Yonsei Med J.
2016 Mar;57(2):306-312. 10.3349/ymj.2016.57.2.306.
Hemodynamic Follow-Up in Adult Patients with Pulmonary Hypertension Associated with Atrial Septal Defect after Partial Closure
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. herzhuh@skku.edu
- 2Department of Pediatrics, Sejong General Hospital, Sejong Cardiovascular Center, Bucheon, Korea.
- 3Department of Thoracic Surgery, Sejong General Hospital, Sejong Cardiovascular Center, Bucheon, Korea.
- 4Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2374033
- DOI: http://doi.org/10.3349/ymj.2016.57.2.306
Abstract
- PURPOSE
We evaluated the hemodynamic statuses of patients after partial closure of atrial septal defects with fenestration due to pulmonary hypertension.
MATERIALS AND METHODS
Seventeen adult patients underwent partial atrial septal defect closure and follow-up cardiac catheterization. We analyzed hemodynamic data and clinical parameters before and after closure.
RESULTS
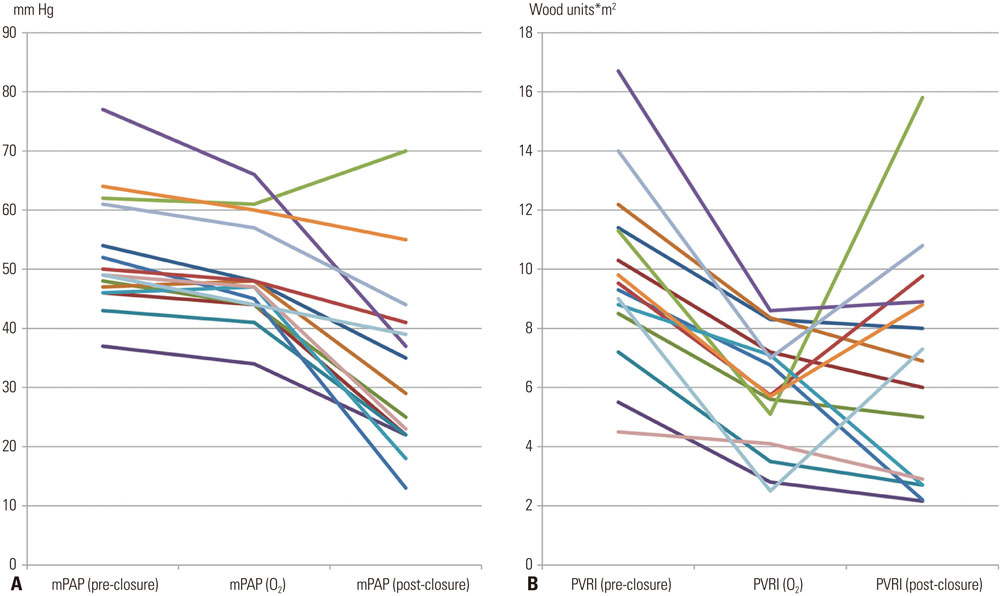
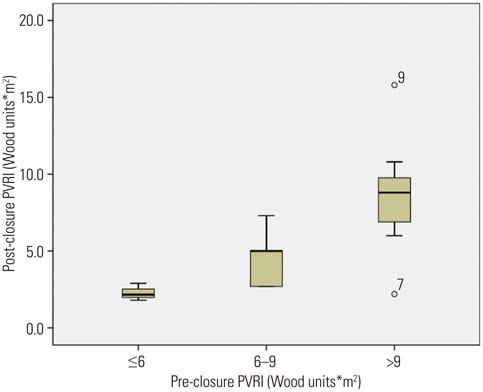
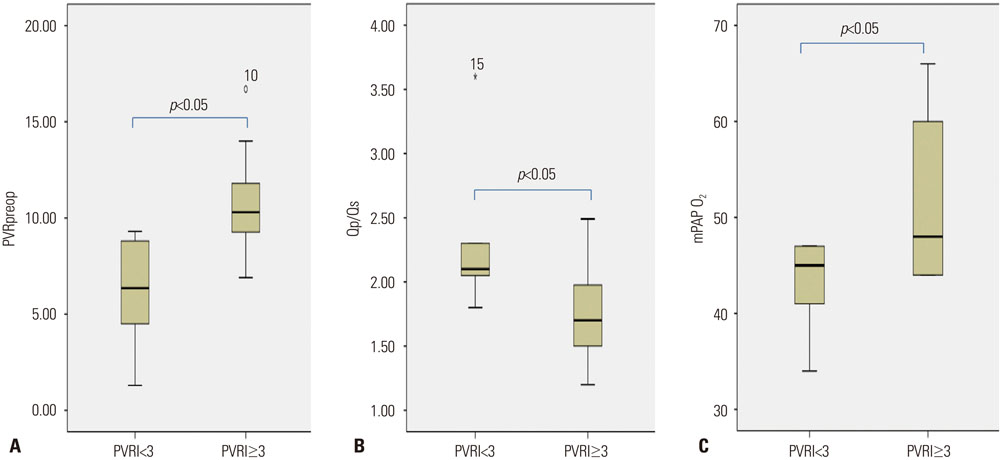
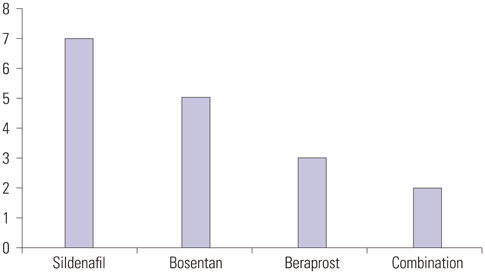
The median age at closure was 29 years old. The baseline Qp/Qs was 1.9+/-0.6. The median interval from the operation to the cardiac catheterization was 27 months. The CT ratio decreased from 0.55+/-0.07 to 0.48+/-0.06 (p<0.05). The mean pulmonary arterial pressure decreased from 50.0+/-11.5 mm Hg to 32.5+/-14.4 mm Hg (p<0.05), and the pulmonary resistance index decreased from 9.2+/-3.6 Wood units*m2 to 6.3+/-3.8 Wood units*m2 (p<0.05). Eleven patients (64.7%) continued to exhibit high pulmonary resistance (over 3.0 Wood units*m2) after closure. These patients had significantly higher pulmonary resistance indices and mean pulmonary arterial pressures based on oxygen testing before the partial closures (p<0.05). However, no significant predictors of post-closure pulmonary hypertension were identified.
