J Korean Soc Radiol.
2017 Mar;76(3):179-186. 10.3348/jksr.2017.76.3.179.
Analysis of Factors Affecting Local Tumor Progression of Colorectal Cancer Liver Metastasis after Radiofrequency Ablation
- Affiliations
-
- 1Department of Radiology, Veterans Health Service Medical Center, Seoul, Korea. yunkucho2004@yahoo.co.kr
- 2Department of Surgery, Veterans Health Service Medical Center, Seoul, Korea.
- KMID: 2371683
- DOI: http://doi.org/10.3348/jksr.2017.76.3.179
Abstract
- PURPOSE
The purpose of this study was to evaluate the independent predictive factors for local tumor progression (LTP) of colorectal liver metastasis (CRLM) after radiofrequency ablation (RFA).
MATERIALS AND METHODS
Patients with CRLM were included in the analysis if nodules were up to five in number, each nodule was ≤ 5 cm, and RFA was performed in our center from January 2006 to December 2015. Univariate and multivariate analyses to identify the predictors of LTP were performed by using a Cox proportional hazard model.
RESULTS
Overall, 58 tumors from 38 patients were included in this study. LTP occurred in 14 tumors from 9 patients. The overall 1- and 3-year LTP rates were 23.5% and 29.4%, respectively. Multivariate analysis showed that tumor size > 2 cm and insufficient ablative margin were two independently significant adverse prognostic factors for LTP (p = 0.045 and 0.022, respectively). The 3-year LTP rates for 33 and 25 tumors with and without sufficient ablative margin were 4.5% and 61.2%, respectively. The difference was statistically significant (p < 0.001). The difference in the 3-year LTP rates according to the tumor size was not statistically significant (p = 0.791).
