Obstet Gynecol Sci.
2017 May;60(3):296-302. 10.5468/ogs.2017.60.3.296.
Analysis of surgeries performed after hysteroscopic sterilization as tabulated from 3,803 Essure patient experiences
- Affiliations
-
- 1Center for Advanced Genetics, Carlsbad, CA, USA. drsills@CAGivf.com
- 2Department of Obstetrics and Gynecology, Palomar Medical Center, Escondido, CA, USA.
- 3Reproductive Sciences Medical Center, San Diego, CA, USA.
- 4Progenesis, Inc., La Jolla, CA, USA.
- 5Department of Surgery, University of Vermont College of Medicine, Burlington, VT, USA.
- KMID: 2378592
- DOI: http://doi.org/10.5468/ogs.2017.60.3.296
Abstract
OBJECTIVE
Although previous research has suggested that risk for reoperation among hysteroscopic sterilization (HS) patients is more than ten times higher than for patients undergoing standard laparoscopic tubal ligation, little has been reported about these subsequent procedures.
METHODS
This descriptive cohort study used a confidential online questionnaire to gather data from women (n=3,803) who volunteered information on HS followed by device removal surgery performed due to new symptoms developing after Essure placement.
RESULTS
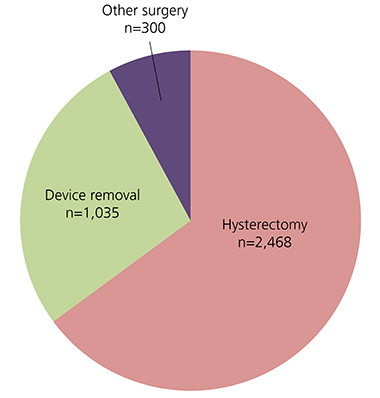
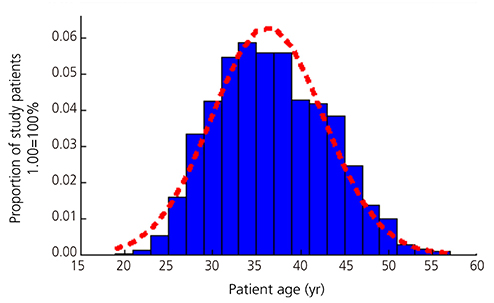
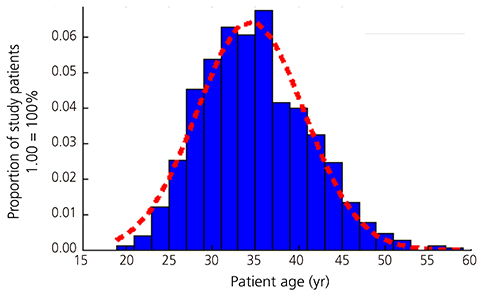
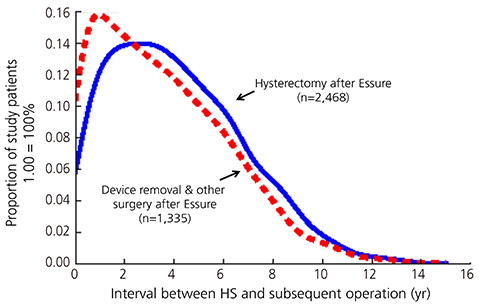
In this sample, mean age was 35.6 years and women undergoing hysterectomy after HS comprised 64.9% (n=2,468). Median interval between HS and hysterectomy was 3.7 (interquartile range, 3.9) years and mean age at hysterectomy was 36.3 years. Some patients (n=1,035) sought removal of HS devices and fallopian tubes only, while other miscellaneous gynecological procedures were also occasionally performed for Essure-associated symptoms. When data from all patients who had any post-Essure surgery besides hysterectomy were aggregated (e.g., device removal +"other" cases, n=1,335) and compared to those cases undergoing hysterectomy, mean age was significantly lower than for the hysterectomy group (34.4 vs. 36.3 years, respectively; P<0.01); uterus-conserving surgeries were also typically performed significantly earlier than hysterectomy (P<0.01).
CONCLUSION
This investigation is the first to characterize specific gynecological operations after Essure, and suggests that the predominant surgical answer to HS complaints is hysterectomy for many women. Dissatisfaction with HS may represent an important indication for hysterectomy and additional study is needed to quantify this phenomenon.
