J Korean Neurosurg Soc.
2017 Feb;60(2):189-194. 10.3340/jkns.2016.0909.003.
Bone Cement-Augmented Percutaneous Screw Fixation for Malignant Spinal Metastases: Is It Feasible?
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Chosun University, Gwangju, Korea. chosunns@chosun.ac.kr
- KMID: 2374880
- DOI: http://doi.org/10.3340/jkns.2016.0909.003
Abstract
OBJECTIVE
We evaluated the validity of bone cement-augmented percutaneous screw fixation for treating malignant spinal metastases.
METHODS
Between 2011 and 2015, 14 patients (eight men and six women) who underwent bone cement-augmented percutaneous screw fixation for malignant spinal metastases were enrolled in this study. Their life expectancy was considered to be more than one month and less than one year, based on the revised Tokuhashi scoring system. Clinical findings including the back pain scale score, functional outcome, procedure related complications, and survival were assessed preoperatively, postoperatively, and then six months after the procedure.
RESULTS
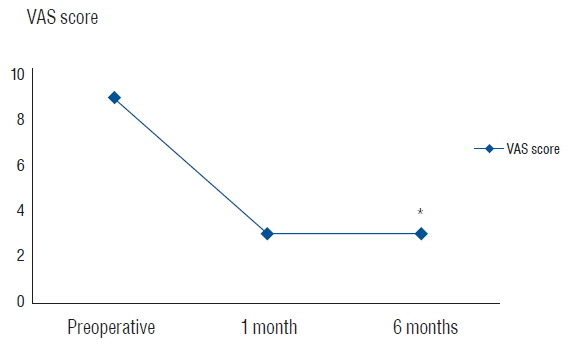
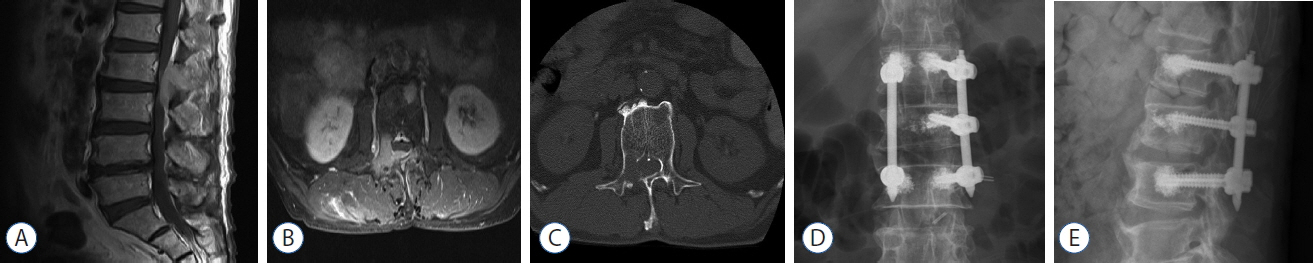
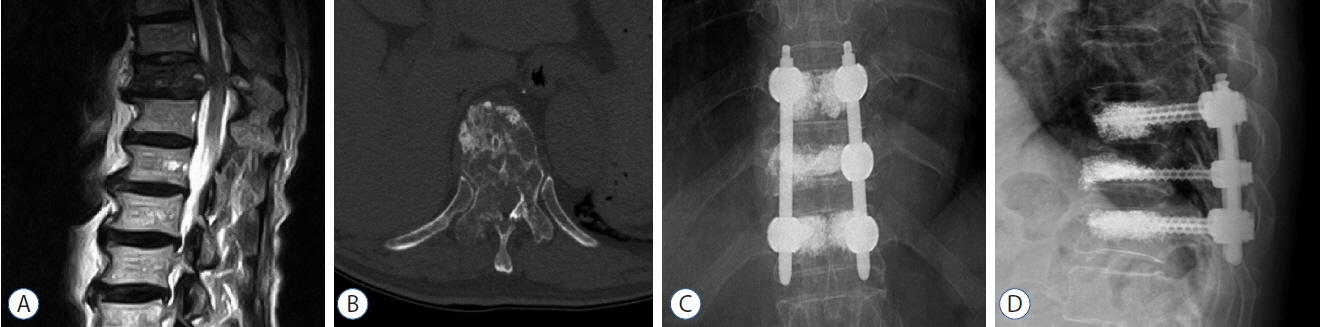
Twelve of the patients (86%) survived up to six months after the procedure. Three required mini-open decompressive laminectomy for severe epidural compression. Bone cement-augmented percutaneous screw fixation was performed one level above, one level below, and at the pathologic level itself. The mean operation time was 60 minutes (45-180) and blood loss was less than 100 mL. Prior to surgery, the mean pain score on the visual analogue scale was 8.8, while one month after the procedure, it had reduced to 3.0; this improvement was maintained until the six-month assessment in the surviving patients. All patients were able to sit within the first two days after surgery, and no patient experienced neurological deterioration at the one-month follow up after the surgery. No patient experienced screw loosening during the six months of follow-up. Asymptomatic cement leakage into the epidural space was observed in two patients, but no major complications were observed.