CONCLUSION
Insufficient ablative margin seems to be the most potent predictor of LTP after RFA of CRLM.
MeSH Terms
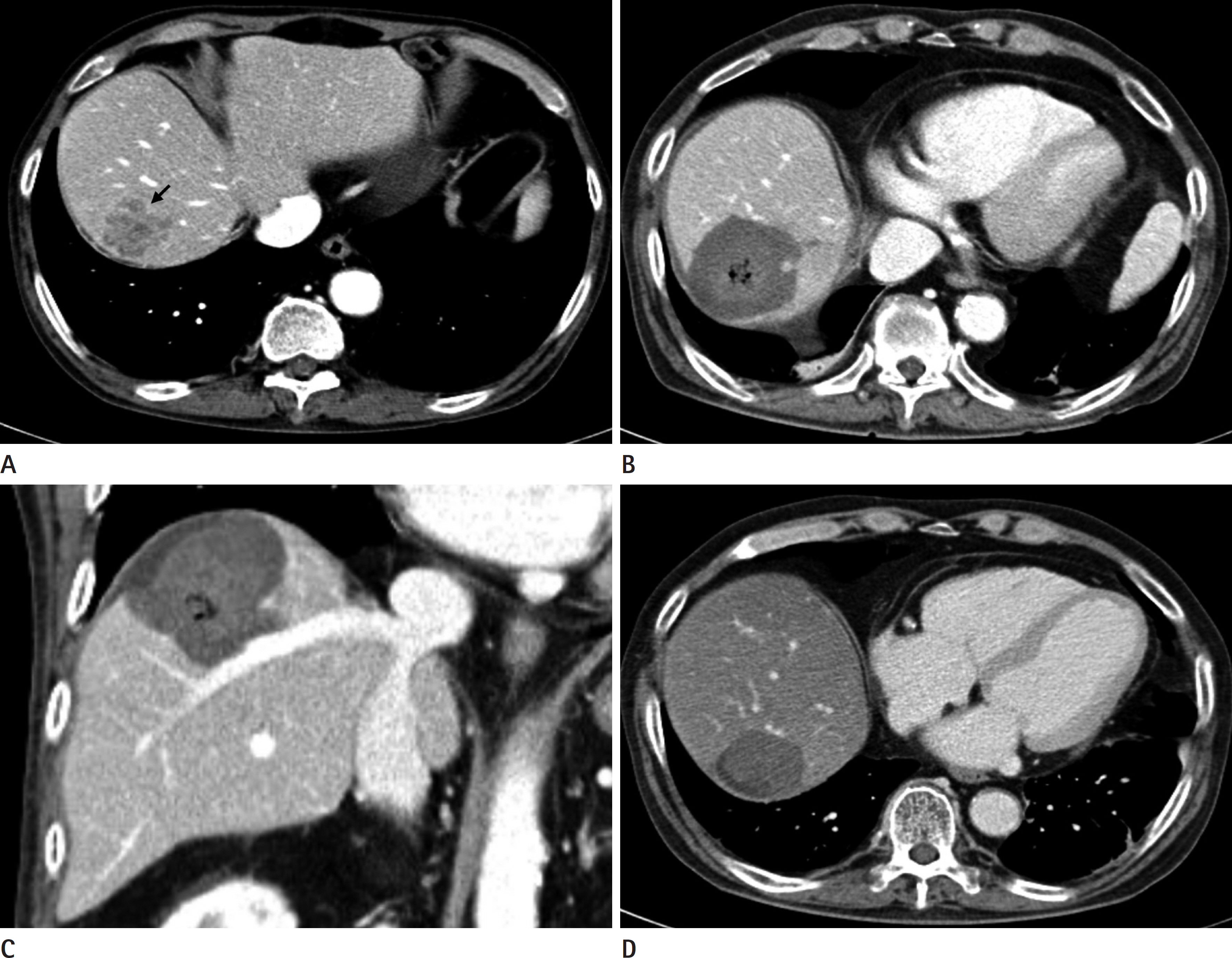
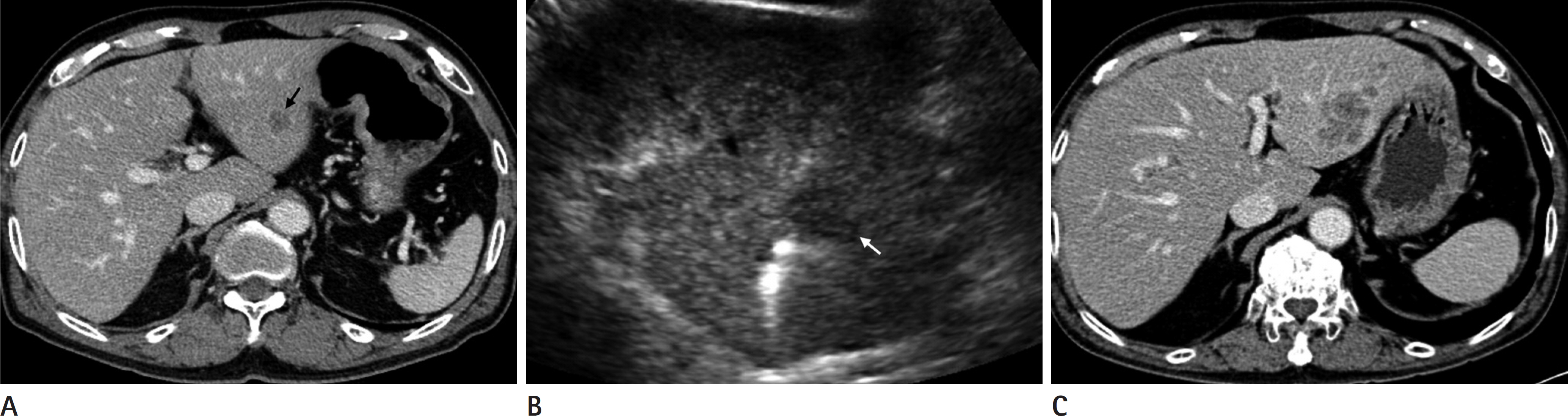
Figure
Reference
-
1. Mulier S, Ruers T, Jamart J, Michel L, Marchal G, Ni Y. Radiofrequency ablation versus resection for resectable colorectal liver metastases: time for a randomized trial? An update. Dig Surg. 2008; 25:445–460.2. Wu YZ, Li B, Wang T, Wang SJ, Zhou YM. Radiofrequency ablation vs hepatic resection for solitary colorectal liver metastasis: a meta-analysis. World J Gastroenterol. 2011; 17:4143–4148.3. Bismuth H, Adam R, Lévi F, Farabos C, Waechter F, Casta-ing D, et al. Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg. 1996; 224:509–520. discussion 520-522.
Article4. Kokudo N, Tada K, Seki M, Ohta H, Azekura K, Ueno M, et al. Anatomical major resection versus nonanatomical lim-ited resection for liver metastases from colorectal carcinoma. Am J Surg. 2001; 181:153–159.
Article5. Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal liver metastases. World J Surg. 1995; 19:59–71.
Article6. Berber E, Tsinberg M, Tellioglu G, Simpfendorfer CH, Siperstein AE. Resection versus laparoscopic radiofrequency thermal ablation of solitary colorectal liver metastasis. J Gastrointest Surg. 2008; 12:1967–1972.
Article7. Hur H, Ko YT, Min BS, Kim KS, Choi JS, Sohn SK, et al. Comparative study of resection and radiofrequency ablation in the treatment of solitary colorectal liver metastases. Am J Surg. 2009; 197:728–736.
