Clin Exp Otorhinolaryngol.
2017 Mar;10(1):121-128. 10.21053/ceo.2015.01424.
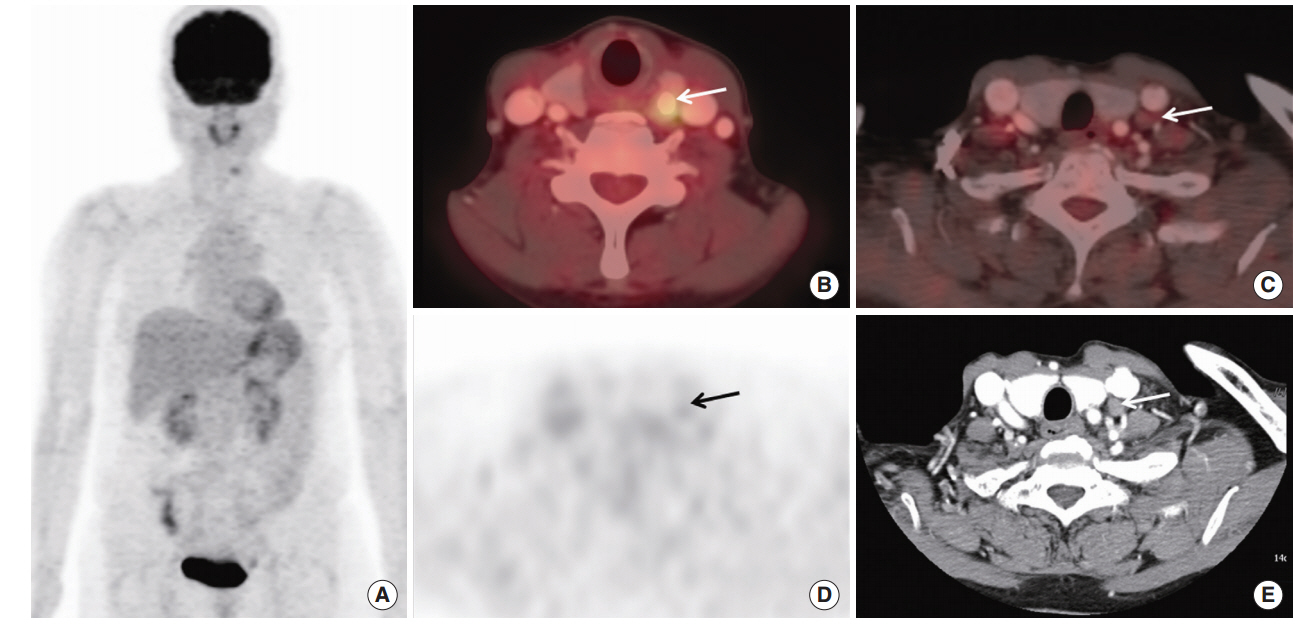
Preoperative Lymph Node Staging by FDG PET/CT With Contrast Enhancement for Thyroid Cancer: A Multicenter Study and Comparison With Neck CT
- Affiliations
-
- 1Department of Nuclear Medicine, Chosun University Hospital, Gwangju, Korea.
- 2Department of Nuclear Medicine, Chonbuk National University Hospital, Jeonju, Korea.
- 3Department of Nuclear Medicine, Yeungnam University Medical Center, Daegu, Korea.
- 4Department of Nuclear Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 5Department of Otolaryngology-Head and Neck Surgery, Research Institute of Clinical Medicine, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea.
- 6Department of Otolaryngology-Head and Neck Surgery, Chosun University College of Medicine, Gwangju, Korea.
- 7Department of Radiology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 8Department of Nuclear Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea. jmipark@schmc.ac.kr
- KMID: 2376419
- DOI: http://doi.org/10.21053/ceo.2015.01424
Abstract
OBJECTIVES
The purpose of this study was to compare lymph node (LN) staging using ¹â¸F-fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) with contrast-enhancement (CE) PET/CT and contrast-enhanced neck CT (neck CT) in patients with thyroid cancer with level-by-level comparison with various factors.
