J Korean Med Assoc.
2017 Feb;60(2):118-125. 10.5124/jkma.2017.60.2.118.
Recent updates on treatment for pediatric migraine
- Affiliations
-
- 1Department of Pediatrics, Kangnam Sacred Heart Hospital, Hallym University School of Medicine, Seoul, Korea. headaches77@gmail.com
- KMID: 2368921
- DOI: http://doi.org/10.5124/jkma.2017.60.2.118
Abstract
- Pediatric migraine is a disorder that significantly interferes with the everyday life and school life of approximately 8% of children and adolescents in Korea. Recently, studies on migraine have been carried out very rapidly, many drugs have been developed, and acute-phase and preventive treatments for migraine have been evaluated. Therefore, it is necessary to understand the diagnostic criteria and degree of impairment in pediatric migraine and to become familiar with up-to-date treatment methods in children. Research into the use of botulinum toxin or calcitonin gene-related peptide antagonists to treat adult migraine headaches is progressing, and we expect these therapies to be applicable to pediatric patients soon. Many students in our country are suffering from migraines in their daily life. Therefore, we need to acquire the relevant knowledge and identify practical treatment methods for pediatric migraine in children and adolescents in order to reduce their pain.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Recent advances in pediatric headaches
Eun Sook Suh
J Korean Med Assoc. 2017;60(2):109-111. doi: 10.5124/jkma.2017.60.2.109.Pediatric headache: a narrative review
Saeyoon Kim
J Yeungnam Med Sci. 2022;39(4):278-284. doi: 10.12701/jyms.2022.00528.
Reference
-
1. Rho YI, Chung HJ, Lee KH, Eun BL, Eun SH, Nam SO, Kim WS, Kim YO, Park HJ, Kim HS. Prevalence and clinical characteristics of primary headaches among school children in South Korea: a nationwide survey. Headache. 2012; 52:592–599.
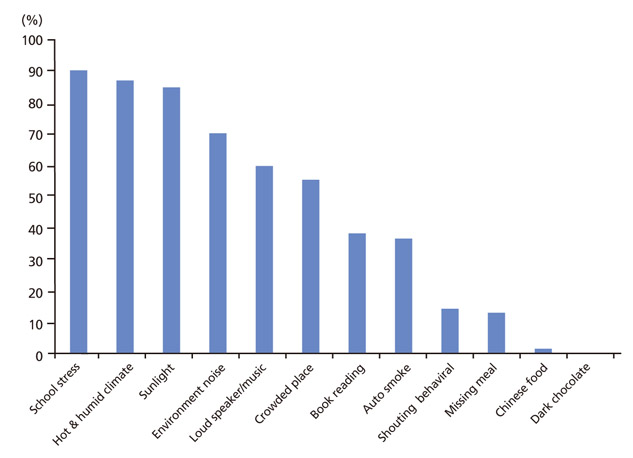
Article2. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013; 33:629–808.3. Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007; 27:394–402.
Article4. Chakravarty A, Mukherjee A, Roy D. Trigger factors in childhood migraine: a clinic-based study from eastern India. J Headache Pain. 2009; 10:375–380.
Article5. Neut D, Fily A, Cuvellier JC, Vallée L. The prevalence of triggers in paediatric migraine: a questionnaire study in 102 children and adolescents. J Headache Pain. 2012; 13:61–65.
Article6. Millichap JG, Yee MM. The diet factor in pediatric and adolescent migraine. Pediatr Neurol. 2003; 28:9–15.
Article7. Chung BY, Hong YL. Comparisons of Stressor and coping style between headache-suffering children and headache-free children. Korean J Child Health Nurs. 2000; 6:354–361.8. Yoon JM, Lee HR, Lee KH. Characteristics of sleep disorders in childhood and adolescence. J Korean Child Neurol Soc. 2007; 15:185–191.9. Rocha-Filho PA, Santos PV. Headaches, quality of life, and academic performance in schoolchildren and adolescents. Headache. 2014; 54:1194–1202.
Article10. Hong EY, Choi KY, Kim SK, Jung AY, Lee KH. Clinical characteristics and diagnoses for pediatric headache in the emergency department. Korean J Headache. 2013; 14:1–5.11. Alfonzo M, Chen L. Acute migraine management in children. Pediatr Emerg Care. 2015; 31:722–727.
Article12. Nye BL, Ward TN. Clinic and emergency room evaluation and testing of headache. Headache. 2015; 55:1301–1308.
Article13. Richer L, Craig W, Rowe B. Randomized controlled trial of treatment expectation and intravenous fluid in pediatric migraine. Headache. 2014; 54:1496–1505.
Article14. Richer L, Billinghurst L, Linsdell MA, Russell K, Vandermeer B, Crumley ET, Durec T, Klassen TP, Hartling L. Drugs for the acute treatment of migraine in children and adolescents. Cochrane Database Syst Rev. 2016; 4:CD005220.
Article15. Patniyot IR, Gelfand AA. Acute treatment therapies for pediatric migraine: a qualitative systematic review. Headache. 2016; 56:49–70.
Article16. Brousseau DC, Duffy SJ, Anderson AC, Linakis JG. Treatment of pediatric migraine headaches: a randomized, double-blind trial of prochlorperazine versus ketorolac. Ann Emerg Med. 2004; 43:256–262.17. Gelfand AA, Goadsby PJ. Treatment of pediatric migraine in the emergency room. Pediatr Neurol. 2012; 47:233–241.
Article18. Kabbouche M. Pediatric inpatient headache therapy: what is available. Headache. 2015; 55:1426–1429.
Article19. Sheridan DC, Meckler GD. Inpatient pediatric migraine treatment: does choice of abortive therapy affect length of stay. J Pediatr. 2016; 179:211–215.
Article20. Tajti J, Szok D, Csati A, Vecsei L. Prophylactic drug treatment of migraine in children and adolescents: an update. Curr Pain Headache Rep. 2016; 20:1.
Article21. Kacperski J, Hershey AD. Preventive drugs in childhood and adolescent migraine. Curr Pain Headache Rep. 2014; 18:422.
Article22. Hickman C, Lewis KS, Little R, Rastogi RG, Yonker M. Prevention for pediatric and adolescent migraine. Headache. 2015; 55:1371–1381.
Article23. Hershey AD, Powers SW, Bentti AL, Degrauw TJ. Effectiveness of amitriptyline in the prophylactic management of childhood headaches. Headache. 2000; 40:539–549.
Article24. Lewis DW, Diamond S, Scott D, Jones V. Prophylactic treatment of pediatric migraine. Headache. 2004; 44:230–237.
Article25. Kim H, Byun SH, Kim JS, Lim BC, Chae JH, Choi J, Kim KJ, Hwang YS, Hwang H. Comparison of flunarizine and topiramate for the prophylaxis of pediatric migraines. Eur J Paediatr Neurol. 2013; 17:45–49.
Article26. Abbaskhanian A, Sadeghi HR, Erfani A, Rezai MS. Effective dose of topiramate in pediatric migraine prophylaxis. J Pediatr Neurosci. 2012; 7:171–174.
Article27. Dodick DW, Turkel CC, DeGryse RE, Aurora SK, Silberstein SD, Lipton RB, Diener HC, Brin MF. PREEMPT Chronic Migraine Study Group. OnabotulinumtoxinA for treatment of chronic migraine: pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache. 2010; 50:921–936.
Article