Article8. Lee WS, Yun SH, Chun HK, Lee WY, Kim SJ, Choi SH, et al. Clinical outcomes of hepatic resection and radiofrequency ablation in patients with solitary colorectal liver metastasis. J Clin Gastroenterol. 2008; 42:945–949.
Article9. Veltri A, Sacchetto P, Tosetti I, Pagano E, Fava C, Gandini G. Radiofrequency ablation of colorectal liver metastases: small size favorably predicts technique effectiveness and survival. Cardiovasc Intervent Radiol. 2008; 31:948–956.
Article10. Aloia TA, Vauthey JN, Loyer EM, Ribero D, Pawlik TM, Wei SH, et al. Solitary colorectal liver metastasis: resection de-termines outcome. Arch Surg. 2006; 141:460–466. discussion 466-467.11. Livraghi T, Solbiati L, Meloni F, Ierace T, Goldberg SN, Ga-zelle GS. Percutaneous radiofrequency ablation of liver metastases in potential candidates for resection: the “test-of-time approach”. Cancer. 2003; 97:3027–3035.12. Lee KH, Kim HO, Yoo CH, Son BH, Park YL, Cho YK, et al. Comparison of radiofrequency ablation and resection for hepatic metastasis from colorectal cancer. Korean J Gastroenterol. 2012; 59:218–223.
Article13. Abitabile P, Hartl U, Lange J, Maurer CA. Radiofrequency ablation permits an effective treatment for colorectal liver metastasis. Eur J Surg Oncol. 2007; 33:67–71.
Article14. Berber E, Siperstein A. Local recurrence after laparoscopic radiofrequency ablation of liver tumors: an analysis of 1032 tumors. Ann Surg Oncol. 2008; 15:2757–2764.
Article15. Minami Y, Kudo M. Radiofrequency ablation of liver metastases from colorectal cancer: a literature review. Gut Liver. 2013; 7:1–6.
Article16. Machi J, Uchida S, Sumida K, Limm WM, Hundahl SA, Oishi AJ, et al. Ultrasound-guided radiofrequency thermal ablation of liver tumors: percutaneous, laparoscopic, and open surgical approaches. J Gastrointest Surg. 2001; 5:477–489.
Article17. Lang EV, Chen F, Fick LJ, Berbaum KS. Determinants of in-travenous conscious sedation for arteriography. J Vasc Interv Radiol. 1998; 9:407–412.
Article18. Shady W, Petre EN, Gonen M, Erinjeri JP, Brown KT, Covey AM, et al. Percutaneous radiofrequency ablation of colorectal cancer liver metastases: factors affecting outcomes–A 10-year experience at a single center. Radiology. 2016; 278:601–611.
Article19. Funai T, Osugi H, Higashino M, Kinoshita H. Estimation of lymph node metastasis by size in patients with intratho-racic oesophageal cancer. Br J Surg. 2000; 87:1234–1239.
Article20. Alvarez S, Añorbe E, Alcorta P, López F, Alonso I, Cortés J. Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol. 2006; 186:1342–1348.
Article21. Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, et al. Image-guided tumor ablation: stan-dardization of terminology and reporting criteria–a 10-year update. J Vasc Interv Radiol. 2014; 25:1691–1705.e4.
Article22. Tanis E, Nordlinger B, Mauer M, Sorbye H, van Coevorden F, Gruenberger T, et al. Local recurrence rates after radiofrequency ablation or resection of colorectal liver metastases. Analysis of the European Organisation for Research and Treatment of Cancer #40004 and #40983. Eur J Cancer. 2014; 50:912–919.
Article23. Kim YS, Lee WJ, Rhim H, Lim HK, Choi D, Lee JY. The mini-mal ablative margin of radiofrequency ablation of hepatocellular carcinoma (> 2 and < 5 cm) needed to prevent local tumor progression: 3D quantitative assessment using CT image fusion. AJR Am J Roentgenol. 2010; 195:758–765.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiofrequency Ablation of Liver Metastases from Colorectal Cancer: A Literature Review
- Percutaneous radiofrequency ablation for hepatic metastasis of colorectal cancer: assessment of tumor visibility and the feasibility of the procedure with planning ultrasonography
- Radiofrequency Ablation of Hepatic Metastasis from Colorectal Cancer; Early Experience
- Percutaneous radiofrequency ablation of solitary hepatic metastases from colorectal cancer: risk factors of local tumor progression-free survival and overall survival
- Delayed hepatic rupture after radiofrequency ablation for colorectal hepatic metastasis: management with transcatheter arterial embolization