Keyword
MeSH Terms
Figure
Reference
-
1. Mino M, Arjona JE, Cordon J, Pelegrin B, Povedano B, Chacon E. Success rate and patient satisfaction with the Essure sterilisation in an outpatient setting: a prospective study of 857 women. BJOG. 2007; 114:763–766.2. Thiel JA, Carson GD. Cost-effectiveness analysis comparing the essure tubal sterilization procedure and laparoscopic tubal sterilization. J Obstet Gynaecol Can. 2008; 30:581–585.3. Levie MD, Chudnoff SG. Office hysteroscopic sterilization compared with laparoscopic sterilization: a critical cost analysis. J Minim Invasive Gynecol. 2005; 12:318–322.4. Rezai S, LaBine M, Gomez Roberts HA, Lora Alcantara I, Henderson CE, Elmadjian M, et al. Essure microinsert abdominal migration after hysteroscopic tubal sterilization of an appropriately placed essure device: dual case reports and review of the literature. Case Rep Obstet Gynecol. 2015; 2015:402197.5. Sills ES, Dalton MM. Referrals for complications following hysteroscopic sterilisation: characteristics associated with symptomatic patients after the Essure procedure. Eur J Contracept Reprod Health Care. 2016; 21:227–233.6. US Food and Drug Administration. MAUDE adverse event report: Bayer Pharma AG Essure insert, tubal occlusion [Internet]. Silver Spring (MD): US Food and Drug Administration;2015. cited 2016 Jun 28. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/detail.cfm?mdrfoi__id=4531887.7. Scarabin C, Dhainaut C. The ESTHYME study. Women's satisfaction after hysteroscopic sterilization (Essure micro-insert). A retrospective multicenter survey. Gynecol Obstet Fertil. 2007; 35:1123–1128.8. Brito LG, Cohen SL, Goggins ER, Wang KC, Einarsson JI. Essure surgical removal and subsequent symptom resolution: case series and follow-up survey. J Minim Invasive Gynecol. 2015; 22:910–913.9. Rudulph HW. The controversial birth control you've never heard of [Internet]. New York (NY): Cosmopolitan;2014. cited 2016 Jun 28. Available from: http://www.cosmopolitan.com/lifestyle/news/a18925/essure-birth-control-controversy.10. Klimas L. Hundreds of women forced to have hysterectomies after reaction to permanent birth control implant [Internet]. [place unknown]: The Blaze;2013. cited 2016 Jun 28. Available from: http://www.theblaze.com/stories/2013/11/13/hundreds-of-women-forced-to-have-hysterectomies-after-reaction-to-permanent-birth-control-implant.11. Doll KM, Dusetzina SB, Robinson W. Trends in inpatient and outpatient hysterectomy and oophorectomy rates among commercially insured women in the United States, 2000-2014. JAMA Surg. 2016; 151:876–877.12. Whiteman MK, Hillis SD, Jamieson DJ, Morrow B, Podgornik MN, Brett KM, et al. Inpatient hysterectomy surveillance in the United States, 2000-2004. Am J Obstet Gynecol. 2008; 198:34.13. Anderson TL, Yunker AC, Scheib SA, Callahan TL. Hysteroscopic sterilization success in outpatient vs office setting is not affected by patient or procedural characteristics. J Minim Invasive Gynecol. 2013; 20:858–863.14. Howard DL, Wall J, Strickland JL. What are the factors predictive of hysterosalpingogram compliance after female sterilization by the Essure procedure in a publicly insured population? Matern Child Health J. 2013; 17:1760–1767.15. Sills ES, Li X, Jones CA, Wood SH. Contraceptive failure after hysteroscopic sterilization: analysis of clinical and demographic data from 103 unplanned pregnancies. Obstet Gynecol Sci. 2015; 58:487–493.16. US Food and Drug Administration. FDA review document: review of the Essure system for hysteroscopic sterilization [Internet]. Silver Spring (MD): US Food and Drug Administration;2015. cited 2015 Jun 28. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/ObstetricsandGynecologyDevices/UCM463486.pdf.17. Adelman MR, Dassel MW, Sharp HT. Management of complications encountered with Essure hysteroscopic sterilization: a systematic review. J Minim Invasive Gynecol. 2014; 21:733–743.18. Mao J, Pfeifer S, Schlegel P, Sedrakyan A. Safety and efficacy of hysteroscopic sterilization compared with laparoscopic sterilization: an observational cohort study. BMJ. 2015; 351:h5162.19. Albright CM, Frishman GN, Bhagavath B. Surgical aspects of removal of Essure microinsert. Contraception. 2013; 88:334–336.20. Lannon BM, Lee SY. Techniques for removal of the Essure hysteroscopic tubal occlusion device. Fertil Steril. 2007; 88:497.21. Kraemer DF, Yen PY, Nichols M. An economic comparison of female sterilization of hysteroscopic tubal occlusion with laparoscopic bilateral tubal ligation. Contraception. 2009; 80:254–260.22. Dhruva SS, Ross JS, Gariepy AM. Revisiting Essure: toward safe and effective sterilization. N Engl J Med. 2015; 373:e17.23. la Chapelle CF, Veersema S, Brolmann HA, Jansen FW. Effectiveness and feasibility of hysteroscopic sterilization techniques: a systematic review and meta-analysis. Fertil Steril. 2015; 103:1516–1525.24. Hoyos LR, Leon-Peters J, Berman JM, Hertz M. Pregnancy following hysteroscopic sterilization at an Urban Abortion Clinic. A case series: are we looking in the wrong places? Contraception. 2016; 94:78–80.25. Sills ES, Fernandez LP, Jones CA. What is the economic cost of unplanned pregnancy following hysteroscopic sterilization in the US? A new national estimate based on Essure procedure prevalence, failure rates, and workforce productivity. World Health Popul. 2016; 17:31–38.26. Kulseng-Hanssen S, Borstad E. The development of a questionnaire to measure the severity of symptoms and the quality of life before and after surgery for stress incontinence. BJOG. 2003; 110:983–988.27. Larochelle A, Podoba J, Ouellet S, Fraser WD. Accuracy of recall in quality-of-life assessment among women operated on for stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20:1233–1241.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endometrial fluid associated with Essure implants placed before in vitro fertilization: Considerations for patient counseling and surgical management
- Contraceptive failure after hysteroscopic sterilization: Analysis of clinical and demographic data from 103 unplanned pregnancies
- Combined hysteroscopy-laparoscopy approach for excision of pelvic nitinol fragment from Essure contraceptive device: Role of intraoperative fluoroscopy for uterine conservation
- Studies on Male Sterilization
- Hysteroscopic Tubal Catheterization for Treatment of Infertility with Proximal Tubal Occlusion