J Korean Assoc Oral Maxillofac Surg.
2017 Apr;43(2):125-133. 10.5125/jkaoms.2017.43.2.125.
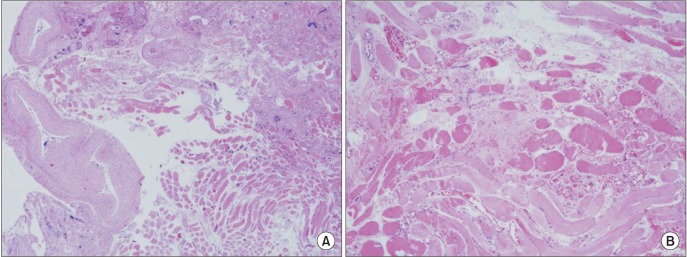
Intramuscular hemangiomas on the masseter muscle and orbicularis oris muscle: a report of two cases
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Inha University College of Medicine, Incheon, Korea. kik@inha.ac.kr
- 2Department of Pathology, Inha University School of Medicine, Incheon, Korea.
- KMID: 2377017
- DOI: http://doi.org/10.5125/jkaoms.2017.43.2.125
Abstract
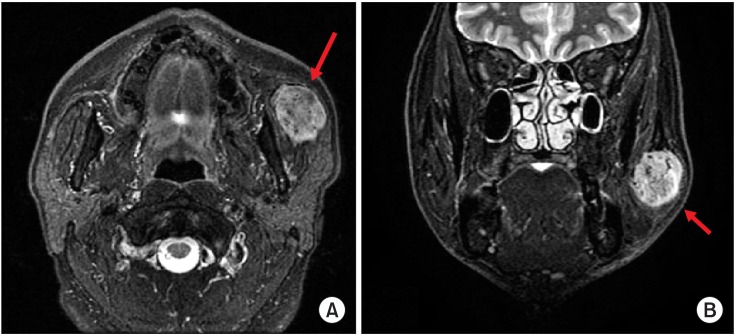
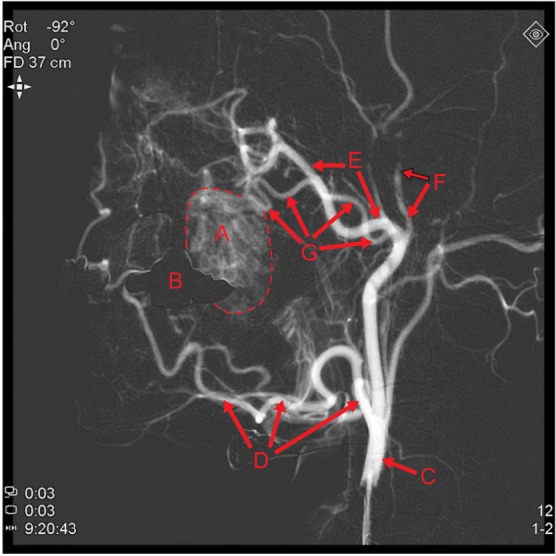
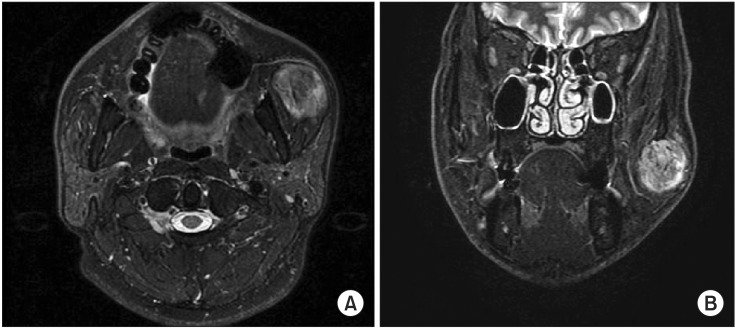
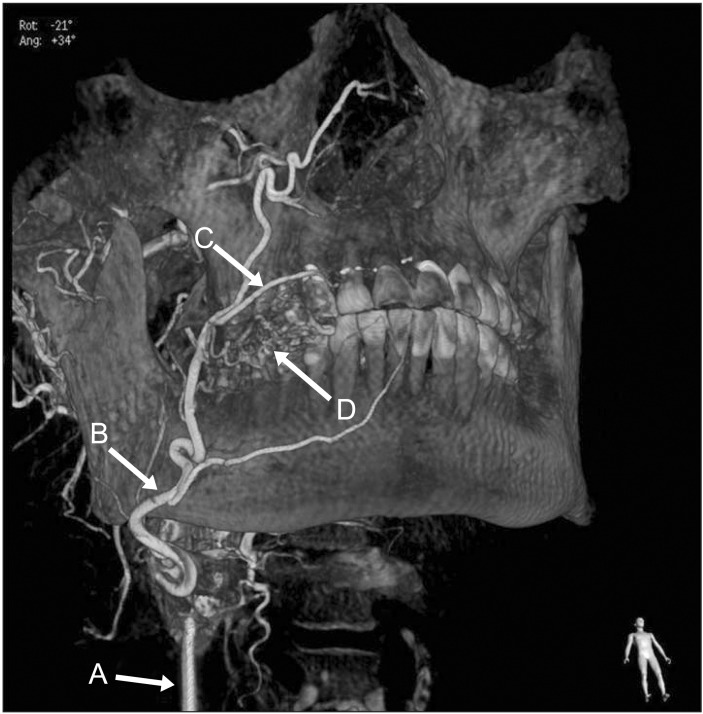
- Intramuscular hemangioma (IMH) is a rare vascular disease involving skeletal muscle, comprising only 0.8% of hemangiomas. About 10% to 15% of IMHs occur in the head and neck region, mostly involving the masseter muscle. IMH occurs mostly in childhood, but is often not found until unexpected enlargement, pain, or cosmetic asymmetry occurs in adulthood. Several non-surgical treatments including cryotherapy, sclerosant injection, and arterial ligature have been described, but complete surgical resection is the curative intervention. In this report, we present two rare cases of IMH. One IMH case in a 48-year-old male occurred in the masseter muscle feeding from the transverse facial artery. Embolization of the distal branch of the facial artery was first conducted, and then the buccal mass was removed surgically via the intraoral approach. A second IMH case in a 58-year-old female occurred in the orbicularis oris muscle feeding from the superior labial artery, and the mass was excised surgically without embolization.
