J Korean Soc Radiol.
2017 Apr;76(4):294-297. 10.3348/jksr.2017.76.4.294.
Hemichorea-Hemiballismus Associated with Hyperglycemia: A Case Report
- Affiliations
-
- 1Department of Radiology, Busan Paik Hospital, Inje University, Busan, Korea. hwjeong2000@lycos.co.kr
- KMID: 2373968
- DOI: http://doi.org/10.3348/jksr.2017.76.4.294
Abstract
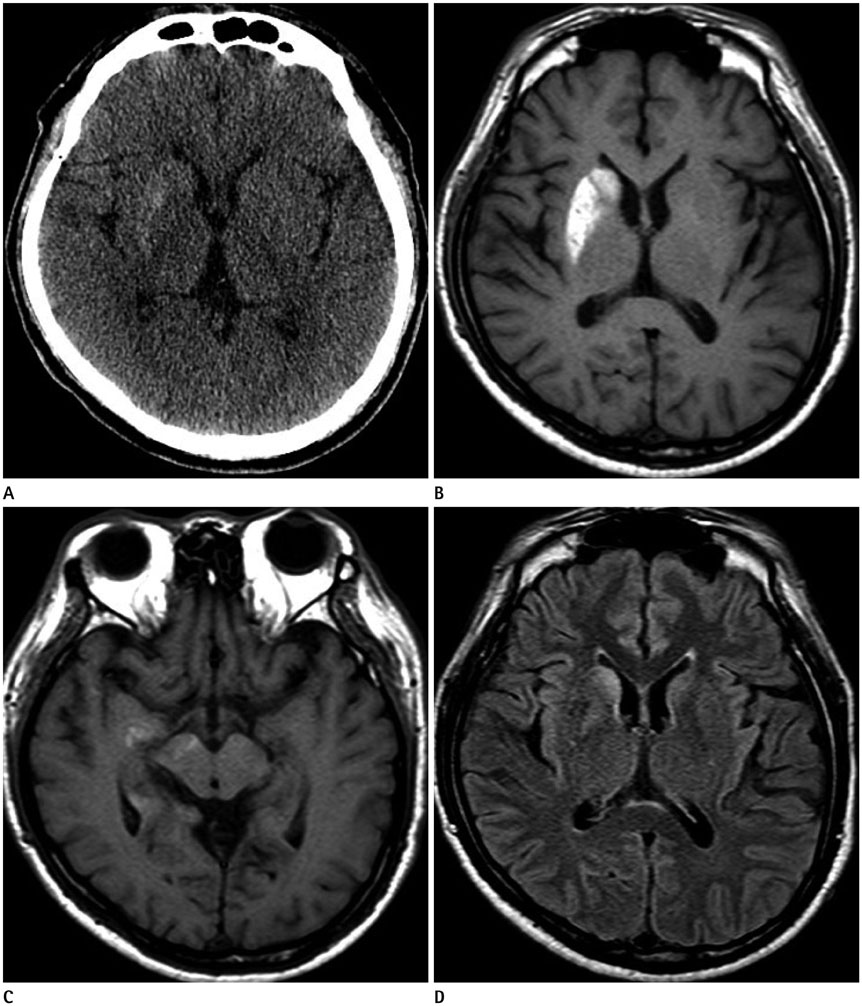
- Hemichorea-hemiballism (HCHB) associated with nonketotic hyperglycemia is the most common cause of unilateral chorea in patients with type 2 diabetes mellitus. T1-weighted MRI characteristically demonstrates hyperintensity in the contralateral corpus striatum. Here we describe a case of HCHB associated with nonketotic hyperglycemia and unusual brain involvement. A 51-year-old man presented with involuntary limb movements for several months. He had a history of diabetes mellitus and poorly controlled hyperglycemia. MRI demonstrated characteristic striatal hyperintensity, with involvement of the temporal lobe and midbrain. The patient's hyperglycemia was controlled with medication. However, his involuntary movements were reduced in terms of severity, but not eliminated, by the time of discharge. HCHB associated with hyperglycemia usually resolves rapidly after correction of blood glucose levels; thus, early recognition and glycemic control are needed to prevent an irreversible outcome.
MeSH Terms
Figure
Reference
-
1. Lee BC, Hwang SH, Chang GY. Hemiballismus-hemichorea in older diabetic women: a clinical syndrome with MRI correlation. Neurology. 1999; 52:646–648.2. Shan DE, Ho DM, Chang C, Pan HC, Teng MM. Hemichorea-hemiballism: an explanation for MR signal changes. AJNR Am J Neuroradiol. 1998; 19:863–870.3. Lai PH, Tien RD, Chang MH, Teng MM, Yang CF, Pan HB, et al. Chorea-ballismus with nonketotic hyperglycemia in primary diabetes mellitus. AJNR Am J Neuroradiol. 1996; 17:1057–1064.4. Chang CV, Felicio AC, Godeiro Cde, Matsubara LS, Duarte DR, Ferraz HB, et al. Chorea-ballism as a manifestation of decompensated type 2 diabetes mellitus. Am J Med Sci. 2007; 333:175–177.5. Oh SH, Lee KY, Im JH, Lee MS. Chorea associated with non-ketotic hyperglycemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI study: a meta-analysis of 53 cases including four present cases. J Neurol Sci. 2002; 200:57–62.6. Chu K, Kang DW, Kim DE, Park SH, Roh JK. Diffusion-weighted and gradient echo magnetic resonance findings of hemichorea-hemiballismus associated with diabetic hyperglycemia: a hyperviscosity syndrome? Arch Neurol. 2002; 59:448–452.7. Nagai C, Kato T, Katagiri T, Sasaki H. Hyperintense putamen on T1-weighted MR images in a case of chorea with hyperglycemia. AJNR Am J Neuroradiol. 1995; 16:1243–1246.8. Bizet J, Cooper CJ, Quansah R, Rodriguez E, Teleb M, Hernandez GT. Chorea, hyperglycemia, basal ganglia syndrome (C-H-BG) in an uncontrolled diabetic patient with normal glucose levels on presentation. Am J Case Rep. 2014; 15:143–146.9. Slabu H, Savedia-Cayabyab S, Senior P, Arnason T. Permanent haemichorea associated with transient hyperglycemia. BMJ Case Rep. 2011; 10. [Epub]. DOI: 10.1136/bcr.08.2011.4641.10. Felicio AC, Chang CV, Godeiro-Junior C, Okoshi MP, Ferraz HB. Hemichorea-hemiballism as the first presentation of type 2 diabetes mellitus. Arq Neuropsiquiatr. 2008; 66:249–250.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Hemichorea Syndrome Associated with Nonketotic Hyperglycemia
- Two Cases of Hemichorea Associated with Nonketotic Hyperglycemia in Type 2 Diabetes Mellitus Patient
- Pediatric Hemichorea-Hemiballismus Associated with Nonketotic Hyperglycemia: A Case Report and Review of the Literature
- Hemiballismus in Uncontrolled Diabetes Mellitus
- Resolution of Stroke-Related Hemichorea-Hemiballismus with Haloperidol