices. Change. 2003; 35:24–32. http://dx.doi.org/10.1080/00091380309604090.
Article24. Kraska M. Retention of graduate students through learning communities. J Ind Teach Educ. 2008; 45:54–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Student Team Achievement Division as a tool for peer assisted co-operative learning in neuroanatomy
- Assessment of students' satisfaction with a student-led team-based learning course
- Perceptions of team-based learning using the Team-Based Learning Student Assessment Instrument: an exploratory analysis amongst pharmacy and biomedical students in the United Kingdom
- The applicability of a validated team-based learning student assessment instrument to assess United Kingdom pharmacy students' attitude toward team-based learning
- Effect on Problem-Based Learning with Simulation in Nursing Student According to Team Activity Satisfaction: Self-Directed Learning Ability, Communication Apprehension