Korean J Crit Care Med.
2017 Feb;32(1):22-28. 10.4266/kjccm.2016.00983.
Blood Transfusion Strategies in Patients Undergoing Extracorporeal Membrane Oxygenation
- Affiliations
-
- 1Department of Cardiothoracic Surgery, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 2Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea. f2000tj@naver.com
- KMID: 2371150
- DOI: http://doi.org/10.4266/kjccm.2016.00983
Abstract
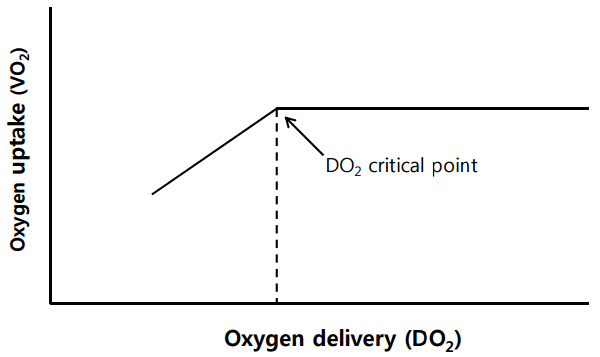
- Extracorporeal membrane oxygenation (ECMO) is frequently associated with bleeding and coagulopathy complications, which may lead to the need for transfusion of multiple blood products. However, blood transfusions are known to increase morbidity and mortality, as well as hospital cost, in critically ill patients. In current practice, patients on ECMO receive a transfusion, on average, of 1-5 packed red blood cells (RBCs)/day, with platelet transfusion accounting for the largest portion of transfusion volume. Generally, adult patients require more transfusions than neonates or children, and patients receiving venovenous ECMO for respiratory failure tend to need smaller transfusion volumes compared to those receiving venoarterial ECMO for cardiac failure. Observation studies have reported that a higher transfusion volume was associated with increased mortality. To date, the evidence for transfusion in patients undergoing ECMO is limited; most knowledge on transfusion strategies was extrapolated from studies in critically ill patients. However, current data support a restrictive blood transfusion strategy for ECMO patients, and a low transfusion trigger seems to be safe and reasonable.
MeSH Terms
Figure
Reference
-
References
1. Extracorporeal Life Support Organization (ELSO). ELSO guidelines [Internet]. Ann Arbor: ELSO;c2016. [cited 2016 Oct 30]. Available from: https://www.elso.org/Resources/Guidelines.aspx.2. Holst LB. Benefits and harms of red blood cell transfusions in patients with septic shock in the intensive care unit. Dan Med J. 2016; 63:B5209.3. Gilliss BM, Looney MR, Gropper MA. Reducing noninfectious risks of blood transfusion. Anesthesiology. 2011; 115:635–49.
Article4. Hébert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999; 340:409–17.5. Holst LB, Haase N, Wetterslev J, Wernerman J, Guttormsen AB, Karlsson S, et al. Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med. 2014; 371:1381–91.
Article6. Roberson RS, Bennett-Guerrero E. Impact of red blood cell transfusion on global and regional measures of oxygenation. Mt Sinai J Med. 2012; 79:66–74.
Article7. Kiefel V. Reactions induced by platelet transfusions. Transfus Med Hemother. 2008; 35:354–8.
Article8. Lelubre C, Vincent J. Red blood cell transfusion in the critically ill patient. Ann Intensive Care. 2011; 1:43.
Article9. Tinmouth A, Fergusson D, Yee IC, Hébert PC; ABLE Investigators; Canadian Critical Care Trials Group. Clinical consequences of red cell storage in the critically ill. Transfusion. 2006; 46:2014–27.
Article10. Koch CG, Li L, Sessler DI, Figueroa P, Hoeltge GA, Mihaljevic T, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med. 2008; 358:1229–39.
Article11. Schmidt M, Tachon G, Devilliers C, Muller G, Hekimian G, Bréchot N, et al. Blood oxygenation and decarboxylation determinants during venovenous ECMO for respiratory failure in adults. Intensive Care Med. 2013; 39:838–46.
Article12. Marik PE, Flemmer M, Shander A. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med. 2015; 373:190–1.
Article13. Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG; FOCUS Investigators, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011; 365:2453–62.
Article14. Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, et al. TITRe2 Investigators: Liberal or restrictive transfusion after cardiac surgery. N Engl J Med. 2015; 372:997–1008.15. Holst LB, Petersen MW, Haase N, Perner A, Wetterslev J. Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. BMJ. 2015; 350:h1354.
Article16. Joshi V, Harvey C, Nakas A, Waller DA, Peek GJ, Firmin R. The need for thoracic surgery in adult patients receiving extracorporeal membrane oxygenation: a 16-year experience. Perfusion. 2013; 28:328–32.
