J Periodontal Implant Sci.
2017 Feb;47(1):20-29. 10.5051/jpis.2017.47.1.20.
Three-dimensional microstructure of human alveolar trabecular bone: a micro-computed tomography study
- Affiliations
-
- 1Department of Periodontology, Chonbuk National University School of Dentistry, Jeonju, Korea. grayheron@hanmail.net
- 2Division in Anatomy and Developmental Biology, Department of Oral Biology, BK21 PLUS Project, Human Identification Research Center, Yonsei University College of Dentistry, Seoul, Korea.
- 3Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2368884
- DOI: http://doi.org/10.5051/jpis.2017.47.1.20
Abstract
- PURPOSE
The microstructural characteristics of trabecular bone were identified using micro-computed tomography (micro-CT), in order to develop a potential strategy for implant surface improvement to facilitate osseointegration.
METHODS
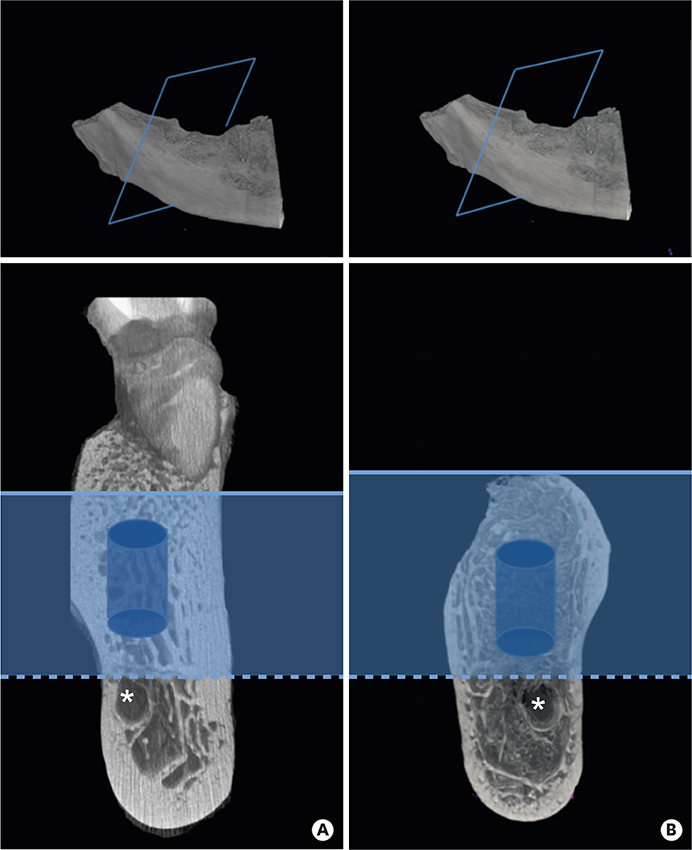
Alveolar bone specimens from the cadavers of 30 humans were scanned by high-resolution micro-CT and reconstructed. Volumes of interest chosen within the jaw were classified according to Hounsfield units into 4 bone quality categories. Several structural parameters were measured and statistically analyzed.
RESULTS
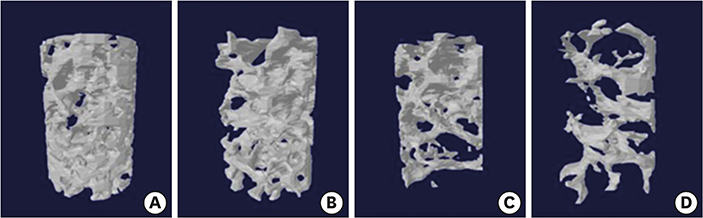
Alveolar bone specimens with D1 bone quality had significantly higher values for all structural parameters than the other bone quality categories, except for trabecular thickness (Tb.Th). The percentage of bone volume, trabecular separation (Tb.Sp), and trabecular number (Tb.N) varied significantly among bone quality categories. Tb.Sp varied markedly across the bone quality categories (D1: 0.59±0.22 mm, D4: 1.20±0.48 mm), whereas Tb.Th had similar values (D1: 0.30±0.08 mm, D4: 0.22±0.05 mm).
CONCLUSIONS
Bone quality depended on Tb.Sp and number"”that is, endosteal space architecture"”rather than bone surface and Tb.Th. Regardless of bone quality, Tb.Th showed little variation. These factors should be taken into account when developing individualized implant surface topographies.
Keyword
Figure
Reference
-
1. Jemt T, Lekholm U. Oral implant treatment in posterior partially edentulous jaws: a 5-year follow-up report. Int J Oral Maxillofac Implants. 1993; 8:635–640.2. Drago CJ. Rates of osseointegration of dental implants with regard to anatomical location. J Prosthodont. 1992; 1:29–31.
Article3. Fanuscu MI, Chang TL. Three-dimensional morphometric analysis of human cadaver bone: microstructural data from maxilla and mandible. Clin Oral Implants Res. 2004; 15:213–218.
Article4. Brånemark PI, Zarb GA, Albrektsson T. Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago (IL): Quintessence;1985.5. Jensen O. Site classification for the osseointegrated implant. J Prosthet Dent. 1989; 61:228–234.
