J Gastric Cancer.
2012 Sep;12(3):149-155.
Risk Stratification for Serosal Invasion Using Preoperative Predictors in Patients with Advanced Gastric Cancer
- Affiliations
-
- 1Department of Surgery, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea. shjin@kcch.re.kr
- 2Department of Surgery, Dongnam Institute of Radiological and Medical Sciences, Busan, Korea.
- 3Department of Pathology, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea.
- 4Department of Surgery, Konkuk University Medical Center, Seoul, Korea.
Abstract
- PURPOSE
Although serosal invasion is a critical predisposing factor for peritoneal dissemination in advanced gastric cancer, the accuracy of preoperative assessment using routine imaging studies is unsatisfactory. This study was conducted to identify high-risk group for serosal invasion using preoperative factors in patients with advanced gastric cancer.
MATERIALS AND METHODS
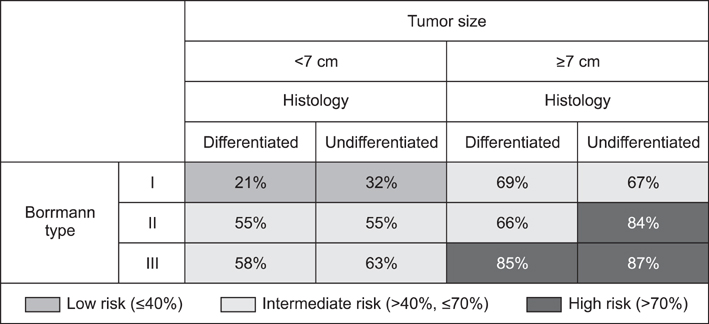
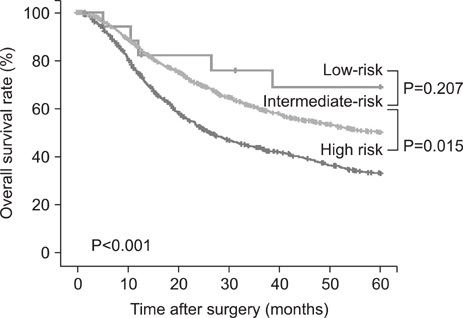
We retrospectively analyzed clinicopathological features of 3,529 advanced gastric cancer patients with Borrmann type I/II/III who underwent gastrectomy at Korea Cancer Center Hospital between 1991 and 2005. We stratified patients into low- (< or =40%), intermediate- (40~70%), and high-risk (>70%) groups, according to the probability of serosal invasion.
RESULTS
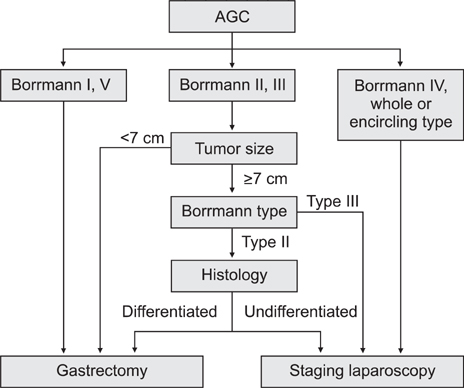
Borrmann type, size, longitudinal and circumferential location, and histology of tumors were independent risk factors for serosal invasion. Most tumors of whole stomach location or encircling type had serosal invasion, so they belonged to high-risk group. Patients were subdivided into 12 subgroups in combination of Borrmann type, size, and histology. A subgroup with Borrmann type II, large size (> or =7 cm), and undifferentiated histology and 2 subgroups with Borrmann type III, large size, and regardless of histology belonged to high-risk group and corresponded to 25% of eligible patients.
CONCLUSIONS
This study have documented high-risk group for serosal invasion using preoperative predictors. And risk stratification for serosal invasion through the combination with imaging studies may collaboratively improve the accuracy of preoperative assessment, reduce the number of eligible patients for further staging laparoscopy, and optimize therapeutic strategy for each individual patient prior to surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Sugarbaker PH, Yu W, Yonemura Y. Gastrectomy, peritonectomy, and perioperative intraperitoneal chemotherapy: the evolution of treatment strategies for advanced gastric cancer. Semin Surg Oncol. 2003. 21:233–248.
Article2. Marutsuka T, Shimada S, Shiomori K, Hayashi N, Yagi Y, Yamane T, et al. Mechanisms of peritoneal metastasis after operation for non-serosa-invasive gastric carcinoma: an ultrarapid detection system for intraperitoneal free cancer cells and a prophylactic strategy for peritoneal metastasis. Clin Cancer Res. 2003. 9:678–685.3. Yonemura Y, Kawamura T, Bandou E, Tsukiyama G, Endou Y, Miura M. The natural history of free cancer cells in the peritoneal cavity. Recent Results Cancer Res. 2007. 169:11–23.
Article4. Kapiev A, Rabin I, Lavy R, Chikman B, Shapira Z, Kais H, et al. The role of diagnostic laparoscopy in the management of patients with gastric cancer. Isr Med Assoc J. 2010. 12:726–728.5. Lehnert T, Rudek B, Kienle P, Buhl K, Herfarth C. Impact of diagnostic laparoscopy on the management of gastric cancer: prospective study of 120 consecutive patients with primary gastric adenocarcinoma. Br J Surg. 2002. 89:471–475.