Article17. Tolksdorf B, Schmeck J, Osika A, Bender HJ, Quintel M. Autotransfusion during extracorporeal membrane oxygenation. Int J Artif Organs. 2000; 23:840–4.
Article18. Arnold P, Jackson S, Wallis J, Smith J, Bolton D, Haynes S. Coagulation factor activity during neonatal extra-corporeal membrane oxygenation. Intensive Care Med. 2001; 27:1395–400.
Article19. Butch SH, Knafl P, Oberman HA, Bartlett RH. Blood utilization in adult patients undergoing extracorporeal membrane oxygenated therapy. Transfusion. 1996; 36:61–3.
Article20. McCoy-Pardington D, Judd WJ, Knafl P, Abruzzo LV, Coombes KR, Butch SH, et al. Blood use during extracorporeal membrane oxygenation. Transfusion. 1990; 30:307–9.
Article21. Morris AH, Wallace CJ, Menlove RL, Clemmer TP, Orme JF Jr, Weaver LK, et al. Randomized clinical trial of pressure-controlled inverse ratio ventilation and extracorporeal CO2 removal for adult respiratory distress syndrome. Am J Respir Crit Care Med. 1994; 149(2 Pt 1):295–305.
Article22. Peek GJ, Moore HM, Moore N, Sosnowski AW, Firmin RK. Extracorporeal membrane oxygenation for adult respiratory failure. Chest. 1997; 112:759–64.
Article23. Ang AL, Teo D, Lim CH, Leou KK, Tien SL, Koh MB. Blood transfusion requirements and independent predictors of increased transfusion requirements among adult patients on extracorporeal membrane oxygenation -- a single centre experience. Vox Sang. 2009; 96:34–43.
Article24. Chevuru SC, Sola MC, Theriaque DW, Hutson AD, Leung WC, Perez JA, et al. Florida Collaborative Neonatology Research Group: multicenter analysis of platelet transfusion usage among neonates on extracorporeal membrane oxygenation. Pediatrics. 2002; 109:e89.25. Henríquez-Henríquez M, Kattan J, Chang M, Pizarro I, Faunes M, Martinez C, et al. Blood component usage during extracorporeal membrane oxygenation: experience in 98 patients at a Latin-American tertiary hospital. Int J Artif Organs. 2014; 37:233–40.
Article26. Omar HR, Mirsaeidi M, Socias S, Sprenker C, Caldeira C, Camporesi EM, et al. Plasma free hemoglobin is an independent predictor of mortality among patients on extracorporeal membrane oxygenation support. PLoS One. 2015; 10:e0124034.
Article27. Australia, New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators, Davies A, Jones D, Bailey M, Beca J, Bellomo R, et al. Extracorporeal membrane oxygenation for 2009 influenza A(H1N1) acute respiratory distress syndrome. JAMA. 2009; 302:1888–95.
Article28. Patroniti N, Zangrillo A, Pappalardo F, Peris A, Cianchi G, Braschi A, et al. preparation for severe respiratory emergency outbreaks. Intensive Care Med. 2011; 37:1447–57.
Article29. Smith A, Hardison D, Bridges B, Pietsch J. Red blood cell transfusion volume and mortality among patients receiving extracorporeal membrane oxygenation. Perfusion. 2013; 28:54–60.
Article30. Agerstrand CL, Burkart KM, Abrams DC, Bacchetta MD, Brodie D. Blood conservation in extracorporeal membrane oxygenation for acute respiratory distress syndrome. Ann Thorac Surg. 2015; 99:590–5.
Article31. Voelker MT, Busch T, Bercker S, Fichtner F, Kaisers UX, Laudi S. Restrictive transfusion practice during extracorporeal membrane oxygenation therapy for severe acute respiratory distress syndrome. Artif Organs. 2015; 39:374–8.
Article32. National Heart Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006; 354:2564–75.
Article33. Brodie D, Bacchetta M. Extracorporeal membrane oxygenation for ARDS in adults. N Engl J Med. 2011; 365:1905–14.
Article34. Rosenberg EM, Chambers LA, Gunter JM, Good JA. A program to limit donor exposures to neonates undergoing extracorporeal membrane oxygenation. Pediatrics. 1994; 94:341–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blood Transfusion Strategies in Patients Supported by Extracorporeal Membrane Oxygenation
- Transfusion Associated Hyperkalemia and Cardiac Arrest in an Infant after Extracorporeal Membrane Oxygenation
- Successful Retrieval of a Fractured Guidewire during Extracorporeal Membrane Oxygenator Insertion
- Application of Extracorporeal Membranous Oxygenation in Trauma Patient with Possible Transfusion Related Acute Lung Injury (TRALI)
- Catastrophic catecholamine-induced cardiomyopathy rescued by extracorporeal membrane oxygenation in recurrent malignant pheochromocytoma