Korean J Endocr Surg.
2013 Jun;13(2):83-86. 10.0000/kjes.2013.13.2.83.
Thyroid Lobectomy for Treatment of Well Differentiated Thyroid Cancer Confined to One Lobe
- Affiliations
-
- 1Department of Surgery, Chosun University College of Medicine, Gwangju, Korea. mdkckim8@hanmail.net
- KMID: 2375419
- DOI: http://doi.org/10.0000/kjes.2013.13.2.83
Abstract
- PURPOSE
There has been controversy of the lobectomy for well differentiated thyroid cancer (WDTC). Current guidelines recommend total thyroidectomy for the cancer over 1cm, despite previous report suggesting that the lobectomy provides similar excellent outcomes. The purpose of our study is to report our experience of WDTC treated by thyroid lobectomy.
METHODS
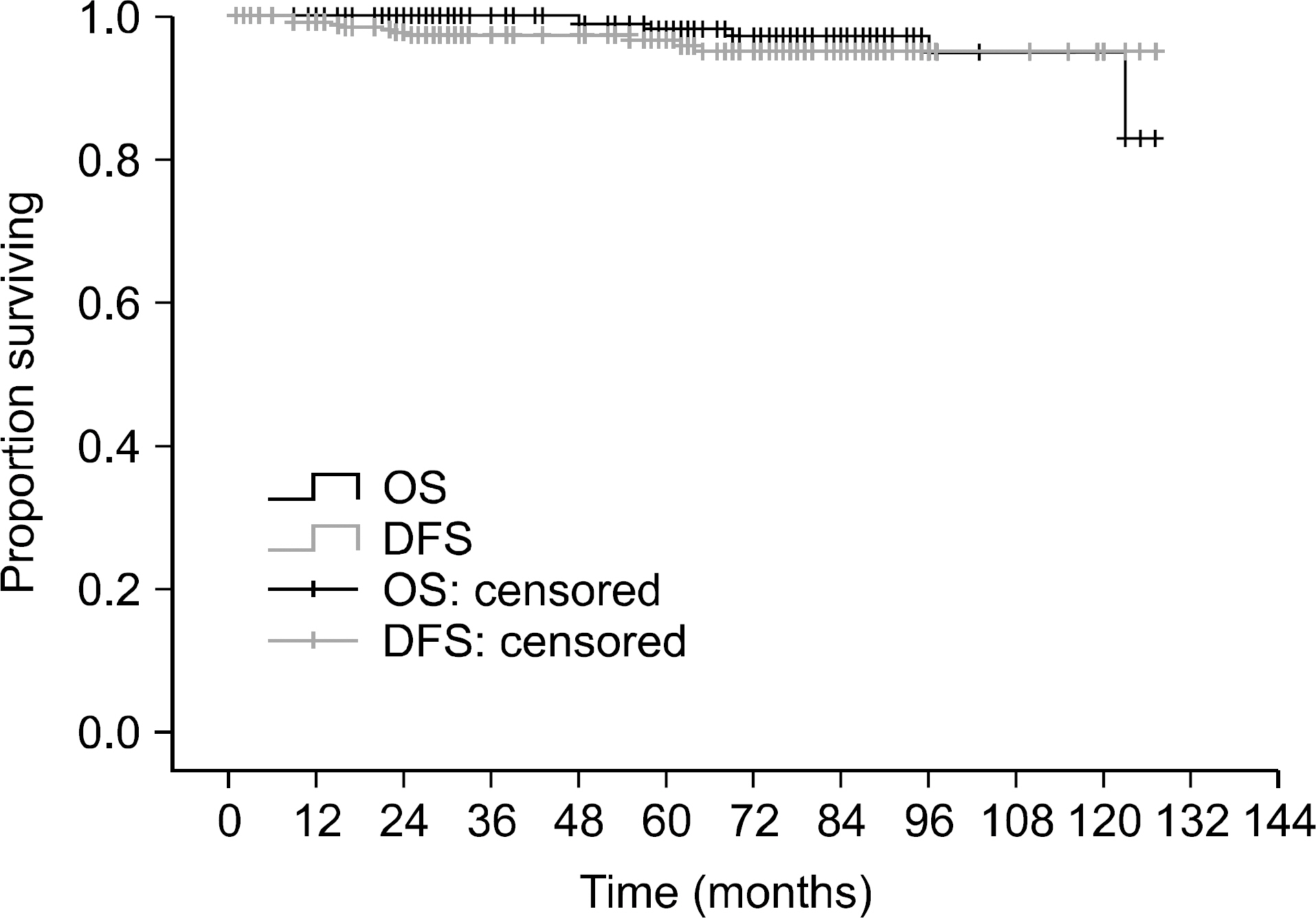
We retrospectively analyzed 284 patients with WDTC treated by thyroid lobectomy at department of Surgery in Chosun University Hospital from January 2002 to December 2010. Overall survival (OS) and disease-free survival (DFS) were determined by the Kaplan-Meier method. Factors predictive of recurrence by univariate and multivariate analysis were determined using the χ2 test and Cox proportional hazard model respectively.
