J Korean Soc Radiol.
2017 May;76(5):363-368. 10.3348/jksr.2017.76.5.363.
Hemorrhagic Listerial Encephalitis in a Patient with Systemic Lupus Erythematosus: A Case Report
- Affiliations
-
- 1Department of Radiology, Hanyang University Hospital, Hanyang University College of Medicine, Seoul, Korea. jyjy133@naver.com
- 2Department of Neurology, Hanyang University Hospital, Hanyang University College of Medicine, Seoul, Korea. aescula@hanmail.net
- 3Department of Radiology, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea.
- KMID: 2377041
- DOI: http://doi.org/10.3348/jksr.2017.76.5.363
Abstract
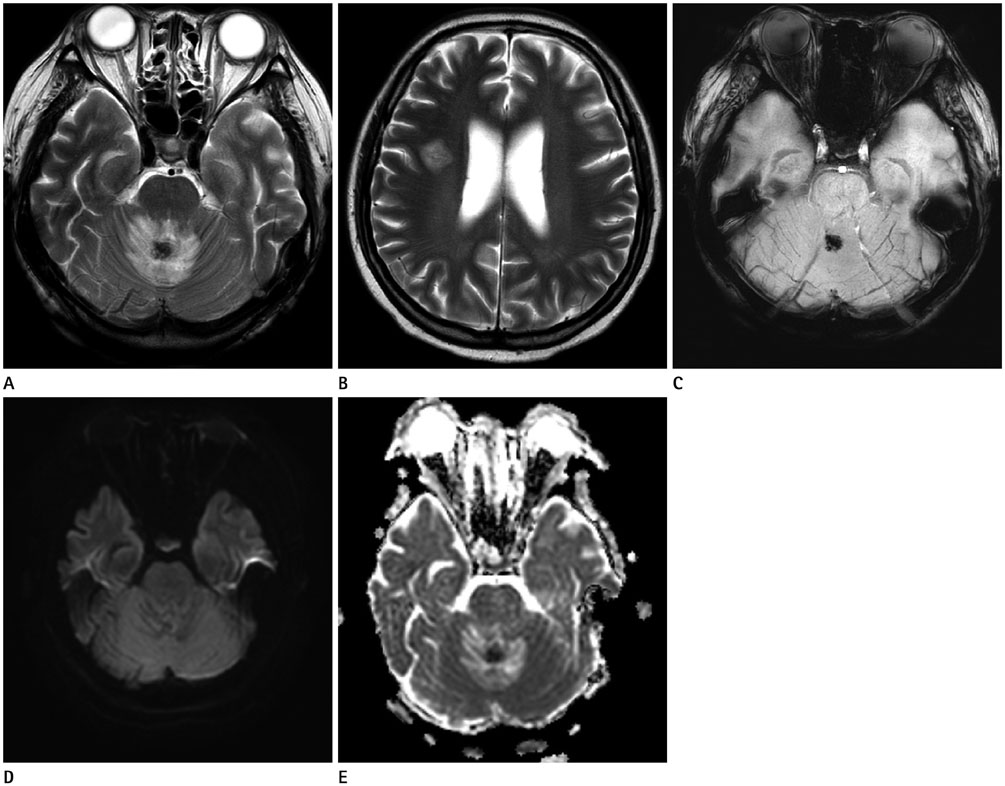
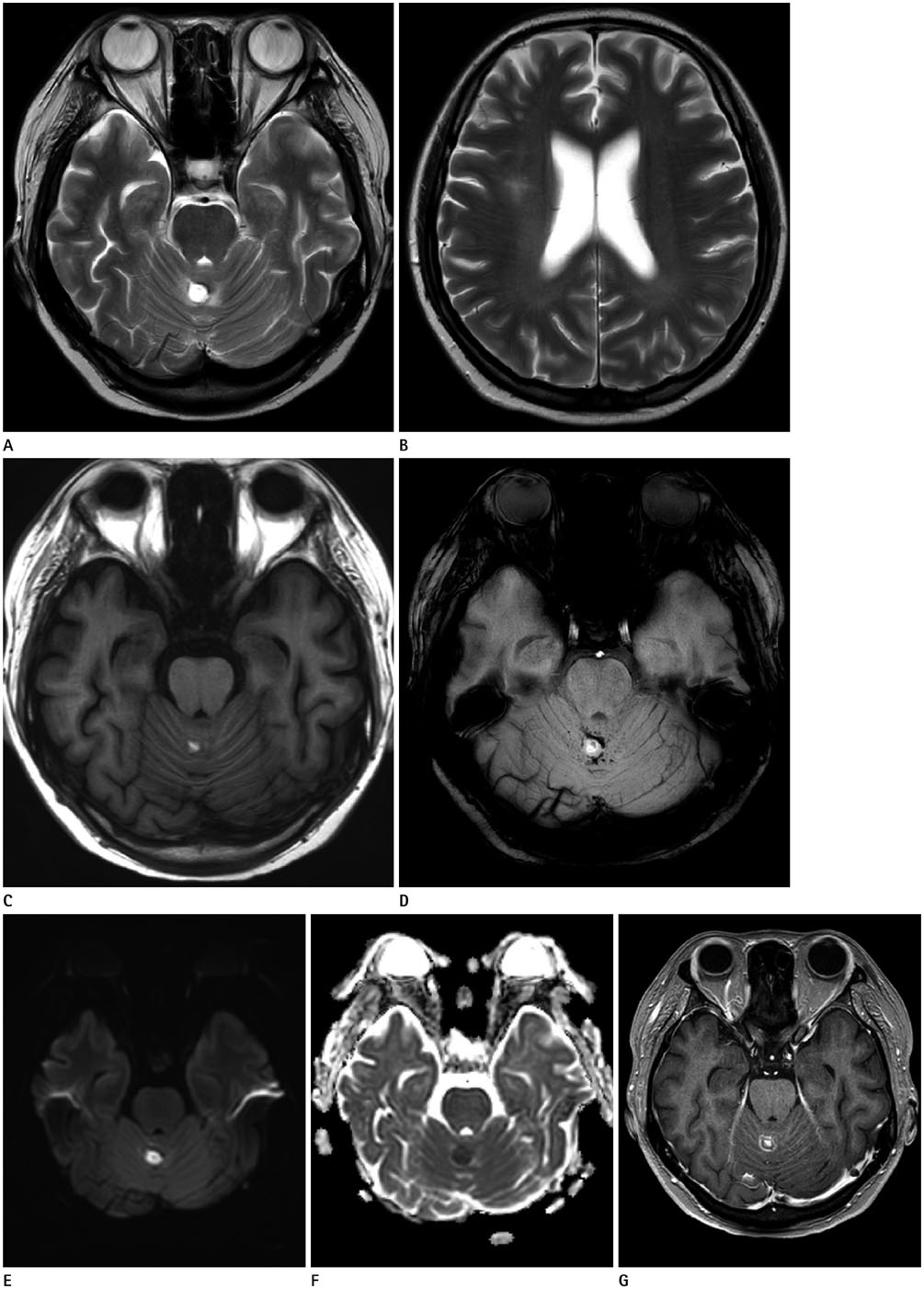
- A 31-year-old female with systemic lupus erythematosus (SLE) presented with fever, headache, seizures and mental status changes. Brain MRI showed T2 hyperintense lesions in the cerebellum and frontal white matter and a lesion in the cerebellum exhibited hemorrhagic changes and peripheral ring enhancement. The MRI features of listerial encephalitis are difficult to differentiate from those of neuropsychiatric SLE and various other diseases. Here, we report a case of hemorrhagic listerial encephalitis in a patient with SLE.
MeSH Terms
Figure
Reference
-
1. Horta-Baas G, Guerrero-Soto O, Barile-Fabris L. Central nervous system infection by Listeria monocytogenes in patients with systemic lupus erythematosus: analysis of 26 cases, including the report of a new case. Reumatol Clin. 2013; 9:340–347.2. Yang CD, Wang XD, Ye S, Gu YY, Bao CD, Wang Y, et al. Clinical features, prognostic and risk factors of central nervous system infections in patients with systemic lupus erythematosus. Clin Rheumatol. 