CONCLUSION
Despite improvement in symptoms and hemodynamics after partial closure of an atrial septal defect, pulmonary hypertension should be monitored carefully.
Keyword
MeSH Terms
-
Adult
Aged
Cardiac Catheterization/*adverse effects
Female
Follow-Up Studies
Heart Defects, Congenital/epidemiology/*physiopathology/*surgery
Heart Septal Defects, Atrial/surgery
Hemodynamics/*physiology
Humans
Hypertension, Pulmonary/diagnosis/epidemiology/*physiopathology
Male
Middle Aged
Oxygen
Postoperative Complications/diagnosis/epidemiology/*physiopathology
Retrospective Studies
Treatment Outcome
Young Adult
Oxygen
Figure
Reference
-
1. van Loon RL, Roofthooft MT, Hillege HL, ten Harkel AD, van Osch-Gevers M, Delhaas T, et al. Pediatric pulmonary hypertension in the Netherlands: epidemiology and characterization during the period 1991 to 2005. Circulation. 2011; 124:1755–1764.
Article2. Baumgartner H, Bonhoeffer P, De Groot NM, de Haan F, Deanfield JE, Galie N, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010; 31:2915–2957.
Article3. Beghetti M, Galiè N, Bonnet D. Can "inoperable" congenital heart defects become operable in patients with pulmonary arterial hypertension? Dream or reality? Congenit Heart Dis. 2012; 7:3–11.
Article4. Lopes AA, O'Leary PW. Measurement, interpretation and use of hemodynamic parameters. Cardiol Young. 2009; 19:Suppl 1. 8–12.
Article5. Hörer J, Müller S, Schreiber C, Kostolny M, Cleuziou J, Prodan Z, et al. Surgical closure of atrial septal defect in patients older than 30 years: risk factors for late death from arrhythmia or heart failure. Thorac Cardiovasc Surg. 2007; 55:79–83.
Article6. Steele PM, Fuster V, Cohen M, Ritter DG, McGoon DC. Isolated atrial septal defect with pulmonary vascular obstructive disease--long-term follow-up and prediction of outcome after surgical correction. Circulation. 1987; 76:1037–1042.