CONCLUSION
For selected patients with malignant spinal metastases, bone cement-augmented percutaneous screw fixation can provide significant pain relief and improve quality of life.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Berenson J, Pflugmacher R, Jarzem P, Zonder J, Schechtman K, Tillman JB, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol. 12:225–235. 2011.
Article2. Böhm P, Huber J. The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Surg Br. 84:521–529. 2002.
Article3. Burval DJ, McLain RF, Milks R, Inceoglu S. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976). 32:1077–1083. 2007.4. Falicov A, Fisher CG, Sparkes J, Boyd MC, Wing PC, Dvorak MF. Impact of surgical intervention on quality of life in patients with spinal metastases. Spine (Phila Pa 1976). 31:2849–2856. 2006.
Article5. Fourney DR, Schomer DF, Nader R, Chlan-Fourney J, Suki D, Ahrar K, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg. 98(1 Suppl):21–30. 2003.
Article6. Harrington K. Metastatic tumors of the spine: Diagnosis and treatment. J Am Acad Orthop Surg. 1:76–86. 1993.
Article7. Kim CH, Chung CK, Sohn S, Lee S, Park SB. Less invasive palliative surgery for spinal metastases. J Surg Oncol. 108:499–503. 2013.
Article8. Kim SK, Chung JY, Cho CB, Choi HC. Percutaneous anterolateral vertebroplasty for a myelomatous pathologic fracture of the subaxial cervical spine: A case report. Korean J Spine. 8:225–228. 2011.
Article9. Lee CG, Kim SH, Kim DM, Kim SW. Giant cell tumor of upper thoracic spine. J Korean Neurosurg Soc. 55:167–169. 2014.
Article10. Park HY, Lee SH, Park SJ, Kim ES, Lee CS, Eoh W. Minimally invasive option using percutaneous pedicle screw for instability of metastasis involving thoracolumbar and lumbar spine: a case series in a single center. J Korean Neurosurg Soc. 57:100–107. 2015.
Article11. Sawakami K, Yamazaki A, Ishikawa S, Ito T, Watanabe K, Endo N. Polymethylmethacrylate augmentation of pedicle screws increases the initial fixation in osteoporotic spine patients. J Spinal Disord Tech. 25:28–35. 2012.
Article12. Sun G, Li L, Jin P, Liu XW, Li M. Percutaneous vertebroplasty for painful spinal metastasis with epidural encroachment. J Surg Oncol. 110:123–128. 2014.
Article13. Tancioni F, Navarria P, Pessina F, Marcheselli S, Rognone E, Mancosu P, et al. Early surgical experience with minimally invasive percutaneous approach for patients with metastatic epidural spinal cord compression (MESCC) to poor prognoses. Ann Surg Oncol. 19:294–300. 2012.
Article14. Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 30:2186–2191. 2005.
Article15. Zairi F, Arikat A, Allaoui M, Marinho P, Assaker R. Minimally invasive decompression and stabilization for the management of thoracolumbar spine metastasis. J Neurosurg Spine. 17:19–23. 2012.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Screw Fixation in Previously Augmented Vertebrae with Bone Cement: Is It Inapplicable?
- Clinical Efficacy of Bone Cement Augmented Screw Fixation for the Severe Osteoporotic Spine
- Cardiac Perforation Caused by Bone Cements as a Complication of Cement Augmented Pedicle Screw Fixation Using the Fenestrated Pedicle Screw: A Case Report
- Bone Cement Augmented Screw Fixation for Severe Osteoporotic Spine: Large Series of Clinical Application
- Percutaneous Iliosacral Screw Fixation with Cement Augmentation in Sacral Insufficient Fracture: A Case Report