Yonsei Med J.
2016 Mar;57(2):388-392. 10.3349/ymj.2016.57.2.388.
Deep Vein Thrombosis in the Lower Extremities in Comatose Elderly Patients with Acute Neurological Diseases
- Affiliations
-
- 1Department of Neurosurgery, Teikyo University Mizonokuchi Hospital, Kawasaki, Japan. merrityamada@hotmail.co.jp
- KMID: 2374044
- DOI: http://doi.org/10.3349/ymj.2016.57.2.388
Abstract
- PURPOSE
Comatose elderly patients with acute neurological illness have a great risk of deep vein thrombosis (DVT). In this study, the incidence of DVT and the effectiveness of early initiation of treatment were evaluated in those patients.
MATERIALS AND METHODS
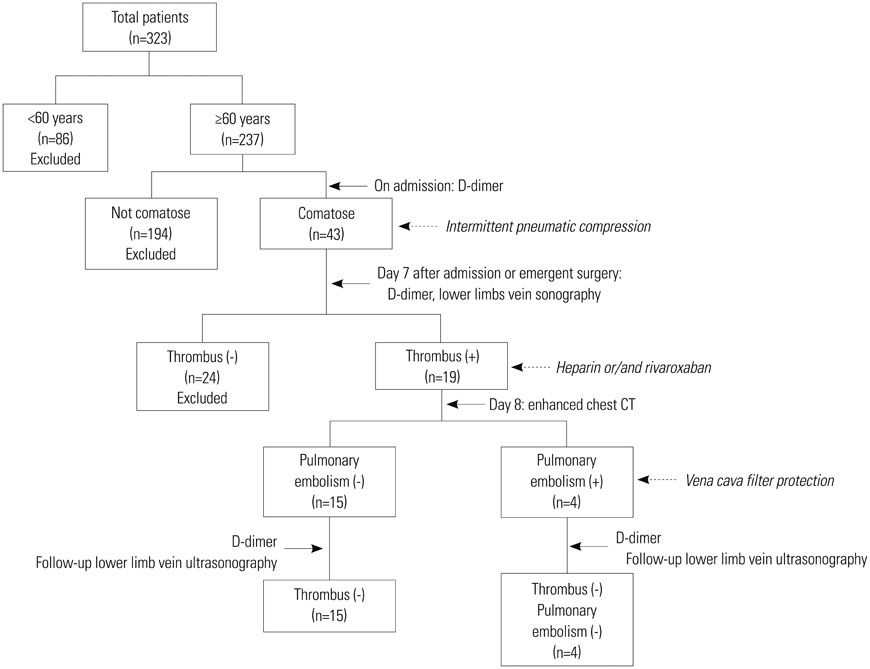
Total 323 patients were admitted to our ward due to neurological diseases in one year, and 43 patients, whose Glasgow Coma Scale was < or =11 and who was older than > or =60 years, were included in this study. D-dimer was measured on admission and day 7, and lower-extremity ultrasonography was performed on day 7. When DVT was positive, heparin treatment was initiated, and further evaluation of pulmonary embolism (PE) was conducted. Vena cava filter protection was inserted in PE-positive patients. Incidence of DVT and PE, alteration of D-dimer value, and effect of heparin treatment were analyzed.
RESULTS
DVT was positive in 19 (44.2%) patients, and PE was in 4 (9.3%). D-dimer was significantly higher in DVT-positive group on day 7 (p<0.01). No DVT were identified in patients with ischemic disease, while 66.7% of intracerebral hemorrhage and 53.3% of brain contusion patients were DVT positive. Surgery was a definite risk factor for DVT, with an odds ratio of 5.25. DVT and PE disappeared by treatment in all cases, and no patients were succumbed to the thrombosis.
CONCLUSION
Patients with hemorrhagic diseases or who undergo operation possess high risk of DVT, and initiation of heparin treatment in 7 days after admission is an effective prophylaxis for DVT in comatose elderly patients without causing bleeding.
Keyword
MeSH Terms
-
Acute Disease
Aged
Anticoagulants/adverse effects/therapeutic use
Antifibrinolytic Agents/therapeutic use
*Coma
Female
Fibrin Fibrinogen Degradation Products/therapeutic use
Hemorrhage/*epidemiology
Heparin/adverse effects/therapeutic use
Humans
Incidence
Japan/epidemiology
Lower Extremity
Male
Middle Aged
Nervous System Diseases/epidemiology
Neurosurgical Procedures/*adverse effects
Pulmonary Embolism/*complications/epidemiology/prevention & control
Risk Factors
Venous Thrombosis/epidemiology/*etiology/prevention & control
Anticoagulants
Antifibrinolytic Agents
Fibrin Fibrinogen Degradation Products
Heparin
Figure
Reference
-
1. Heit JA, Melton LJ 3rd, Lohse CM, Petterson TM, Silverstein MD, Mohr DN, et al. Incidence of venous thromboembolism in hospitalized patients vs community residents. Mayo Clin Proc. 2001; 76:1102–1110.
Article2. Longo MG, Greco A, Pacilli M, D'Ambrosio LP, Scarcelli C, Grandone E, et al. Deep venous thrombosis in elderly hospitalized patients: prevalence and clinical features. Aging Clin Exp Res. 2005; 17:42–45.
Article3. Jaffer AK, Brotman DJ. Prevention of venous thromboembolism in the geriatric patient. Clin Geriatr Med. 2006; 22:93–111, ix.
Article4. Rogers RL. Venous thromboembolic disease in the elderly patient: atypical, subtle, and enigmatic. Clin Geriatr Med. 2007; 23:413–423, viii.