Article6. Misch CE. Contemporary implant dentistry. St. Louis (MO): Mosby;1993.7. Kim YJ, Henkin J. Micro-computed tomography assessment of human alveolar bone: bone density and three-dimensional micro-architecture. Clin Implant Dent Relat Res. 2015; 17:307–313.
Article8. Park YS, Kim S, Oh SH, Park HJ, Lee S, Kim TI, et al. Comparison of alveolar ridge preservation methods using three-dimensional micro-computed tomographic analysis and two-dimensional histometric evaluation. Imaging Sci Dent. 2014; 44:143–148.
Article9. Burghardt AJ, Link TM, Majumdar S. High-resolution computed tomography for clinical imaging of bone microarchitecture. Clin Orthop Relat Res. 2011; 469:2179–2193.
Article10. Ibrahim N, Parsa A, Hassan B, van der Stelt P, Wismeijer D. Diagnostic imaging of trabecular bone microstructure for oral implants: a literature review. Dentomaxillofac Radiol. 2013; 42:20120075.
Article11. Ulrich D, van Rietbergen B, Laib A, Rüegsegger P. The ability of three-dimensional structural indices to reflect mechanical aspects of trabecular bone. Bone. 1999; 25:55–60.
Article12. Moon HS, Won YY, Kim KD, Ruprecht A, Kim HJ, Kook HK, et al. The three-dimensional microstructure of the trabecular bone in the mandible. Surg Radiol Anat. 2004; 26:466–473.
Article13. Sugisaki M, Agematsu H, Matsunaga S, Saka H, Sakiyama K, Ide Y. Three-dimensional analysis of the internal structure of the mandibular condyle in dentulous and edentulous jaws using micro-CT. Cranio. 2009; 27:78–87.
Article14. Xue W, Krishna BV, Bandyopadhyay A, Bose S. Processing and biocompatibility evaluation of laser processed porous titanium. Acta Biomater. 2007; 3:1007–1018.
Article15. LeBrun A, Joglekar T, Bieberich C, Ma R, Zhu L. Identification of infusion strategy for achieving repeatable nanoparticle distribution and quantification of thermal dosage using micro-CT Hounsfield unit in magnetic nanoparticle hyperthermia. Int J Hyperthermia. 2016; 32:132–143.
Article16. Todisco M, Trisi P. Bone mineral density and bone histomorphometry are statistically related. Int J Oral Maxillofac Implants. 2005; 20:898–904.17. Razali NM, Wah YB. Power comparisons of shapiro-wilk, kolmogorov-smirnov, lilliefors and anderson-darling tests. J Stat Model Anal. 2011; 2:21–33.18. Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika. 1965; 52:591–611.
Article19. Puleo DA, Nanci A. Understanding and controlling the bone-implant interface. Biomaterials. 1999; 20:2311–2321.
Article20. Kim JE, Shin JM, Oh SO, Yi WJ, Heo MS, Lee SS, et al. The three-dimensional microstructure of trabecular bone: analysis of site-specific variation in the human jaw bone. Imaging Sci Dent. 2013; 43:227–233.
Article21. Norton MR, Gamble C. Bone classification: an objective scale of bone density using the computerized tomography scan. Clin Oral Implants Res. 2001; 12:79–84.
Article22. Borden M, Attawia M, Khan Y, Laurencin CT. Tissue engineered microsphere-based matrices for bone repair: design and evaluation. Biomaterials. 2002; 23:551–559.
Article23. Le Guéhennec L, Soueidan A, Layrolle P, Amouriq Y. Surface treatments of titanium dental implants for rapid osseointegration. Dent Mater. 2007; 23:844–854.
Article24. Jiang Y, Zhao J, Augat P, Ouyang X, Lu Y, Majumdar S, et al. Trabecular bone mineral and calculated structure of human bone specimens scanned by peripheral quantitative computed tomography: relation to biomechanical properties. J Bone Miner Res. 1998; 13:1783–1790.
Article25. Pallesen L, Schou S, Aaboe M, Hjørting-Hansen E, Nattestad A, Melsen F. Influence of particle size of autogenous bone grafts on the early stages of bone regeneration: a histologic and stereologic study in rabbit calvarium. Int J Oral Maxillofac Implants. 2002; 17:498–506.26. Taniguchi N, Fujibayashi S, Takemoto M, Sasaki K, Otsuki B, Nakamura T, et al. Effect of pore size on bone ingrowth into porous titanium implants fabricated by additive manufacturing: an in vivo experiment. Mater Sci Eng C. 2016; 59:690–701.
Article27. Zadpoor AA. Bone tissue regeneration: the role of scaffold geometry. Biomater Sci. 2015; 3:231–245.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in Microstructure of Proximal Femoral Trabecular Bone
- The three-dimensional microstructure of trabecular bone: Analysis of site-specific variation in the human jaw bone
- Micro-Structural Profiles of Trabecular Bone at the Ankle Joint
- Effect of different voxel sizes on the accuracy of CBCT measurements of trabecular bone microstructure: A comparative micro-CT study
- Micro-CT analysis of LPS-induced Alveolar Bone Loss in Diabetic Mice