Ann Lab Med.
2016 Nov;36(6):529-535. 10.3343/alm.2016.36.6.529.
Prevalence and Molecular Characteristics of Carbapenemase-Producing Enterobacteriaceae From Five Hospitals in Korea
- Affiliations
-
- 1Department of Laboratory Medicine and Research Institute for Antimicrobial Resistance, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Laboratory Medicine, Hallym University College of Medicine, Chuncheon, Korea. swonkeun@hallym.or.kr
- 3Brain Korea 21 PLUS Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Hallym University College of Medicine, Chuncheon, Korea.
- KMID: 2373590
- DOI: http://doi.org/10.3343/alm.2016.36.6.529
Abstract
- BACKGROUND
The emergence of carbapenemase-producing Enterobacteriaceae (CPE) represents a major clinical problem because these bacteria are resistant to most antibiotics. CPE remain relatively uncommon in Korea. We report the prevalence, clinical characteristics, and molecular epidemiology of CPE isolates collected from five university hospitals in Korea.
METHODS
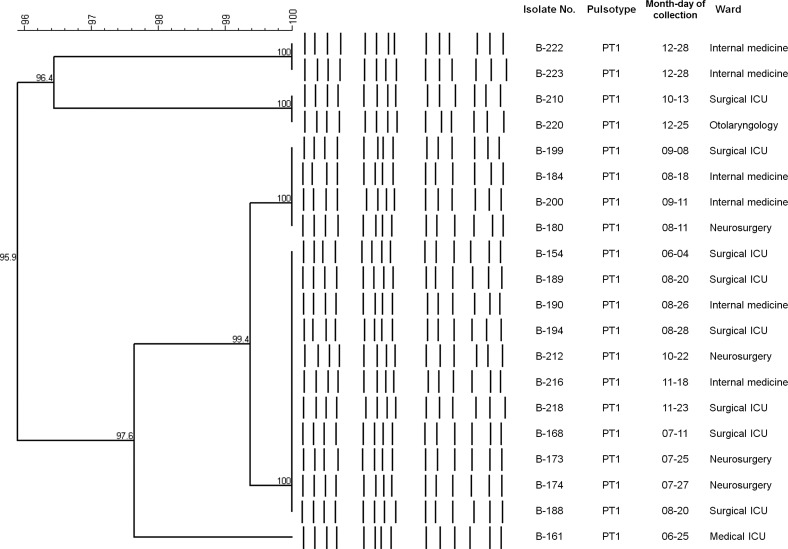
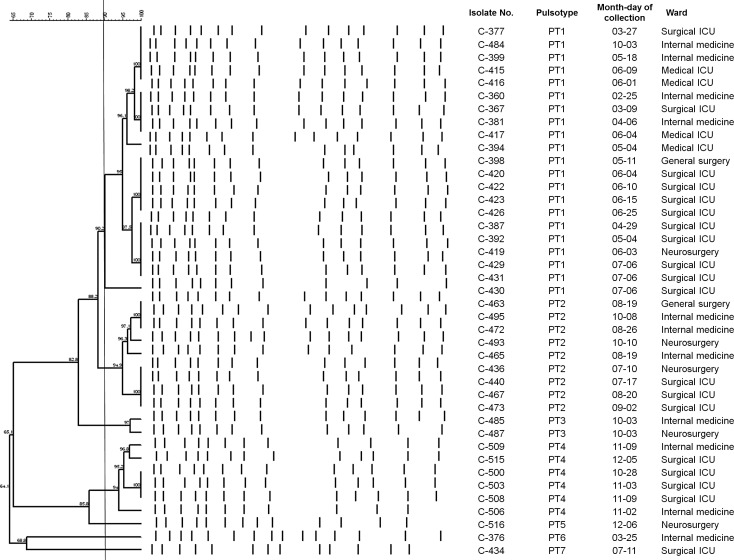
Between January and December 2015, 393 non-duplicated isolates that were nonsusceptible to ertapenem were analyzed. Production of carbapenemase, extended-spectrum β-lactamase, and AmpC β-lactamase was determined by genotypic tests. Antimicrobial susceptibility profiles were determined by using an Etest. Clonality of Klebsiella pneumoniae carbapenemase (KPC)-2-producing and oxacillinase (OXA)-232-producing Klebsiella pneumoniae isolates was determined by pulsed-field gel electrophoresis (PFGE).
