J Korean Med Sci.
2016 Jun;31(6):886-891. 10.3346/jkms.2016.31.6.886.
Being Overweight or Obese Increases the Risk of Progression in Triple-Negative Breast Cancer after Surgical Resection
- Affiliations
-
- 1Department of Radiation Oncology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. rtyoon@gmail.com
- 2Department of Surgery, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 3Department of Pathology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 4Department of Medicine, Yonsei University College of Medicine, Yonsei Graduate School, Seoul, Korea.
- 5Department of Molecular Medicine, College of Medicine, Keimyung University, Daegu, Korea.
- KMID: 2373697
- DOI: http://doi.org/10.3346/jkms.2016.31.6.886
Abstract
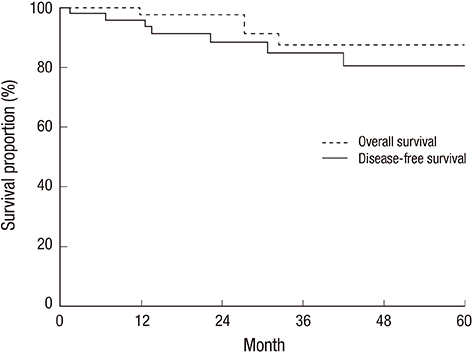
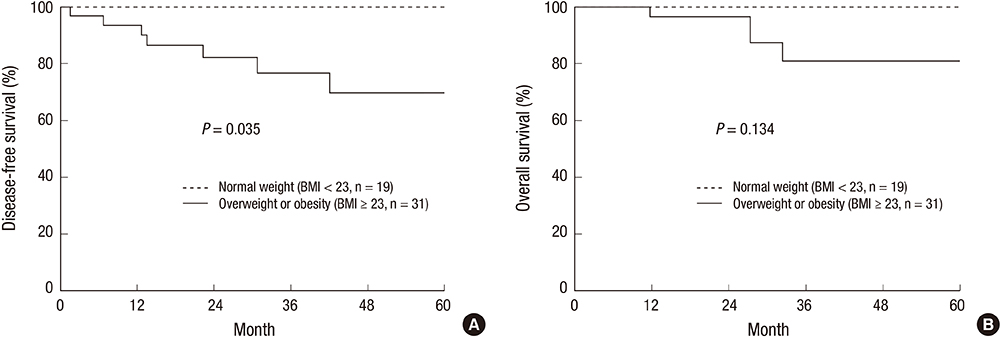
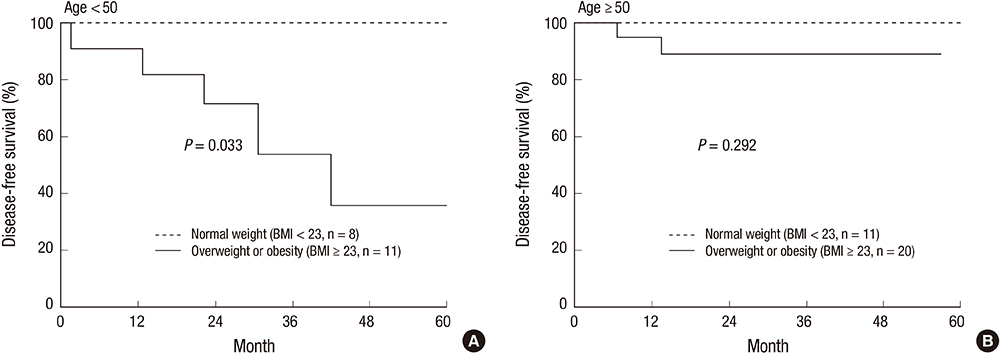
- This study aimed to evaluate the association between body mass index (BMI) and progression in triple-negative breast cancer (TNBC). We retrospectively reviewed the medical records of 50 patients with TNBC who underwent breast-conserving surgery or mastectomy between 2007 and 2014. All patients were classified according to BMI (median 23.5 kg/m2, range 17.2-31.6 kg/m2): 31 patients (62%) were classified as being overweight or obese (BMI ≥ 23 kg/m2) and 19 patients (38%) were classified as having a normal body weight (BMI < 23 kg/m2). The median follow-up for patients was 31.1 months (range, 6.7-101.9 months). Progression occurred in 7 patients (14%), including 5 ipsilateral breast tumor recurrences, 2 regional lymph node metastases, and 5 distant metastases. Progression was significantly correlated with overweight or obese patients (P = 0.035), while none of the normal weight patients showed progression. The 3-year disease-free survival (DFS) and overall survival (OS) rates were 85.0% and 87.7%, respectively. DFS was significantly reduced in overweight or obese patients compared to that in normal weight patients (P = 0.035). However, OS was not significantly compromised by being overweight or obese (P = 0.134). In conclusion, being overweight or obese negatively affects DFS in TNBC patients.
