J Korean Med Sci.
2017 May;32(5):796-802. 10.3346/jkms.2017.32.5.796.
Link between Serum Pepsinogen Concentrations and Upper Gastrointestinal Endoscopic Findings
- Affiliations
-
- 1Department of Internal Medicine, Digestive Disease Center, Konkuk University School of Medicine, Seoul, Korea. sunyoung@kuh.ac.kr
- KMID: 2375080
- DOI: http://doi.org/10.3346/jkms.2017.32.5.796
Abstract
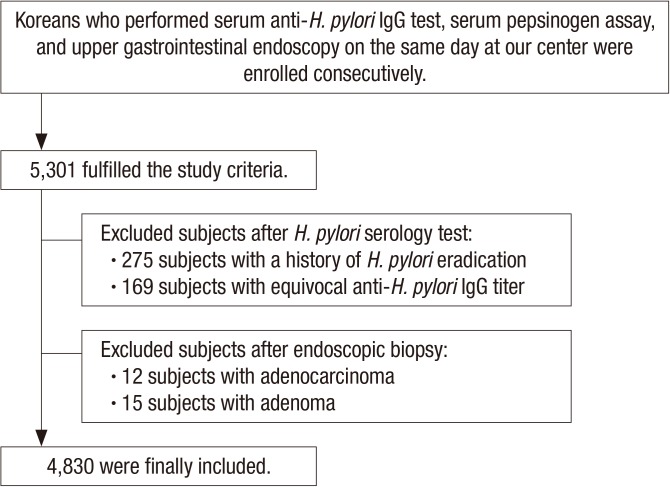
- The serum pepsinogen (PG) assay findings are correlated with the status of Helicobacter pylori infection, but there are controversies on the link with upper gastrointestinal (UGI) endoscopic findings. The aim of this study was to determine the significance of a serum PG assay for correlating with endoscopic findings in H. pylori-seroprevalent adult population. Korean adults who visited for a health check-up were included consecutively. Subjects after gastrectomy or H. pylori eradication were excluded. After completing the serum PG assay and anti-H. pylori immunoglobulin G (IgG) titer on the same day of UGI endoscopy, subjects with equivocal serology test finding or gastric neoplasm were excluded. Of the 4,830 included subjects, 3,116 (64.5%) were seropositive for H. pylori. Seropositive finding was related to high serum PG I (P < 0.001) and PG II (P < 0.001) concentrations, low PG I/II ratio (P < 0.001), old age (P < 0.001), and male gender (P = 0.006). After adjusting age and gender, the serum PG I and II concentrations were positively correlated with the presence of nodular gastritis (NG) (all P = 0.003). The serum PG I was positively correlated with gastric ulcer (P = 0.003), and it was correlated with duodenal ulcer in seropositive subjects (P = 0.008). The PG I/II ratio was positively correlated with erosive esophagitis, while it was inversely related to chronic atrophic gastritis and metaplastic gastritis (all P < 0.001). Our findings suggest that the serum PG assay finding correlates well with the UGI endoscopic finding. A higher serum PG concentration in subjects with NG and peptic ulcer disease suggests that endoscopic findings reflect gastric secreting ability.
MeSH Terms
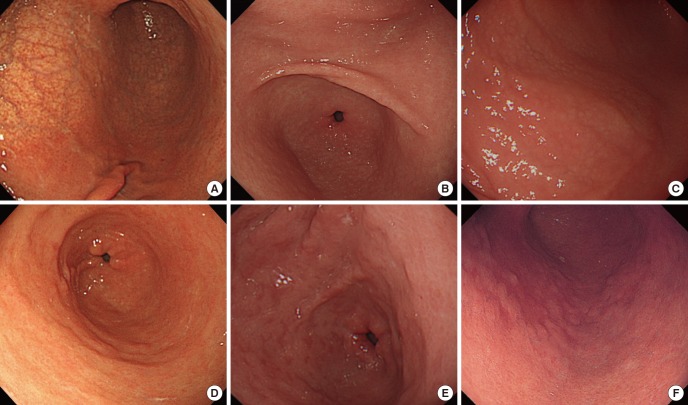
Figure
Cited by 2 articles
-
Nodular Gastritis as a Precursor Lesion of Atrophic and Metaplastic Gastritis
Young Jung Kim, Sun-Young Lee, Hojun Yang, Jeong Hwan Kim, In-Kyung Sung, Hyung Seok Park
Korean J Gastroenterol. 2019;73(6):332-340. doi: 10.4166/kjg.2019.73.6.332.Identification of Nodular Gastritis among Patients Diagnosed with Lymphofollicular Gastritis on a Gastric Biopsied Specimen
Young Jung Kim, Sun-Young Lee, Sang Pyo Lee, Jeong Hwan Kim, In-Kyung Sung, Hyung Seok Park, Chan Sup Shim, Hye Seung Han
Korean J Gastroenterol. 2018;71(3):143-152. doi: 10.4166/kjg.2018.71.3.143.