Article7. Beghetti M, Galiè N. Eisenmenger syndrome a clinical perspective in a new therapeutic era of pulmonary arterial hypertension. J Am Coll Cardiol. 2009; 53:733–740.8. Hirabayashi A, Miyaji K, Akagi T. Continuous epoprostenol therapy and septal defect closure in a patient with severe pulmonary hypertension. Catheter Cardiovasc Interv. 2009; 73:688–691.
Article9. Althoff TF, Knebel F, Panda A, McArdle J, Gliech V, Franke I, et al. Long-term follow-up of a fenestrated Amplatzer atrial septal occluder in pulmonary arterial hypertension. Chest. 2008; 133:283–285.
Article10. Bruch L, Winkelmann A, Sonntag S, Scherf F, Rux S, Grad MO, et al. Fenestrated occluders for treatment of ASD in elderly patients with pulmonary hypertension and/or right heart failure. J Interv Cardiol. 2008; 21:44–49.
Article11. Cho YH, Jun TG, Yang JH, Park PW, Huh J, Kang IS, et al. Surgical strategy in patients with atrial septal defect and severe pulmonary hypertension. Heart Surg Forum. 2012; 15:E111–E115.
Article12. Kyle WB. Pulmonary hypertension associated with congenital heart disease: a practical review for the pediatric cardiologist. Congenit Heart Dis. 2012; 7:575–583.
Article13. McLaughlin VV, Archer SL, Badesch DB, Barst RJ, Farber HW, Lindner JR, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol. 2009; 53:1573–1619.14. Berger RM, Beghetti M, Galiè N, Gatzoulis MA, Granton J, Lauer A, et al. Atrial septal defects versus ventricular septal defects in BREATHE-5, a placebo-controlled study of pulmonary arterial hypertension related to Eisenmenger's syndrome: a subgroup analysis. Int J Cardiol. 2010; 144:373–378.
Article15. Dimopoulos K, Inuzuka R, Goletto S, Giannakoulas G, Swan L, Wort SJ, et al. Improved survival among patients with Eisenmenger syndrome receiving advanced therapy for pulmonary arterial hypertension. Circulation. 2010; 121:20–25.
Article16. Galiè N, Beghetti M, Gatzoulis MA, Granton J, Berger RM, Lauer A, et al. Bosentan therapy in patients with Eisenmenger syndrome: a multicenter, double-blind, randomized, placebo-controlled study. Circulation. 2006; 114:48–54.17. Barst RJ, Agnoletti G, Fraisse A, Baldassarre J, Wessel DL. NO Diagnostic Study Group. Vasodilator testing with nitric oxide and/or oxygen in pediatric pulmonary hypertension. Pediatr Cardiol. 2010; 31:598–606.
Article18. Sánchez-Recalde A, Oliver JM, Galeote G, González A, Calvo L, Jiménez-Valero S, et al. Atrial septal defect with severe pulmonary hypertension in elderly patients: usefulness of transient balloon occlusion. Rev Esp Cardiol. 2010; 63:860–864.
Article19. Dell'avvocata F, Rigatelli G, Cardaioli P, Giordan M. Home-made fenestrated amplatzer occluder for atrial septal defect and pulmonary arterial hypertension. J Geriatr Cardiol. 2011; 8:127–129.20. Yong G, Khairy P, De Guise P, Dore A, Marcotte F, Mercier LA, et al. Pulmonary arterial hypertension in patients with transcatheter closure of secundum atrial septal defects: a longitudinal study. Circ Cardiovasc Interv. 2009; 2:455–462.
Article21. D'Alto M, Romeo E, Argiento P, Correra A, Santoro G, Gaio G, et al. Hemodynamics of patients developing pulmonary arterial hypertension after shunt closure. Int J Cardiol. 2013; 168:3797–3801.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subacute, Silent Embolization of Amplatzer Atrial Septal Defect Closure Device to the Pulmonary Artery
- Large Atrial Septal Defect Closure in a Patient with Severe Pulmonary Arterial Hypertension
- Device Closure of a Large Atrial Septal Defect in a Patient with Severe Pulmonary Arterial Hypertension after 1 Year Use of an Oral Endothelin Receptor Antagonist
- Surgical Extraction of an Embolized Atrial Septal Defect Occluder Device into Pulmonary Artery after Percutaneous Closure
- Comparison of Efficacy of Transcatheter Closure of Atrial Septal Defect with Amplatzer Septal Occluder between Children and Adult