MeSH Terms
-
Adult
Aged
Body Mass Index
Disease Progression
Disease-Free Survival
Female
Follow-Up Studies
Humans
Middle Aged
Neoplasm Recurrence, Local
Obesity/*complications
Overweight/*complications
Prognosis
Retrospective Studies
Risk Factors
Survival Rate
Triple Negative Breast Neoplasms/*complications/mortality/*pathology
Figure
Reference
-
1. Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, Senn HJ, Albain KS, Andre F, Bergh J, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013; 24:2206–2223.2. Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, Lickley LA, Rawlinson E, Sun P, Narod SA. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007; 13:4429–4434.3. Hudis CA, Gianni L. Triple-negative breast cancer: an unmet medical need. Oncologist. 2011; 16:Suppl 1. 1–11.4. Seyfried TN, Flores RE, Poff AM, D’Agostino DP. Cancer as a metabolic disease: implications for novel therapeutics. Carcinogenesis. 2014; 35:515–527.5. Boeing H. Obesity and cancer--the update 2013. Best Pract Res Clin Endocrinol Metab. 2013; 27:219–227.6. Yazici O, Aksoy S, Sendur MA, Babacan T, Ozdemir N, Ozisik Y, Zengin N, Altundag K. The effect of obesity on recurrence pattern in early breast cancer patients. J BUON. 2015; 20:954–962.7. Turkoz FP, Solak M, Petekkaya I, Keskin O, Kertmen N, Sarici F, Arik Z, Babacan T, Ozisik Y, Altundag K. Association between common risk factors and molecular subtypes in breast cancer patients. Breast. 2013; 22:344–350.8. Dean SJ, Rhodes A. Triple negative breast cancer: the role of metabolic pathways. Malays J Pathol. 2014; 36:155–162.9. Hauner D, Hauner H. Metabolic syndrome and breast cancer: is there a link? Breast Care (Basel). 2014; 9:277–281.10. Vona-Davis L, Rose DP, Hazard H, Howard-McNatt M, Adkins F, Partin J, Hobbs G. Triple-negative breast cancer and obesity in a rural Appalachian population. Cancer Epidemiol Biomarkers Prev. 2008; 17:3319–3324.11. Hao S, Liu Y, Yu KD, Chen S, Yang WT, Shao ZM. Overweight as a prognostic factor for triple-negative breast cancers in Chinese women. PLoS One. 2015; 10:e0129741.12. Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013; 31:3997–4013.13. Ahn HJ, Jung SJ, Kim TH, Oh MK, Yoon HK. Differences in clinical outcomes between Luminal A and B type breast cancers according to the St. Gallen Consensus 2013. J Breast Cancer. 2015; 18:149–159.14. Miller LD, Smeds J, George J, Vega VB, Vergara L, Ploner A, Pawitan Y, Hall P, Klaar S, Liu ET, et al. An expression signature for p53 status in human breast cancer predicts mutation status, transcriptional effects, and patient survival. Proc Natl Acad Sci USA. 2005; 102:13550–13555.15. Luporsi E, André F, Spyratos F, Martin PM, Jacquemier J, Penault-Llorca F, Tubiana-Mathieu N, Sigal-Zafrani B, Arnould L, Gompel A, et al. Ki-67: level of evidence and methodological considerations for its role in the clinical management of breast cancer: analytical and critical review. Breast Cancer Res Treat. 2012; 132:895–915.16. Sheridan W, Scott T, Caroline S, Yvonne Z, Vanessa B, David V, Karen G, Stephen C. Breast cancer in young women: have the prognostic implications of breast cancer subtypes changed over time? Breast Cancer Res Treat. 2014; 147:617–629.17. Kim IK, Choi HM, Kim MH. Menopausal knowledge and management in peri-menopausal women. J Korean Soc Menopause. 2012; 18:124–131.18. Expert Consultation WH. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.19. Ballard-Barbash R, Hunsberger S, Alciati MH, Blair SN, Goodwin PJ, McTiernan A, Wing R, Schatzkin A. Physical activity, weight control, and breast cancer risk and survival: clinical trial rationale and design considerations. J Natl Cancer Inst. 2009; 101:630–643.20. Davis AA, Kaklamani VG. Metabolic syndrome and triple-negative breast cancer: a new paradigm. Int J Breast Cancer. 2012; 2012:809291.21. Liu R, Huang Y. Lipid signaling in tumorigenesis. Mol Cell Pharmacol. 2014; 6:1–9.22. Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, Pietenpol JA. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest. 2011; 121:2750–2767.23. Erler JT, Linding R. Network medicine strikes a blow against breast cancer. Cell. 2012; 149:731–733.24. Kim HA, Seong MK, Kim EK, Kang E, Park S, Hur MH, Song BJ, Noh WC; Korea Breast Cancer Society. Evaluation of the survival benefit of different chemotherapy regimens in patients with T1-2N0 triple-negative breast cancer. J Breast Cancer. 2015; 18:271–278.25. Sioshansi S, Huber KE, Wazer DE. The implications of breast cancer molecular phenotype for radiation oncology. Front Oncol. 2011; 1:12.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinicopathologic Characteristics and Prognosis of Early Stage Triple Negative Breast Cancer: Comparison with Non-triple Negative Group
- Fear of Cancer Recurrence and Unmet Needs in Triple Negative Breast Cancer Survivors
- Treatment Outcomes of Weakly Positive Hormone Receptor Breast Cancer and Triple-Negative Breast Cancer
- Overexpression of Cell Cycle Progression Inhibitor Geminin is Associated with Tumor Stem-Like Phenotype of Triple-Negative Breast Cancer
- Comment on “Histomorphological Factors Predicting the Response to Neoadjuvant Chemotherapy in Triple-Negative Breast Cancerâ€