METHODS
This was a retrospective multicenter study. A total of 85 patients were enrolled. Patients who underwent a preoperative evaluation by CE PET/CT and neck CT for thyroid cancer were enrolled. The gold standard for LN was the combination of surgical pathology and clinical follow-up. We compared CE PET/CT with neck CT using a level-by-level method. Factors, including age, sex, camera, arm position, tumor size, extra-thyroidal extension, tumor location, number of primary tumors, primary tumor maximum standardized uptake value, and the interval from scan to operation were also analyzed.
RESULTS
Overall accuracy was 81.2% for CE PET/CT and 68.2% for neck CT. CE PET/CT was more sensitive than neck CT (65.8% vs. 44.7%). Also, CE PET/CT showed higher negative predictive value (77.2% vs. 66.1%). CE PET/CT showed good agreement with the gold standard (weighted kappa [κ], 0.7) for differentiating N0, N1a, and N1b, whereas neck CT showed moderate agreement (weighted κ, 0.5). CE PET/CT showed better agreement for the number of levels involved with the gold standard (weighted κ, 0.7) than that of neck CT with the gold standard (weighted κ, 0.5). The accuracies for differentiating N0, N1a, and N1b were 81.2% for CE PET/CT and 68.2% for neck CT. Level-by-level analysis showed that CE PET/CT was more sensitive and has higher negative predictive value for detecting ipsilateral level IV and level VI LNs than neck CT. Other analyzed factors were not related to accuracies of both modalities.
CONCLUSION
CE PET/CT was more sensitive and reliable than neck CT for preoperative LN staging in patients with thyroid cancer.
Keyword
MeSH Terms
Figure
Reference
-
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012; Jan-Feb. 62(1):10–29.
Article2. Enewold L, Zhu K, Ron E, Marrogi AJ, Stojadinovic A, Peoples GE, et al. Rising thyroid cancer incidence in the United States by demographic and tumor characteristics, 1980-2005. Cancer Epidemiol Biomarkers Prev. 2009; Mar. 18(3):784–91.
Article3. Dimov RS. The effect of neck dissection on quality of life in patients with differentiated thyroid cancer. Gland Surg. 2013; Nov. 2(4):219–26.4. Adam MA, Pura J, Goffredo P, Dinan MA, Reed SD, Scheri RP, et al. Presence and number of lymph node metastases are associated with compromised survival for patients younger than age 45 years with papillary thyroid cancer. J Clin Oncol. 2015; Jul. 33(21):2370–5.
Article5. Stack BC Jr, Ferris RL, Goldenberg D, Haymart M, Shaha A, Sheth S, et al. American Thyroid Association consensus review and statement regarding the anatomy, terminology, and rationale for lateral neck dissection in differentiated thyroid cancer. Thyroid. 2012; May. 22(5):501–8.
Article6. Luster M, Weber T, Verburg FA. Differentiated thyroid cancer-personalized therapies to prevent overtreatment. Nat Rev Endocrinol. 2014; Sep. 10(9):563–74.
Article7. Grant CS. Papillary thyroid cancer: strategies for optimal individualized surgical management. Clin Ther. 2014; Jul. 36(7):1117–26.
Article8. Kim E, Park JS, Son KR, Kim JH, Jeon SJ, Na DG. Preoperative diagnosis of cervical metastatic lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid. 2008; Apr. 18(4):411–8.
Article9. Langer JE, Mandel SJ. Sonographic imaging of cervical lymph nodes in patients with thyroid cancer. Neuroimaging Clin N Am. 2008; Aug. 18(3):479–89.
Article10. Pak K, Kim SJ, Kim IJ, Kim BH, Kim SS, Jeon YK. The role of 18F-fluorodeoxyglucose positron emission tomography in differentiated thyroid cancer before surgery. Endocr Relat Cancer. 2013; Jul. 20(4):R203–13.
Article11. Byun BH, Jeong UG, Hong SP, Min JJ, Chong A, Song HC, et al. Prediction of central lymph node metastasis from papillary thyroid microcarcinoma by 18F-fluorodeoxyglucose PET/CT and ultrasonography. Ann Nucl Med. 2012; Jul. 26(6):471–7.