2007; 26:895–901.3. Lee MC, Wu YK, Chen CH, Wu TW, Lee CH. Listeria monocytogenes meningitis in a young woman with systemic lupus erythematosus. Rheumatol Int. 2011; 31:555–557.4. Osborn AG. Osborns brain: imaging, pathology, and anatomy. Salt Lake City, UT: Amirsys;2013.5. McCaffrey LM, Petelin A, Cunha BA. Systemic lupus erythematosus (SLE) cerebritis versus Listeria monocytogenes meningoencephalitis in a patient with systemic lupus erythematosus on chronic corticosteroid therapy: the diagnostic importance of cerebrospinal fluid (CSF) of lactic acid levels. Heart Lung. 2012; 41:394–397.6. López Montes A, Andrés Mompeán E, Martínez Villaescusa M, Hernández Belmonte A, Mateos Rodríguez F, Abad Ortiz L, et al. [Meningoencephalitis by Listeria in the lupus disease]. An Med Interna. 2005; 22:379–382.7. Alper G, Knepper L, Kanal E. MR findings in listerial rhombencephalitis. AJNR Am J Neuroradiol. 1996; 17:593–596.8. Just M, Krämer G, Higer HP, Thömke F, Pfannenstiel P. MRI of Listeria rhombencephalitis. Neuroradiology. 1987; 29:401–402.9. Hatipoglu HG, Gurbuz MO, Sakman B, Yuksel E. Diffusion-weighted magnetic resonance imaging in rhombencephalitis due to Listeria monocytogenes. Acta Radiol. 2007; 48:464–467.10. Pelegrín I, Moragas M, Suárez C, Ribera A, Verdaguer R, Martínez-Yelamos S, et al. Listeria monocytogenes meningoencephalitis in adults: analysis of factors related to unfavourable outcome. Infection. 2014; 42:817–827.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus
- A Ruptured Aneurysm in a Patient with Systemic Lupus Erythematosus: Case Report
- Anti-N-Methyl-D-Aspartate Receptor Encephalitis in a Patient with Systemic Lupus Erythematosus
- Multiple Dermatofibromas in a woman with Systemic Lupus Erythematosus
- Adalimumab-induced Lupus Erythematosus Profundus in a Rheumatoid Arthritis Patient