Obstet Gynecol Sci.
2016 Jul;59(4):337-341. 10.5468/ogs.2016.59.4.337.
Combined hysteroscopy-laparoscopy approach for excision of pelvic nitinol fragment from Essure contraceptive device: Role of intraoperative fluoroscopy for uterine conservation
- Affiliations
-
- 1Reproductive Research Section, Center for Advanced Genetics, Carlsbad, CA, USA. drsills@CAGivf.com
- 2Department of Obstetrics and Gynecology, Saddleback Memorial Medical Center, Laguna Hills, CA, USA.
- 3Molecular and Applied Biosciences Department, Faculty of Science & Technology, University of Westminster, London, UK.
- 4Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine, Weill Cornell Medical College, New York, NY, USA.
- KMID: 2329059
- DOI: http://doi.org/10.5468/ogs.2016.59.4.337
Abstract
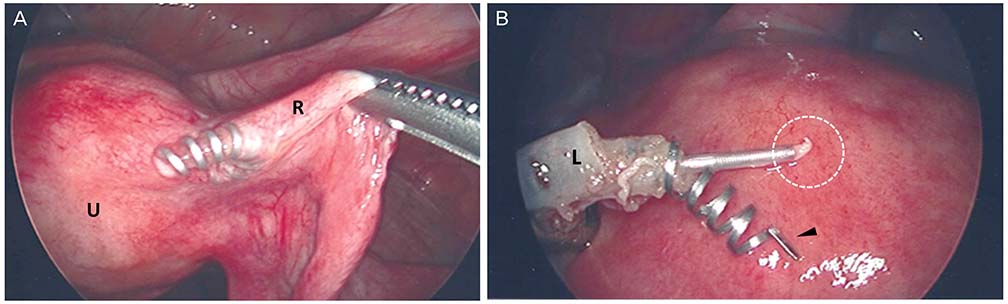
- We describe the successful removal of a pelvic contraceptive coil in a symptomatic 46-year-old patient who had Essure devices for four years, using a combined hysteroscopy-laparoscopy-fluoroscopy approach. Following normal hysteroscopy, at laparoscopy the right Essure implant was disrupted and its outer nitinol coil had perforated the fallopian tube. However, the inner rod (containing polyethylene terephthalate) had migrated to an extrapelvic location, near the proximal colon. In contrast, the left implant was situated within the corresponding tube. Intraoperative fluoroscopy was used to confirm complete removal of the device, which was further verified by postoperative computed tomography. The patient's condition improved after surgery and she continues to do well. This is the first report to describe this technique in managing Essure complications remote from time of insertion. Our case highlights the value and limitations of preoperative and intraoperative imaging to map Essure fragment location before surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Mao J, Pfeifer S, Schlegel P, Sedrakyan A. Safety and efficacy of hysteroscopic sterilization compared with laparoscopic sterilization: an observational cohort study. BMJ. 2015; 351:h5162.2. la Chapelle CF, Veersema S, Brolmann HA, Jansen FW. Effectiveness and feasibility of hysteroscopic sterilization techniques: a systematic review and meta-analysis. Fertil Steril. 2015; 103:1516–1525. 1525.e1–1525.e3.3. Sills ES, Walsh DJ, Jones CA, Wood SH. Endometrial fluid associated with Essure implants placed before in vitro fertilization: considerations for patient counseling and surgical management. Clin Exp Reprod Med. 2015; 42:126–129.4. Ricci G, Restaino S, Di Lorenzo G, Fanfani F, Scrimin F, Mangino FP. Risk of Essure microinsert abdominal migration: case report and review of literature. Ther Clin Risk Manag. 2014; 10:963–968.5. Rezai S, LaBine M, Gomez Roberts HA, Lora Alcantara I, Henderson CE, Elmadjian M, et al. Essure microinsert abdominal migration after hysteroscopic tubal sterilization of an appropriately placed Essure device: dual case reports and review of the literature. Case Rep Obstet Gynecol. 2015; 2015:402197.6. Braginsky L, George ST, Locher SR. Management of perforated essure with migration into small and large bowel mesentery. J Minim Invasive Gynecol. 2015; 22:504–508.7. Dhruva SS, Ross JS, Gariepy AM. Revisiting Essure: toward safe and effective sterilization. N Engl J Med. 2015; 373:e17.8. US Food and Drug Administration. MAUDE adverse event report: Bayer Healthcare LLC Essure device, occlusion, tubal, contraceptive [Internet]. Silver Spring (MD): US Food and Drug Administration;2015. cited 2015 Dec 15. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/detail.cfm?mdrfoi__id=4531887.9. Howard DL, Christenson PJ, Strickland JL. Use of intraoperative fluoroscopy during laparotomy to identify fragments of retained Essure microinserts: case report. J Minim Invasive Gynecol. 2012; 19:667–670.10. Guiahi M, Tocce K, Teal S, Green T, Rochon P. Removal of a Nexplanon implant located in the biceps muscle using a combination of ultrasound and fluoroscopy guidance. Contraception. 2014; 90:606–608.11. Guelfguat M, Gruenberg TR, Dipoce J, Hochsztein JG. Imaging of mechanical tubal occlusion devices and potential complications. Radiographics. 2012; 32:1659–1673.12. Nag S, Ciezki JP, Cormack R, Doggett S, DeWyngaert K, Edmundson GK, et al. Intraoperative planning and evaluation of permanent prostate brachytherapy: report of the American Brachytherapy Society. Int J Radiat Oncol Biol Phys. 2001; 51:1422–1430.13. Kuo N, Dehghan E, Deguet A, Mian OY, Le Y, Burdette EC, et al. An image-guidance system for dynamic dose calculation in prostate brachytherapy using ultrasound and fluoroscopy. Med Phys. 2014; 41:091712.14. Daly MJ, Siewerdsen JH, Moseley DJ, Jaffray DA, Irish JC. Intraoperative cone-beam CT for guidance of head and neck surgery: assessment of dose and image quality using a C-arm prototype. Med Phys. 2006; 33:3767–3780.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endometrial fluid associated with Essure implants placed before in vitro fertilization: Considerations for patient counseling and surgical management
- Ureteral Obstruction Caused by Pelvic Actinomycosis
- A case of displacement of intrauterine device into abdominal cavity by uterine perforation in early pregnancy
- Gas Embolism during Diagnostic Laparoscopy Combined with Hysteroscopic Procedure: A case report
- Laparoscopic Removal of an Intrauterine Contraceptive Device That Had Migrated into the Intraabdominal Cavity