Reference
-
1. Kang HY, Kim N, Park YS, Hwang JH, Kim JW, Jeong SH, Lee DH, Jung HC, Song IS. Progression of atrophic gastritis and intestinal metaplasia drives Helicobacter pylori out of the gastric mucosa. Dig Dis Sci. 2006; 51:2310–2315. PMID: 17080249.2. Testoni PA, Bonassi U, Bagnolo F, Colombo E, Scelsi R. In diffuse atrophic gastritis, routine histology underestimates Helicobacter pylori infection. J Clin Gastroenterol. 2002; 35:234–239. PMID: 12192199.3. Storskrubb T, Aro P, Ronkainen J, Vieth M, Stolte M, Wreiber K, Engstrand L, Nyhlin H, Bolling-Sternevald E, Talley NJ, et al. A negative Helicobacter pylori serology test is more reliable for exclusion of premalignant gastric conditions than a negative test for current H. pylori infection: a report on histology and H. pylori detection in the general adult population. Scand J Gastroenterol. 2005; 40:302–311. PMID: 15932171.4. Hahn M, Fennerty MB, Corless CL, Magaret N, Lieberman DA, Faigel DO. Noninvasive tests as a substitute for histology in the diagnosis of Helicobacter pylori infection. Gastrointest Endosc. 2000; 52:20–26. PMID: 10882957.5. Shin CM, Kim N, Lee HS, Lee HE, Lee SH, Park YS, Hwang JH, Kim JW, Jeong SH, Lee DH, et al. Validation of diagnostic tests for Helicobacter pylori with regard to grade of atrophic gastritis and/or intestinal metaplasia. Helicobacter. 2009; 14:512–519. PMID: 19889068.6. Nardone G, Rocco A, Staibano S, Mezza E, Autiero G, Compare D, De Rosa G, Budillon G. Diagnostic accuracy of the serum profile of gastric mucosa in relation to histological and morphometric diagnosis of atrophy. Aliment Pharmacol Ther. 2005; 22:1139–1146. PMID: 16305728.7. Song HJ, Jang SJ, Yun SC, Park YS, Kim MJ, Lee SM, Choi KD, Lee GH, Jung HY, Kim JH. Low levels of pepsinogen I and pepsinogen I/II ratio are valuable serologic markers for predicting extensive gastric corpus atrophy in patients undergoing endoscopic mucosectomy. Gut Liver. 2010; 4:475–480. PMID: 21253295.8. Choi HS, Lee SY, Kim JH, Sung IK, Park HS, Shim CS, Jin CJ. Combining the serum pepsinogen level and Helicobacter pylori antibody test for predicting the histology of gastric neoplasm. J Dig Dis. 2014; 15:293–298. PMID: 24602176.9. Park SY, Lim SO, Ki HS, Jun CH, Park CH, Kim HS, Choi SK, Rew JS. Low pepsinogen I level predicts multiple gastric epithelial neoplasias for endoscopic resection. Gut Liver. 2014; 8:277–281. PMID: 24827624.10. Nomura S, Ida K, Terao S, Adachi K, Kato T, Watanabe H, Shimbo T; Research Group for Establishment of Endoscopic Diagnosis of Chronic Gastritis. Endoscopic diagnosis of gastric mucosal atrophy: multicenter prospective study. Dig Endosc. 2014; 26:709–719. PMID: 24698334.11. Lee SY. Endoscopic gastritis, serum pepsinogen assay, and Helicobacter pylori infection. Korean J Intern Med. 2016; 31:835–844. PMID: 27604795.12. Rubenstein JH, Inadomi JM, Scheiman J, Schoenfeld P, Appelman H, Zhang M, Metko V, Kao JY. Association between Helicobacter pylori and Barrett’s esophagus, erosive esophagitis, and gastroesophageal reflux symptoms. Clin Gastroenterol Hepatol. 