Article5. Heit JA. The epidemiology of venous thromboembolism in the community: implications for prevention and management. J Thromb Thrombolysis. 2006; 21:23–29.
Article6. Nokes TJ, Keenan J. Thromboprophylaxis in patients with lower limb immobilisation - review of current status. Br J Haematol. 2009; 146:361–368.
Article7. Rosendaal FR, Reitsma PH. Genetics of venous thrombosis. J Thromb Haemost. 2009; 7:Suppl 1. 301–304.
Article8. Tichelaar YI, Kluin-Nelemans HJ, Meijer K. Infections and inflammatory diseases as risk factors for venous thrombosis. A systematic review. Thromb Haemost. 2012; 107:827–837.
Article9. Wong P, Baglin T. Epidemiology, risk factors and sequelae of venous thromboembolism. Phlebology. 2012; 27:Suppl 2. 2–11.
Article10. Kraft C, Schuettfort G, Weil Y, Tirneci V, Kasper A, Haberichter B, et al. Thrombosis of the inferior vena cava and malignant disease. Thromb Res. 2014; 134:668–673.
Article11. Zarowitz BJ, Tangalos E, Lefkovitz A, Bussey H, Deitelzweig S, Nutescu E, et al. Thrombotic risk and immobility in residents of longterm care facilities. J Am Med Dir Assoc. 2010; 11:211–221.
Article12. Enders JM, Burke JM, Dobesh PP. Prevention of venous thromboembolism in acute medical illness. Pharmacotherapy. 2002; 22:1564–1578.
Article13. Lacherade JC, Cook D, Heyland D, Chrusch C, Brochard L, Brun-Buisson C. French and Canadian ICU Directors Groups. Prevention of venous thromboembolism in critically ill medical patients: a Franco-Canadian cross-sectional study. J Crit Care. 2003; 18:228–237.
Article14. McGarry LJ, Thompson D. Retrospective database analysis of the prevention of venous thromboembolism with low-molecular-weight heparin in acutely III medical inpatients in community practice. Clin Ther. 2004; 26:419–430.
Article15. Spencer A, Cawood T, Frampton C, Jardine D. Heparin-based treatment to prevent symptomatic deep venous thrombosis, pulmonary embolism or death in general medical inpatients is not supported by best evidence. Intern Med J. 2014; 44:1054–1065.
Article16. Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003; 349:1227–1235.
Article17. Perrier A. Review: the Wells clinical prediction guide and D-dimer testing predict deep venous thrombosis. ACP J Club. 2006; 145:24.
Article18. Hogg K, Wells PS, Gandara E. The diagnosis of venous thromboembolism. Semin Thromb Hemost. 2012; 38:691–701.
Article19. Tenna AM, Kappadath S, Stansby G. Diagnostic tests and strategies in venous thromboembolism. Phlebology. 2012; 27:Suppl 2. 43–52.
Article20. Wells P, Anderson D. The diagnosis and treatment of venous thromboembolism. Hematology Am Soc Hematol Educ Program. 2013; 2013:457–463.
Article21. André C, de Freitas GR, Fukujima MM. Prevention of deep venous thrombosis and pulmonary embolism following stroke: a systematic review of published articles. Eur J Neurol. 2007; 14:21–32.
Article22. Vespa P. Participants in the International Multi-Disciplinary Consensus Conference on the Critical Care Management of Subarachnoid Hemorrhage. Deep venous thrombosis prophylaxis. Neurocrit Care. 2011; 15:295–297.
Article23. Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E. Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal. Health Technol Assess. 2009; 13:Suppl 3. 43–48.
Article24. Turpie AG, Kreutz R, Llau J, Norrving B, Haas S. Management consensus guidance for the use of rivaroxaban--an oral, direct factor Xa inhibitor. Thromb Haemost. 2012; 108:876–886.
Article25. Bembenek JP, Karlinski M, Kobayashi A, Czlonkowska A. Deep venous thrombosis in acute stroke patients. Clin Appl Thromb Hemost. 2012; 18:258–264.
Article26. Weill-Engerer S, Meaume S, Lahlou A, Piette F, Saint-Jean O, Sachet A, et al. Risk factors for deep vein thrombosis in inpatients aged 65 and older: a case-control multicenter study. J Am Geriatr Soc. 2004; 52:1299–1304.
Article27. Kniffin WD Jr, Baron JA, Barrett J, Birkmeyer JD, Anderson FA Jr. The epidemiology of diagnosed pulmonary embolism and deep venous thrombosis in the elderly. Arch Intern Med. 1994; 154:861–866.
Article28. Di Minno G, Tufano A. Challenges in the prevention of venous thromboembolism in the elderly. J Thromb Haemost. 2004; 2:1292–1298.
Article29. Keenan CR, White RH. Age as a risk factor for venous thromboembolism after major surgery. Curr Opin Pulm Med. 2005; 11:398–402.
Article30. Kearon C. Natural history of venous thromboembolism. Circulation. 2003; 107:23 Suppl 1. I22–I30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Contrast Enhanced Rapid MR Sequence(True FISP) in Deep Vein Thrombosis
- The Incidence of Deep Vein Thrombosis in the Lower Extremity
- A Case of Upper Extremity Deep Vein Thrombosis and Pulmonary Thromboembolism in a Severely Obese Man
- Fibrinolytic Activity in Patients with Deep Vein Thrombosis
- An Acute Pulmonary Embolism Accompanying Greater Saphenous Vein Thrombosis