RESULTS
Of the 393 isolates tested, 79 (20.1%) were CPE. Of these 79 isolates, 47 (59.5%) harbored the bla(OXA-232) gene while the remaining isolates carried genes bla(KPC-2) (n=27), bla(IMP-1) (n=4), and bla(NDM-1) (n=1). Among the 24 KPC-2 K. pneumoniae isolates from hospital B, 100% were resistant to carbapenems, 8% to colistin, and 0% to tigecycline. Among the 45 OXA-232 K. pneumoniae at hospital C, 95% were resistant to ertapenem, 68% to imipenem, 95% to meropenem, 10% to colistin, and 24% to tigecycline. PFGE analysis revealed a unique pattern for KPC-2 K. pneumoniae and identified 30 isolates belonging to the dominant pulsotypes (PT)1 and PT2 among 41 OXA-232 K. pneumoniae isolates.
CONCLUSIONS
CPE strains are present in Korea, with the majority of K. pneumoniae isolates producing OXA-232 and KPC-2. The prevalence and predominant genotypes of CPE show hospital-specific differences.
Keyword
MeSH Terms
-
Aged
Anti-Bacterial Agents/pharmacology
Bacterial Proteins/*genetics/metabolism
Drug Resistance, Bacterial
Electrophoresis, Gel, Pulsed-Field
Enterobacteriaceae/drug effects/*enzymology/isolation & purification
Enterobacteriaceae Infections/diagnosis/epidemiology/*microbiology
Female
Genotype
Hospitals
Humans
Male
Microbial Sensitivity Tests
Middle Aged
Prevalence
Republic of Korea/epidemiology
beta-Lactamases/*genetics/metabolism
Anti-Bacterial Agents
Bacterial Proteins
beta-Lactamases
Figure
Cited by 3 articles
-
Carbapenem-resistant
Enterobacteriaceae : recent updates and treatment strategies
Hyo-Jin Lee, Dong-Gun Lee
J Korean Med Assoc. 2018;61(4):281-289. doi: 10.5124/jkma.2018.61.4.281.Surveillance Culture of Carbapenemase-Producing
Enterobacteriaceae in a Tertiary-Care Hospital
Eunyoung Lee, Yangsoon Lee
Ann Clin Microbiol. 2018;21(1):8-11. doi: 10.5145/ACM.2018.21.1.8.Management of multi-drug resistant organisms in healthcare settings
Sun Hee Park
J Korean Med Assoc. 2018;61(1):26-35. doi: 10.5124/jkma.2018.61.1.26.
Reference
-
1. Tzouvelekis LS, Markogiannakis A, Psichogiou M, Tassios PT, Daikos GL. Carbapenemases in Klebsiella pneumoniae and other Enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev. 2012; 25:682–707. PMID: 23034326.2. Queenan AM, Bush K. Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev. 2007; 20:440–458. PMID: 17630334.3. Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, et al. Novel carbapenem-hydrolyzing β-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001; 45:1151–1161. PMID: 11257029.4. Nordmann P, Naas T, Poirel L. Global spread of Carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 2011; 17:1791–1798. PMID: 22000347.5. Poirel L, Héritier C, Tolün V, Nordmann P. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004; 48:15–22. PMID: 14693513.6. Poirel L, Potron A, Nordmann P. OXA-48-like carbapenemases: the phantom menace. J Antimicrob Chemother. 2012; 67:1597–1606. PMID: 22499996.7. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. Twenty-fourth Informational supplement, M100-S24. Wayne, PA: Clinical and Laboratory Standards Institute;2014.8. Poirel L, Walsh TR, Cuvillier V, Nordman P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis. 2011; 70:119–123. PMID: 21398074.9. Ryoo NH, Kim EC, Hong SG, Park YJ, Lee K, Bae IK, et al. Dissemination of SHV-12 and CTX-M-type extended-spectrum β-lactamases among clinical isolates of Escherichia coli and Klebsiella pneumoniae and emergence of GES-3 in Korea. J Antimicrob Chemother. 