2014; 12:239–245. PMID: 23988686.13. Lee SY, Moon HW, Hur M, Yun YM. Validation of western Helicobacter pylori IgG antibody assays in Korean adults. J Med Microbiol. 2015; 64:513–518. PMID: 25752852.14. Iijima K, Kanno T, Koike T, Shimosegawa T. Helicobacter pylori-negative, non-steroidal anti-inflammatory drug: negative idiopathic ulcers in Asia. World J Gastroenterol. 2014; 20:706–713. PMID: 24574744.15. Lee JY, Kim N, Lee HS, Oh JC, Kwon YH, Choi YJ, Yoon KC, Hwang JJ, Lee HJ, Lee A, et al. Correlations among endoscopic, histologic and serologic diagnoses for the assessment of atrophic gastritis. J Cancer Prev. 2014; 19:47–55. PMID: 25337572.16. Song HJ, Shim KN, Yoon SJ, Kim SE, Oh HJ, Ryu KH, Ha CY, Yeom HJ, Song JH, Jung SA, et al. The prevalence and clinical characteristics of reflux esophagitis in Koreans and its possible relation to metabolic syndrome. J Korean Med Sci. 2009; 24:197–202. PMID: 19399258.17. Kitamura Y, Yoshihara M, Ito M, Boda T, Matsuo T, Kotachi T, Tanaka S, Chayama K. Diagnosis of Helicobacter pylori-induced gastritis by serum pepsinogen levels. J Gastroenterol Hepatol. 2015; 30:1473–1477. PMID: 25974661.18. Tu H, Sun L, Dong X, Gong Y, Xu Q, Jing J, Long Q, Flanders WD, Bostick RM, Yuan Y. Temporal changes in serum biomarkers and risk for progression of gastric precancerous lesions: a longitudinal study. Int J Cancer. 2015; 136:425–434. PMID: 24895149.19. Chae H, Lee JH, Lim J, Kim M, Kim Y, Han K, Kang CS, Shim SI, Kim JI, Park SH. Clinical utility of serum pepsinogen levels as a screening test of atrophic gastritis. Korean J Lab Med. 2008; 28:201–206. PMID: 18594172.20. Kim EH, Kang H, Park CH, Choi HS, Jung DH, Chung H, Park JC, Shin SK, Lee SK, Lee YC. The optimal serum pepsinogen cut-off value for predicting histologically confirmed atrophic gastritis. Dig Liver Dis. 2015; 47:663–668. PMID: 26077884.21. He CY, Sun LP, Gong YH, Xu Q, Dong NN, Yuan Y. Serum pepsinogen II: a neglected but useful biomarker to differentiate between diseased and normal stomachs. J Gastroenterol Hepatol. 2011; 26:1039–1046. PMID: 21303408.22. Gritti I, Banfi G, Roi GS. Pepsinogens: physiology, pharmacology pathophysiology and exercise. Pharmacol Res. 2000; 41:265–281. PMID: 10675278.23. Seo JH, Lim CW, Park JS, Yeom JS, Lim JY, Jun JS, Woo HO, Youn HS, Baik SC, Lee WK, et al. Correlations between the CagA antigen and serum levels of anti-Helicobacter pylori IgG and IgA in children. J Korean Med Sci. 2016; 31:417–422. PMID: 26955243.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serum Pepsinogen l, ll Levels and Upper Gastrointestinal Diseases in Children with H. pylori Infection
- Serum gastrin and pepsinogen I, II concentrations in children with Helicobacter pylori infection: the role of CagA and VacA
- Changing Trends of Serum Pepsinogen I/II Ratio in Asymptomatic Subjects
- Endoscopic gastritis, serum pepsinogen assay, and Helicobacter pylori infection
- Gastric red spots and serum pepsinogen I levels in cirrhotic patients