Yonsei Med J.
2017 Jan;58(1):187-194. 10.3349/ymj.2017.58.1.187.
Costs Attributable to Overweight and Obesity in Working Asthma Patients in the United States
- Affiliations
-
- 1College of Pharmacy, Chung-Ang University, Seoul, Korea. dongsuh75@gmail.com
- 2Department of Internal Medicine, College of Medicine, Chung-Ang University, Seoul, Korea.
- KMID: 2374206
- DOI: http://doi.org/10.3349/ymj.2017.58.1.187
Abstract
- PURPOSE
To estimate annual health care and productivity loss costs attributable to overweight or obesity in working asthmatic patients.
MATERIALS AND METHODS
This study was conducted using the 2003-2013 Medical Expenditure Panel Survey (MEPS) in the United States. Patients aged 18 to 64 years with asthma were identified via self-reported diagnosis, a Clinical Classification Code of 128, or a ICD-9-CM code of 493.xx. All-cause health care costs were estimated using a generalized linear model with a log function and a gamma distribution. Productivity loss costs were estimated in relation to hourly wages and missed work days, and a two-part model was used to adjust for patients with zero costs. To estimate the costs attributable to overweight or obesity in asthma patients, costs were estimated by the recycled prediction method.
RESULTS
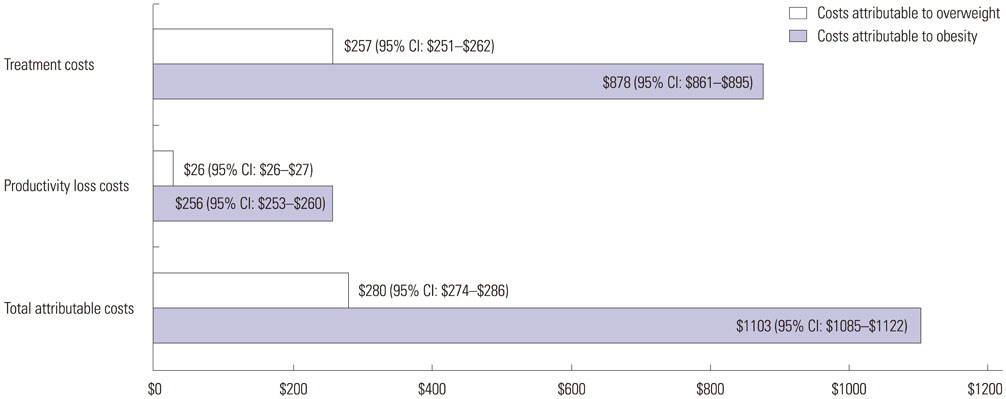
Among 11670 working patients with a diagnosis of asthma, 4428 (35.2%) were obese and 3761 (33.0%) were overweight. The health care costs attributable to obesity and overweight in working asthma patients were estimated to be $878 [95% confidence interval (CI): $861-$895] and $257 (95% CI: $251-$262) per person per year, respectively, from 2003 to 2013. The productivity loss costs attributable to obesity and overweight among working asthma patients were $256 (95% CI: $253-$260) and $26 (95% CI: $26-$27) per person per year, respectively.
CONCLUSION
Health care and productivity loss costs attributable to overweight and obesity in asthma patients are substantial. This study's results highlight the importance of effective public health and educational initiatives targeted at reducing overweight and obesity among patients with asthma, which may help lower the economic burden of asthma.
MeSH Terms
Figure
Reference
-
1. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Summary Health Statistics for U.S. Children: National Health Interview Survey, 2012. 2013. accessed on 2016 March 15. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_258.pdf.2. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2012. 2014. accessed on 2016 March 15. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_260.pdf.3. Kamble S, Bharmal M. Incremental direct expenditure of treating asthma in the United States. J Asthma. 2009; 46:73–80.
Article4. Sullivan PW, Ghushchyan VH, Slejko JF, Belozeroff V, Globe DR, Lin SL. The burden of adult asthma in the United States: evidence from the Medical Expenditure Panel Survey. J Allergy Clin Immunol. 2011; 127:363–369.
Article5. Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002-2007. J Allergy Clin Immunol. 2011; 127:145–152.
Article6. Jang J, Gary Chan KC, Huang H, Sullivan SD. Trends in cost and outcomes among adult and pediatric patients with asthma: 2000-2009. Ann Allergy Asthma Immunol. 2013; 111:516–522.
Article7. Cisternas MG, Blanc PD, Yen IH, Katz PP, Earnest G, Eisner MD, et al. A comprehensive study of the direct and indirect costs of adult asthma. J Allergy Clin Immunol. 2003; 111:1212–1218.
Article8. Trogdon JG, Finkelstein EA, Feagan CW, Cohen JW. State- and payer-specific estimates of annual medical expenditures attributable to obesity. Obesity (Silver Spring). 2012; 20:214–220.
Article9. Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011; 12:131–141.
Article10. Sarpong EM. The impact of obesity on medication use and expenditures among nonelderly adults with asthma. J Health Care Poor Underserved. 2014; 25:1245–1261.
Article11. Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009; 28:w822–w831.
Article12. Cawley J, Rizzo JA, Haas K. Occupation-specific absenteeism costs associated with obesity and morbid obesity. J Occup Environ Med. 2007; 49:1317–1324.