Article12. Choi JS, Kim J, Kwak JY, Kim MJ, Chang HS, Kim EK. Preoperative staging of papillary thyroid carcinoma: comparison of ultrasound imaging and CT. AJR Am J Roentgenol. 2009; Sep. 193(3):871–8.
Article13. American Joint Committee on Cancer. AJCC cancer staging manual. 6th ed. New York: Springer-Verlag;2002.14. Som PM. Detection of metastasis in cervical lymph nodes: CT and MR criteria and differential diagnosis. AJR Am J Roentgenol. 1992; May. 158(5):961–9.
Article15. Jeong HS, Baek CH, Son YI, Choi JY, Kim HJ, Ko YH, et al. Integrated 18F-FDG PET/CT for the initial evaluation of cervical node level of patients with papillary thyroid carcinoma: comparison with ultrasound and contrast-enhanced CT. Clin Endocrinol (Oxf). 2006; Sep. 65(3):402–7.16. Mitchell JC, Grant F, Evenson AR, Parker JA, Hasselgren PO, Parangi S. Preoperative evaluation of thyroid nodules with 18FDG-PET/CT. Surgery. 2005; Dec. 138(6):1166–74.
Article17. Choi WH, Chung YA, Han EJ, Sohn HS, Lee SH. Clinical value of integrated [18F]fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography in the preoperative assessment of papillary thyroid carcinoma: comparison with sonography. J Ultrasound Med. 2011; Sep. 30(9):1267–73.18. Choi JW, Yoon YH, Yoon YH, Kim SM, Koo BS. Characteristics of primary papillary thyroid carcinoma with false-negative findings on initial (18)F-FDG PET/CT. Ann Surg Oncol. 2011; May. 18(5):1306–11.
Article19. Jeong HS, Chung M, Baek CH, Ko YH, Choi JY, Son YI. Can [18F]-fluorodeoxyglucose standardized uptake values of PET imaging predict pathologic extrathyroid invasion of thyroid papillary microcarcinomas? Laryngoscope. 2006; Dec. 116(12):2133–7.20. Morita S, Mizoguchi K, Suzuki M, Iizuka K. The accuracy of (18)[F]-fluoro-2-deoxy-D-glucose-positron emission tomography/computed tomography, ultrasonography, and enhanced computed tomography alone in the preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma. World J Surg. 2010; Nov. 34(11):2564–9.
Article21. Schlumberger M, Tubiana M, De Vathaire F, Hill C, Gardet P, Travagli JP, et al. Long-term results of treatment of 283 patients with lung and bone metastases from differentiated thyroid carcinoma. J Clin Endocrinol Metab. 1986; Oct. 63(4):960–7.22. Shaha AR, Shah JP, Loree TR. Differentiated thyroid cancer presenting initially with distant metastasis. Am J Surg. 1997; Nov. 174(5):474–6.23. Pryma DA, Schoder H, Gonen M, Robbins RJ, Larson SM, Yeung HW. Diagnostic accuracy and prognostic value of 18F-FDG PET in Hurthle cell thyroid cancer patients. J Nucl Med. 2006; Aug. 47(8):1260–6.24. Yoneyama T, Tateishi U, Endo I, Inoue T. Staging accuracy of pancreatic cancer: comparison between non-contrast-enhanced and contrast-enhanced PET/CT. Eur J Radiol. 2014; Oct. 83(10):1734–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Neck CT and ¹â¸F-FDG PET-CT for Making the Preoperative Diagnosis of Lymph Node Metastasis in Papillary Thyroid Cancer
- (18)F-FDG PET/CT with Contrast Enhancement for Evaluation of Axillary Lymph Node Involvement in T1 Breast Cancer
- The Diagnostic Utility of Ultrasonography, CT and PET/CT for the Preoperative Evaluation of Cervical Lymph Node Metastasis in Papillary Thyroid Cancer Patients
- Reliability of 18F-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography in the Nodal Staging of Colorectal Cancer Patients
- F18-fluorodeoxyglucose-positron emission tomography and computed tomography is not accurate in preoperative staging of gastric cancer