J Adv Prosthodont.
2016 Jun;8(3):194-200. 10.4047/jap.2016.8.3.194.
Early complications and performance of 327 heat-pressed lithium disilicate crowns up to five years
- Affiliations
-
- 1Department of Prosthodontics, Centre for Dentistry, Oral Medicine, and Maxillofacial Surgery, Eberhard-Karls-Universität Tübingen, Tübingen, Germany. fabian.huettig@med.uni-tuebingen.de
- KMID: 2376843
- DOI: http://doi.org/10.4047/jap.2016.8.3.194
Abstract
- PURPOSE
The prospective follow-up aimed to assess the performance of lithium disilicate crowns and clinical reasons of adverse events compromising survival and quality.
MATERIALS AND METHODS
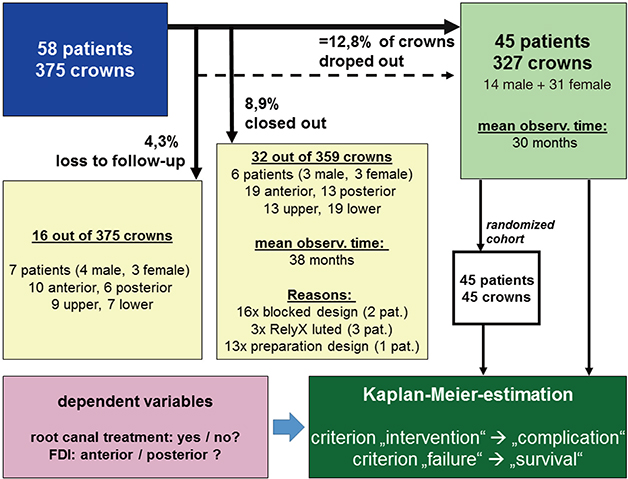
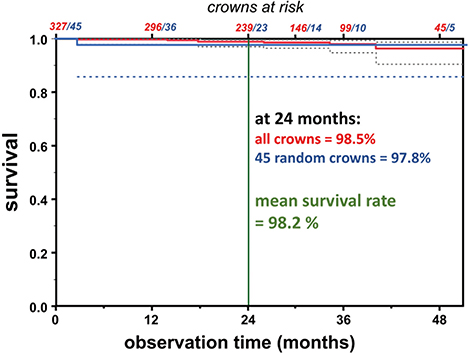
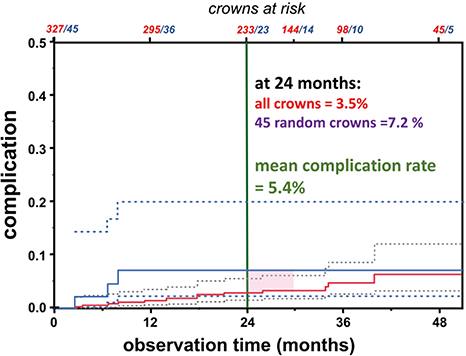
58 patients were treated with 375 heat-pressed monolithic crowns, which were bonded with resin cement. Annual recalls up to five years included a complete dental examination as well as quality assessment using CDA-criteria. Any need for clinical intervention led to higher complication rate and any failure compromised the survival rate. Kaplan-Meier-method was applied to all crowns and a dataset containing one randomly selected crown from each patient.