2005; 56:698–702. PMID: 16141280.10. Pérez-Pérez FJ, Hanson ND. Detection of plasmid-mediated AmpC β-lactamase genes in clinical isolates by using multiplex PCR. J Clin Microbiol. 2002; 40:2153–2162. PMID: 12037080.11. Korea Centers for Disease Control and Prevention. Korean Antimicrobial Resistance Monitoring System (KARMS) annual report, 2014. Korea Centers for Disease Control and Prevention;2015.12. Centers for Disease Control and Prevention. Vital signs: carbapenem-resistant Enterobacteriaceae. MMWR Morb Mortal Wkly Rep. 2013; 62:165–170. PMID: 23466435.13. Pollett S, Miller S, Hindler J, Uslan D, Carvalho M, Humphries RM. Phenotypic and molecular characteristics of carbapenem-resistant Enterobacteriaceae in a health care system in Los Angeles, California, from 2011-2013. J Clin Microbiol. 2014; 52:4003–4009. PMID: 25210072.14. Tseng IL, Liu YM, Wang SJ, Yeh HY, Hsieh CL, Lu HL, et al. Emergence of carbapenemase producing Klebsiella pneumoniae and spread of KPC-2 and KPC-17 in Taiwan: a nationwide study from 2011 to 2013. PLoS One. 2015; 10:e0138471. PMID: 26384242.15. Kim MN, Yong D, An D, Chung HS, Woo JH, Lee K, et al. Nosocomial clustering of NDM-1-producing Klebsiella pneumoniae sequence type 340 strains in four patients at a South Korean tertiary care hospital. J Clin Microbiol. 2012; 50:1433–1436. PMID: 22259206.16. Hong SK, Yong D, Kim K, Hong SS, Hong SG, Khosbayar T, et al. First outbreak of KPC-2-producing Klebsiella pneumoniae sequence type 258 in a hospital in South Korea. J Clin Microbiol. 2013; 51:3877–3879. PMID: 24006005.17. Jeong SH, Lee KM, Lee J, Bae IK, Kim JS, Kim HS, et al. Clonal and horizontal spread of the blaOXA-232 gene among Enterobacteriaceae in a Korean hospital. Diagn Microbiol Infect Dis. 2015; 82:70–72. PMID: 25702524.18. Lefebvre B, Lévesque S, Bourgault AM, Mulvey MR, Mataseje L, Boyd D, et al. Carbapenem non-susceptible Enterobacteriaceae in Quebec, Canada: results of a laboratory surveillance program (2010-2012). PLoS One. 2015; 10:e0125076. PMID: 25910041.19. Brañas P, Villa J, Viedma E, Mingorance J, Orellana MA, Chaves F. Molecular epidemiology of carbapenemase-producing Klebsiella pneumoniae in a hospital in Madrid: Successful establishment of an OXA-48 ST11 clone. Int J Antimicrob Agents. 2015; 46:111–116. PMID: 25914088.20. Docquier JD, Calderone V, De Luca F, Benvenuti M, Giuliani F, Bellucci L, et al. Crystal structure of the OXA-48 β-lactamase reveals mechanistic diversity among class D carbapenemases. Chem Biol. 2009; 16:540–547. PMID: 19477418.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of Carbapenem-Resistant Enterobacteriaceae in Seoul, Korea
- Carbapenem-resistant Enterobacteriaceae in Korea
- Surveillance Culture of Carbapenemase-Producing Enterobacteriaceae in a Tertiary-Care Hospital
- Characterization of Carbapenemase Genes in Enterobacteriaceae Species Exhibiting Decreased Susceptibility to Carbapenems in a University Hospital in Chongqing, China
- Rapid Identification of OXA-48-like, KPC, NDM, and VIM Carbapenemase-Producing Enterobacteriaceae From Culture: Evaluation of the RESIST-4 O.K.N.V. Multiplex Lateral Flow Assay