MeSH Terms
Figure
Reference
-
1. Watson WL, McCarthy WD. Blood and lymph vessel tumors. Srug Gynecol Obstet. 1940; 71:569–588.2. Wolf GT, Daniel F, Krause CJ, Kaufman RS. Intramuscular hemangioma of the head and neck. Laryngoscope. 1985; 95:210–213. PMID: 3968956.
Article3. Gordon JS, Mandel L. Masseteric intramuscular hemangioma: case report. J Oral Maxillofac Surg. 2014; 72:2192–2196. PMID: 24976110.
Article4. Odabasi AO, Metin KK, Mutlu C, Başak S, Erpek G. Intramuscular hemangioma of the masseter muscle. Eur Arch Otorhinolaryngol. 1999; 256:366–369. PMID: 10473832.
Article5. Chan MJ, McLean NR, Soames JV. Intramuscular haemangioma of the orbicularis oris muscle. Br J Oral Maxillofac Surg. 1992; 30:192–194. PMID: 1622968.
Article6. Kinni ME, Webb RI, Christensen RE. Intramuscular hemangioma of the orbicularis oris muscle: report of case. J Oral Surg. 1981; 39:780–782. PMID: 6944460.7. Righini CA, Berta E, Atallah I. Intramuscular cavernous hemangioma arising from the masseter muscle. Eur Ann Otorhinolaryngol Head Neck Dis. 2014; 131:57–59. PMID: 23845293.
Article8. Ichimura K, Nibu K, Tanaka T. Essentials of surgical treatment for intramasseteric hemangioma. Eur Arch Otorhinolaryngol. 1995; 252:125–129. PMID: 7662343.
Article9. Righi S, Boffano P, Malvè L, Rossi P, Zanardi F, Pateras D. Intramural perimasseteric hemangiomas of the inner cheek. J Craniofac Surg. 2015; 26:959–960. PMID: 25974807.
Article10. Chaudry MI, Manzoor MU, Turner RD, Turk AS. Diagnostic imaging of vascular anomalies. Facial Plast Surg. 2012; 28:563–574. PMID: 23188683.
Article11. Donnelly LF, Adams DM, Bisset GS 3rd. Vascular malformations and hemangiomas: a practical approach in a multidisciplinary clinic. AJR Am J Roentgenol. 2000; 174:597–608. PMID: 10701595.12. Flors L, Leiva-Salinas C, Maged IM, Norton PT, Matsumoto AH, Angle JF, et al. MR imaging of soft-tissue vascular malformations: diagnosis, classification, and therapy follow-up. Radiographics. 2011; 31:1321–1340. PMID: 21918047.
Article13. Yilmaz S, Kozakewich HP, Alomari AI, Fishman SJ, Mulliken JB, Chaudry G. Intramuscular capillary-type hemangioma: radiologic-pathologic correlation. Pediatr Radiol. 2014; 44:558–565. PMID: 24487677.
Article14. Rosbe KW, Hess CP, Dowd CF, Frieden IJ. Masseteric venous malformations: diagnosis, treatment, and outcomes. Otolaryngol Head Neck Surg. 2010; 143:779–783. PMID: 21109077.
Article15. Lee SK, Kwon SY. Intramuscular cavernous hemangioma arising from masseter muscle: a diagnostic dilemma (2006: 12b). Eur Radiol. 2007; 17:854–857. PMID: 17225132.
Article16. Allen PW, Enzinger FM. Hemangioma of skeletal muscle. An analysis of 89 cases. Cancer. 1972; 29:8–22. PMID: 5061701.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cavernous Hemangioma of the Masseter Muscle
- Intramuscular hemangioma formation in the masseter muscle: a case report
- Intramuscular Hemangioma of the Sternocleidomastoid Muscle: An Unusual Neck Mass
- A hemangioma in the masseter muscle: a case report
- The effects of facial denervation on facial muscles and bones in growing rabbits