Korean J Ophthalmol.
2017 Apr;31(2):172-174. 10.3341/kjo.2017.31.2.172.
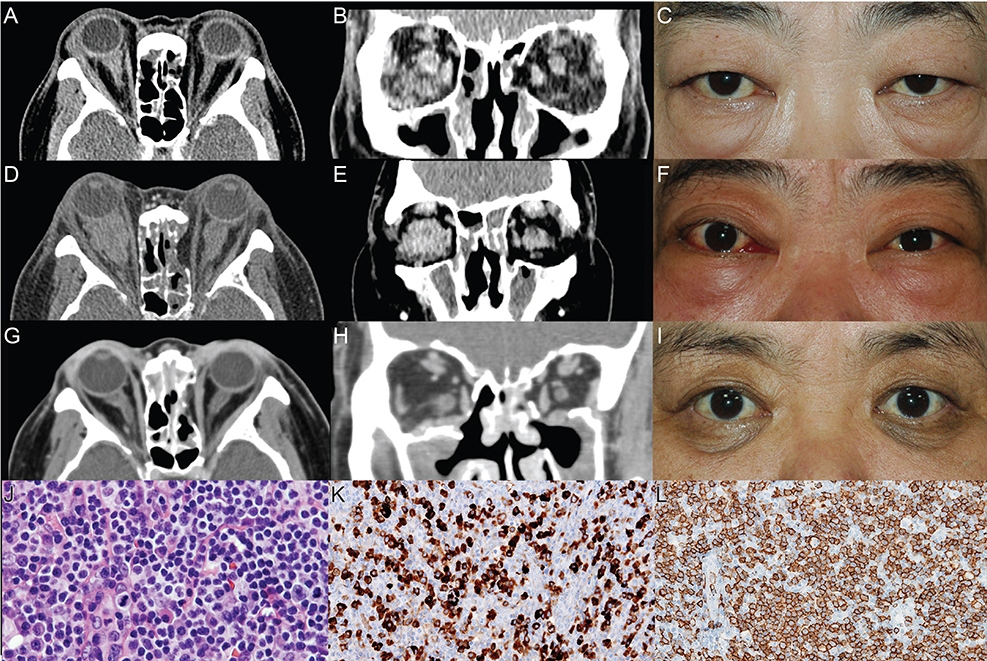
Incipient Ocular Mucosa-associated Lymphoid Tissue Lymphoma in IgG4-related Orbital Disease
- Affiliations
-
- 1Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea.
- 2Kyung Hee University College of Medicine, Seoul, Korea.
- 3Department of Ophthalmology, Kyungpook National University School of Medicine, Daegu, Korea.
- 4Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 5Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. yoonjs@yuhs.ac
- KMID: 2373475
- DOI: http://doi.org/10.3341/kjo.2017.31.2.172
Abstract
- No abstract available.
Figure
Reference
-
1. van den Brand M, van Krieken JH. Recognizing nodal marginal zone lymphoma: recent advances and pitfalls. A systematic review. Haematologica. 2013; 98:1003–1013.2. Lee MJ, Kim N, Choe JY, et al. Clinicopathological analysis of ocular adnexal extranodal marginal zone B-cell lymphoma with IgG4-positive cells. PLoS One. 2015; 10:e0131458.3. Igawa T, Hayashi T, Ishiguro K, et al. IgG4-producing lymphoma arising in a patient with IgG4-related disease. Med Mol Morphol. 2016; 49:243–249.4. Yamamoto M, Takahashi H, Tabeya T, et al. Risk of malignancies in IgG4-related disease. Mod Rheumatol. 2012; 22:414–418.5. Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012; 22:21–30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ocular adnexal mucosa-associated lymphoid tissue lymphoma: a narrative review
- The Prognosis of Ocular-adnexal Lymphoproliferative Lesions
- Mucosa-Associated Lymphoid Tissue Lymphoma of the Esophagus Coexistent with Bronchus-Associated Lymphoid Tissue Lymphoma of the Lung
- A case report of the Pulmonary Malignant Lymphomaof the mucosa-associated lymphoid tissue(MALT)
- Role of Chemotherapy in Gastric Marginal Zone B-Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Type