RESULTS
With a mean follow-up of 60.4 months, OS and RFS for all patients were 97.9% and 96.5% respectively. No patient died due to WDTC. Univariate analysis showed statistically significant differences in recurrence by tumor size (P=0.013) and presence of invasion (P=0.039). However, Multivariate analysis showed no significant difference in local recurrence.
CONCLUSION
Patients with WDTC confined to one lobe can be safely treated by lobectomy.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Chen AY, Jemal A, Ward EM. Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer. 2009; 115:3801–7.
Article2. Enewold L, Zhu K, Ron E, Marrogi AJ, Stojadinovic A, Peoples GE, et al. Rising thyroid cancer incidence in the United States by demographic and tumor characteristics, 1980–2005. Cancer Epidemiol Biomarkers Prev. 2009; 18:784–91.
Article3. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA. 2006; 295:2164–7.
Article4. Shah JP, Loree TR, Dharker D, Strong EW. Lobectomy versus total thyroidectomy for differentiated carcinoma of the thyroid: a matched-pair analysis. Am J Surg. 1993; 166:331–5.
Article5. Hay ID, Grant CS, Taylor WF, McConahey WM. Ipsilateral lobectomy versus bilateral lobar resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system. Surgery. 1987; 102:1088–95.6. Sanders LE, Cady B. Differentiated thyroid cancer: reexamination of risk groups and outcome of treatment. Arch Surg. 1998; 133:419–25.7. Loh KC, Greenspan FS, Gee L, Miller TR, Yeo PP. Pathological tumor-node-metastasis (pTNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. J Clin Endocrinol Metab. 1997; 82:3553–62.
Article8. Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994; 97:418–28.
Article9. Yi KH, Park YJ, Koong SS, Kim JH, Na DG, Ryu JS, et al. Revised Korean thyroid association management guidelines for patients with thyroid nodules and thyroid cancer. J Korean Soc Radiol. 2011; 64:389–416.
Article10. Shaha AR, Shah JP, Loree TR. Risk group stratification and prognostic factors in papillary carcinoma of thyroid. Ann Surg Oncol. 1996; 3:534–8.
Article11. Sugitani I, Toda K, Yamamoto N, Sakamoto A, Fujimoto Y. Reevaluation of histopathological factors affecting prognosis of differentiated thyroid carcinoma in an iodine-sufficient country. World J Surg. 2010; 34:1265–73.
Article12. Cady B, Rossi R. An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery. 1988; 104:947–53.13. McConahey WM, Hay ID, Woolner LB, van Heerden JA, Taylor WF. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin Proc. 1986; 61:978–96.
Article14. Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery. 1993; 114:1050–7.15. Lin HW, Bhattacharyya N. Survival impact of treatment options for papillary microcarcinoma of the thyroid. Laryngoscope. 2009; 119:1983–7.
Article16. Saadi H, Kleidermacher P, Esselstyn C Jr. Conservative management of patients with intrathyroidal well-differentiated follicular thyroid carcinoma. Surgery. 2001; 130:30–5.
Article17. Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940–1999): temporal trends in initial therapy and longterm outcome in 2444 consecutively treated patients. World J Surg. 2002; 26:879–85.
Article18. Lee MJ, Ha TK, Park HK, Lee HT, Shin JH, An MS, et al. Prognostic significance of minimal extrathyroidal extension of papillary thyroid carcinomas. Korean J Endocrine Surg. 2012; 12:102–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thyroid Lobectomy as an Initial Treatment Option on 1-4 cm Papillary Cancer
- Preoperative Staging of Well Differentiated Thyroid Cancer: US Is Enough?
- Pediatric thyroid cancer: key considerations based on the 2024 Korean Thyroid Association Differentiated Thyroid Cancer Management Guidelines
- ATA Guideline in a View Point of Nuclear Medicine
- Ablation of Remnant Thyroid Tissue with I-131 in Well Differentiated Thyroid Cancer After Surgery