Article6. Bando E, Yonemura Y, Takeshita Y, Taniguchi K, Yasui T, Yoshimitsu Y, et al. Intraoperative lavage for cytological examination in 1,297 patients with gastric carcinoma. Am J Surg. 1999. 178:256–262.
Article7. Suzuki T, Ochiai T, Hayashi H, Hori S, Shimada H, Isono K. Peritoneal lavage cytology findings as prognostic factor for gastric cancer. Semin Surg Oncol. 1999. 17:103–107.
Article8. Yamamoto M, Matsuyama A, Kameyama T, Okamoto M, Okazaki J, Utsunomiya T, et al. Prognostic re-evaluation of peritoneal lavage cytology in Japanese patients with gastric carcinoma. Hepatogastroenterology. 2009. 56:261–265.9. Sugarbaker PH, Yonemura Y. Clinical pathway for the management of resectable gastric cancer with peritoneal seeding: best palliation with a ray of hope for cure. Oncology. 2000. 58:96–107.
Article10. Boku T, Nakane Y, Minoura T, Takada H, Yamamura M, Hioki K, et al. Prognostic significance of serosal invasion and free intraperitoneal cancer cells in gastric cancer. Br J Surg. 1990. 77:436–439.
Article11. Furukawa K, Miyahara R, Itoh A, Ohmiya N, Hirooka Y, Mori K, et al. Diagnosis of the invasion depth of gastric cancer using MDCT with virtual gastroscopy: comparison with staging with endoscopic ultrasound. AJR Am J Roentgenol. 2011. 197:867–875.
Article12. Mukai K, Ishida Y, Okajima K, Isozaki H, Morimoto T, Nishiyama S. Usefulness of preoperative FDG-PET for detection of gastric cancer. Gastric Cancer. 2006. 9:192–196.
Article13. Yook JH, Oh ST, Kim BS. Clinicopathological analysis of Borrmann type IV gastric cancer. Cancer Res Treat. 2005. 37:87–91.
Article14. Li C, Oh SJ, Kim S, Hyung WJ, Yan M, Zhu ZG, et al. Macroscopic Borrmann type as a simple prognostic indicator in patients with advanced gastric cancer. Oncology. 2009. 77:197–204.
Article15. Maehara Y, Anai H, Moriguchi S, Watanabe A, Tsujitani S, Sugimachi K. Gastric carcinoma invading muscularis propria and macroscopic appearance. Eur J Surg Oncol. 1992. 18:131–134.16. Ichiyoshi Y, Tomoda M, Tomisaki S, Oda S, Ohno S, Maehara Y, et al. Macroscopic appearance and biological character of gastric cancer invading the muscularis propria. Hepatogastroenterology. 1996. 43:553–559.17. Arnold JC, Neubauer HJ, Zöpf T, Schneider A, Benz C, Adamek HE, et al. Improved tumor staging by diagnostic laparoscopy. Z Gastroenterol. 1999. 37:483–488.18. Blackshaw GR, Barry JD, Edwards P, Allison MC, Thomas GV, Lewis WG. Laparoscopy significantly improves the perceived preoperative stage of gastric cancer. Gastric Cancer. 2003. 6:225–229.
Article19. Roviaro GC, Varoli F, Sonnino D, Nucca O, Rabughino G, Scarduelli A. Can routine laparoscopy help to reduce the rate of explorative laparotomies for gastric cancer? Laparoscopy in gastric cancer. Diagn Ther Endosc. 2000. 6:125–131.
Article20. Sotiropoulos GC, Kaiser GM, Lang H, Treckmann J, Brokalaki EI, Pottgen C, et al. Staging laparoscopy in gastric cancer. Eur J Med Res. 2005. 10:88–91.21. Smith A, Finch MD, John TG, Garden OJ, Brown SP. Role of laparoscopic ultrasonography in the management of patients with oesophagogastric cancer. Br J Surg. 1999. 86:1083–1087.
Article22. Yano M, Tsujinaka T, Shiozaki H, Inoue M, Sekimoto M, Doki Y, et al. Appraisal of treatment strategy by staging laparoscopy for locally advanced gastric cancer. World J Surg. 2000. 24:1130–1135.
Article23. Sadeghi B, Arvieux C, Glehen O, Beaujard AC, Rivoire M, Baulieux J, et al. Peritoneal carcinomatosis from non-gynecologic malignancies: results of the EVOCAPE 1 multicentric prospective study. Cancer. 2000. 88:358–363.
Article24. Hwang SW, Lee DH, Lee SH, Park YS, Hwang JH, Kim JW, et al. Preoperative staging of gastric cancer by endoscopic ultrasonography and multidetector-row computed tomography. J Gastroenterol Hepatol. 2010. 25:512–518.
Article25. Polkowski M. Endosonographic staging of upper intestinal malignancy. Best Pract Res Clin Gastroenterol. 2009. 23:649–661.
Article26. Kwee RM, Kwee TC. Imaging in local staging of gastric cancer: a systematic review. J Clin Oncol. 2007. 25:2107–2116.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Macroscopic Serosal Invasion in Advanced Gastric Cancer
- Significance of Carcinoembryonic Antigen Levels in Peritoneal Washings for Gastric Cancer Patients
- Usefulness of Spiral CT for T Staging of Gastric Carcinoma
- Impact of Intraoperative Macroscopic Diagnosis of Serosal Invasion in Pathological Subserosal (pT3) Gastric Cancer
- The Prognostic Significance of the Preoperative Serum CEA, CA19-9 and AFP Levels in Gastric Cancer Patients