RESULTS
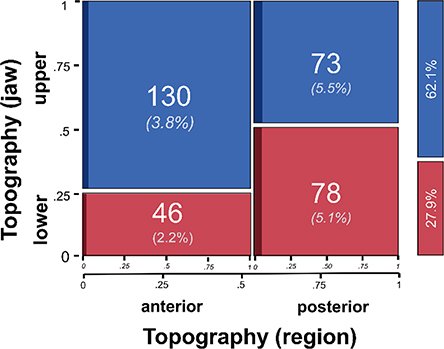
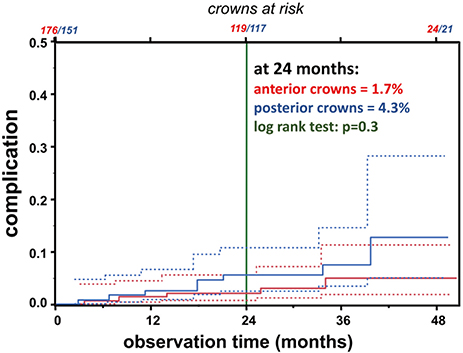
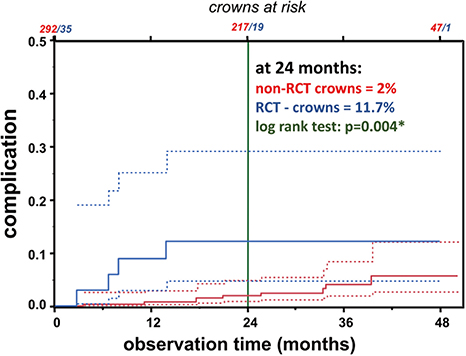
Due to drop-outs, 45 patients (31 females, 14 males) with the average age of 43 years (range = 17-73) who had 327 crowns (176 anterior, 151 posterior; 203 upper jaw, 124 lower jaw) were observed and evaluated for between 4 and 51 months (median = 28). Observation revealed 4 chippings, 3 losses of retention, 3 fractures, 3 secondary caries, 1 endodontic problem, and 1 tooth fracture. Four crowns had to be removed. Survival and complication rate was estimated 98.2% and 5.4% at 24 months, and 96.8% and 7.1% at 48 months. The complication rate was significantly higher for root canal treated teeth (12%, P<.01) at 24 months. At the last observation, over 90% of all crowns showed excellent ratings (CDA-rating Alfa) for color, marginal fit, and caries.
CONCLUSION
Heat pressed lithium disilicate crowns showed an excellent performance. Besides a careful luting, dentists should be aware of patients' biological prerequisites (grade of caries, oral hygiene) to reach full success with these crowns.
Keyword
MeSH Terms
Figure
Reference
-
1. Akın A, Toksavul S, Toman M. Clinical Marginal and Internal Adaptation of Maxillary Anterior Single All-Ceramic Crowns and 2-year Randomized Controlled Clinical Trial. J Prosthodont. 2015; 24:345–350.2. Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater. 2015; 31:603–623.3. Shenoy A, Shenoy N. Dental ceramics: An update. J Conserv Dent. 2010; 13:195–203.4. Edelhoff D, Brix O. All-ceramic restorations in different indications: a case series. J Am Dent Assoc. 2011; 142:14S–19S.5. Fabbri G, Zarone F, Dellificorelli G, Cannistraro G, De Lorenzi M, Mosca A, Sorrentino R. Clinical evaluation of 860 anterior and posterior lithium disilicate restorations: retrospective study with a mean follow-up of 3 years and a maximum observational period of 6 years. Int J Periodontics Restorative Dent. 2014; 34:165–177.6. Mörmann W, Wolf D, Ender A, Bindl A, Ghring T, Attin T. Effect of two self-adhesive cements on marginal adaptation and strength of esthetic ceramic CAD/CAM molar crowns. J Prosthodont. 2009; 18:403–410.7. Gehrt M, Wolfart S, Rafai N, Reich S, Edelhoff D. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin Oral Investig. 2013; 17:275–284.8. Christensen GJ. Use of luting or bonding with lithium disilicate and zirconia crowns. J Am Dent Assoc. 2014; 145:383–386.9. Manso AP, Silva NR, Bonfante EA, Pegoraro TA, Dias RA, Carvalho RM. Cements and adhesives for all-ceramic restorations. Dent Clin North Am. 2011; 55:311–332.10. Lekesiz H. Reliability estimation for single-unit ceramic crown restorations. J Dent Res. 2014; 93:923–928.11. Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 2003; 89:268–274.12. Hooshmand T, Rostami G, Behroozibakhsh M, Fatemi M, Keshvad A, van Noort R. Interfacial fracture toughness of different resin cements bonded to a lithium disilicate glass ceramic. J Dent. 2012; 40:139–145.13. Burke FJ, Fleming GJ, Nathanson D, Marquis PM. Are adhesive technologies needed to support ceramics? An assessment of the current evidence. J Adhes Dent. 2002; 4:7–22.14. Pieger S, Salman A, Bidra AS. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review. J Prosthet Dent. 2014; 112:22–30.15. Guess PC, Schultheis S, Bonfante EA, Coelho PG, Ferencz JL, Silva NR. All-ceramic systems: laboratory and clinical performance. Dent Clin North Am. 2011; 55:333–352.16. Land MF, Hopp CD. Survival rates of all-ceramic systems differ by clinical indication and fabrication method. J Evid Based Dent Pract. 2010; 10:37–38.17. Conrad HJ, Seong WJ, Pesun IJ. Current ceramic materials and systems with clinical recommendations: a systematic review. J Prosthet Dent. 2007; 98:389–404.18. Cvar JF, Ryge G. Reprint of criteria for the clinical evaluation of dental restorative materials. 1971. Clin Oral Investig. 2005; 9:215–232.19. Groten M, Axmann D. Time needed for data collection in clinical studies on fixed prosthodontics. Int J Prosthodont. 2004; 17:651–656.20. Klink A, Huettig F. Complication and survival of Mark II restorations: 4-year clinical follow-up. Int J Prosthodont. 2013; 26:272–276.21. Anusavice KJ. Standardizing failure, success, and survival decisions in clinical studies of ceramic and metal-ceramic fixed dental prostheses. Dent Mater. 2012; 28:102–111.22. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958; 53:457–481.23. Hickel R, Roulet JF, Bayne S, Heintze SD, Mjör IA, Peters M, Rousson V, Randall R, Schmalz G, Tyas M, Vanherle G. Recommendations for conducting controlled clinical studies of dental restorative materials. Int Dent J. 2007; 57:300–302.24. Frankenberger R, Reinelt C, Petschelt A, Krämer N. Operator vs. material influence on clinical outcome of bonded ceramic inlays. Dent Mater. 2009; 25:960–968.25. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications in fixed prosthodontics. J Prosthet Dent. 2003; 90:31–41.26. Selz CF, Strub JR, Vach K, Guess PC. Long-term performance of posterior InCeram Alumina crowns cemented with different luting agents: a prospective, randomized clinical split-mouth study over 5 years. Clin Oral Investig. 2014; 18:1695–1703.27. Cortellini D, Canale A. Bonding lithium disilicate ceramic to feather-edge tooth preparations: a minimally invasive treatment concept. J Adhes Dent. 2012; 14:7–10.28. Guess PC, Zavanelli RA, Silva NR, Bonfante EA, Coelho PG, Thompson VP. Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns: comparison of failure modes and reliability after fatigue. Int J Prosthodont. 2010; 23:434–442.29. Contrepois M, Soenen A, Bartala M, Laviole O. Marginal adaptation of ceramic crowns: a systematic review. J Prosthet Dent. 2013; 110:447–454.30. Fabbri G, Mancini R, Marinelli V, Ban G. Anterior discolored teeth restored with procera all-ceramic restorations: a clinical evaluation of the esthetic outcome based on the thickness of the core selected. Eur J Esthet Dent. 2011; 6:76–86.31. Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J. 2010; 43:171–189.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- FLEXURE STRENGTH AND MICROSTRUCTURE OF IPS EMPRESS 2 GLASS-CERAMIC ON HEAT PRESSING AND HEAT TREATMENTS
- Mechanical Properties Of Reused Lithium Disilicate Glass-Ceramic Of Ips Empress 2 System
- Clinical Evaluation of Lithium Disilicate Pressed Zirconia and Monolithic Zirconia in Posterior Implant-Supported Prostheses
- Comparison of micro CT and cross-section technique for evaluation of marginal and internal fit of lithium disilicate crowns
- A prospective clinical of lithium disilicate pressed zirconia and monolithic zirconia in posterior implant-supported prostheses: A 24-month follow-up