Article13. Sullivan PW, Ghushchyan V, Ben-Joseph RH. The effect of obesity and cardiometabolic risk factors on expenditures and productivity in the United States. Obesity (Silver Spring). 2008; 16:2155–2162.
Article14. Pakhale S, Doucette S, Vandemheen K, Boulet LP, McIvor RA, Fitzgerald JM, et al. A comparison of obese and nonobese people with asthma: exploring an asthma-obesity interaction. Chest. 2010; 137:1316–1323.
Article15. Taylor B, Mannino D, Brown C, Crocker D, Twum-Baah N, Holguin F. Body mass index and asthma severity in the National Asthma Survey. Thorax. 2008; 63:14–20.
Article16. Saint-Pierre P, Bourdin A, Chanez P, Daures JP, Godard P. Are overweight asthmatics more difficult to control? Allergy. 2006; 61:79–84.
Article17. Peters-Golden M, Swern A, Bird SS, Hustad CM, Grant E, Edelman JM. Influence of body mass index on the response to asthma controller agents. Eur Respir J. 2006; 27:495–503.
Article18. Lavoie KL, Bacon SL, Labrecque M, Cartier A, Ditto B. Higher BMI is associated with worse asthma control and quality of life but not asthma severity. Respir Med. 2006; 100:648–657.
Article19. Rodrigo GJ, Plaza V. Body mass index and response to emergency department treatment in adults with severe asthma exacerbations: a prospective cohort study. Chest. 2007; 132:1513–1519.
Article20. Mosen DM, Schatz M, Magid DJ, Camargo CA Jr. The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol. 2008; 122:507–511.
Article21. Shah R, Yang Y. Health and economic burden of obesity in elderly individuals with asthma in the United States. Popul Health Manag. 2015; 18:186–191.
Article22. Agency for Healthcare Research and Quality. MEPS HC-163: 2013 Full Year Consolidated Data File. 2015. accessed on 2016 March 31. Available at: http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h163/h163doc.pdf.23. United States Bureau of Labor Statistics. May 2015 national occupational employment and wage estimates United States. accessed on 2016 March 15. Available at: http://www.bls.gov/oes/current/oes_nat.htm.24. Sullivan PW, Ghushchyan V, Wyatt HR, Wu EQ, Hill JO. Productivity costs associated with cardiometabolic risk factor clusters in the United States. Value Health. 2007; 10:443–450.
Article25. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010; 303:235–241.
Article26. Valerio MA, Gong ZM, Wang S, Bria WF, Johnson TR, Clark NM. Overweight women and management of asthma. Womens Health Issues. 2009; 19:300–305.
Article27. Honeycutt AA, Segel JE, Hoerger TJ, Finkelstein EA. Comparing cost-of-illness estimates from alternative approaches: an application to diabetes. Health Serv Res. 2009; 44:303–320.
Article28. Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004; 23:525–542.29. Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001; 20:461–494.
Article30. Duan N, Manning WG Jr, Morris CN, Newhouse JP. A comparison of alternative models for the demand for medical care. J Bus Econ Stat. 1983; 1:115–126.
Article31. Basu A, Rathouz PJ. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics. 2005; 6:93–109.
Article32. Basu A, Arondekar BV, Rathouz PJ. Scale of interest versus scale of estimation: comparing alternative estimators for the incremental costs of a comorbidity. Health Econ. 2006; 15:1091–1107.
Article33. Mullahy J. Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J Health Econ. 1998; 17:247–281.
Article34. United States Bureau of Labor Statistics. Consumer price indexes. accessed on 2016 March 31. Available at: http://www.bls.gov/cpi/.35. Carrier E, Cunningham P. Medical cost burdens among nonelderly adults with asthma. Am J Manag Care. 2014; 20:925–932.36. Maniscalco M, Zedda A, Faraone S, Cerbone MR, Cristiano S, Giardiello C, et al. Weight loss and asthma control in severely obese asthmatic females. Respir Med. 2008; 102:102–108.
Article37. Hakala K, Stenius-Aarniala B, Sovijärvi A. Effects of weight loss on peak flow variability, airways obstruction, and lung volumes in obese patients with asthma. Chest. 2000; 118:1315–1321.
Article38. Stenius-Aarniala B, Poussa T, Kvarnström J, Grönlund EL, Ylikahri M, Mustajoki P. Immediate and long term effects of weight reduction in obese people with asthma: randomised controlled study. BMJ. 2000; 320:827–832.
Article39. Trogdon JG, Finkelstein EA, Hylands T, Dellea PS, Kamal-Bahl SJ. Indirect costs of obesity: a review of the current literature. Obes Rev. 2008; 9:489–500.
Article40. Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012; 31:219–230.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Morbidities from Lack of Exercise and the Socioeconomic Effects
- Medical Expenditure Attributable to Overweight and Obesity in Adults with Hypertension, Diabetes and Dyslipidemia : Evidence from Korea National Health and Nutrition Examination Survey Data and Korea National Health Corporation Data
- Asthma and obesity: Is asthma a risk factor for obesity?
- Socioeconomic Costs of Overweight and Obesity in Korean Adults
- Current Status of Bariatric Endoscopy in Obesity Control