Investig Clin Urol.
2017 Mar;58(2):117-126. 10.4111/icu.2017.58.2.117.
Immunohistochemical analysis of estrogen receptors in prostate and clinical correlation in men with benign prostatic hyperplasia
- Affiliations
-
- 1Department of Urology and Renal Transplantation, SMS Medical College & Attached Hospitals, Jaipur, India. bhattarrohit@gmail.com
- 2Department of Pathology, SMS Medical College & Attached Hospitals, Jaipur, India.
- KMID: 2368477
- DOI: http://doi.org/10.4111/icu.2017.58.2.117
Abstract
- PURPOSE
Estrogens act through interaction with 2 receptor subtypes, ER alpha (ERα) and ER beta (ERβ), in human prostate. The aim of the present study was to semiquantitatively assess the differential expression of ER subtypes in human benign prostatic hyperplasia (BPH) by use of immunocytochemistry (IHC) methods and to explore their relationship with various measures of BPH.
MATERIALS AND METHODS
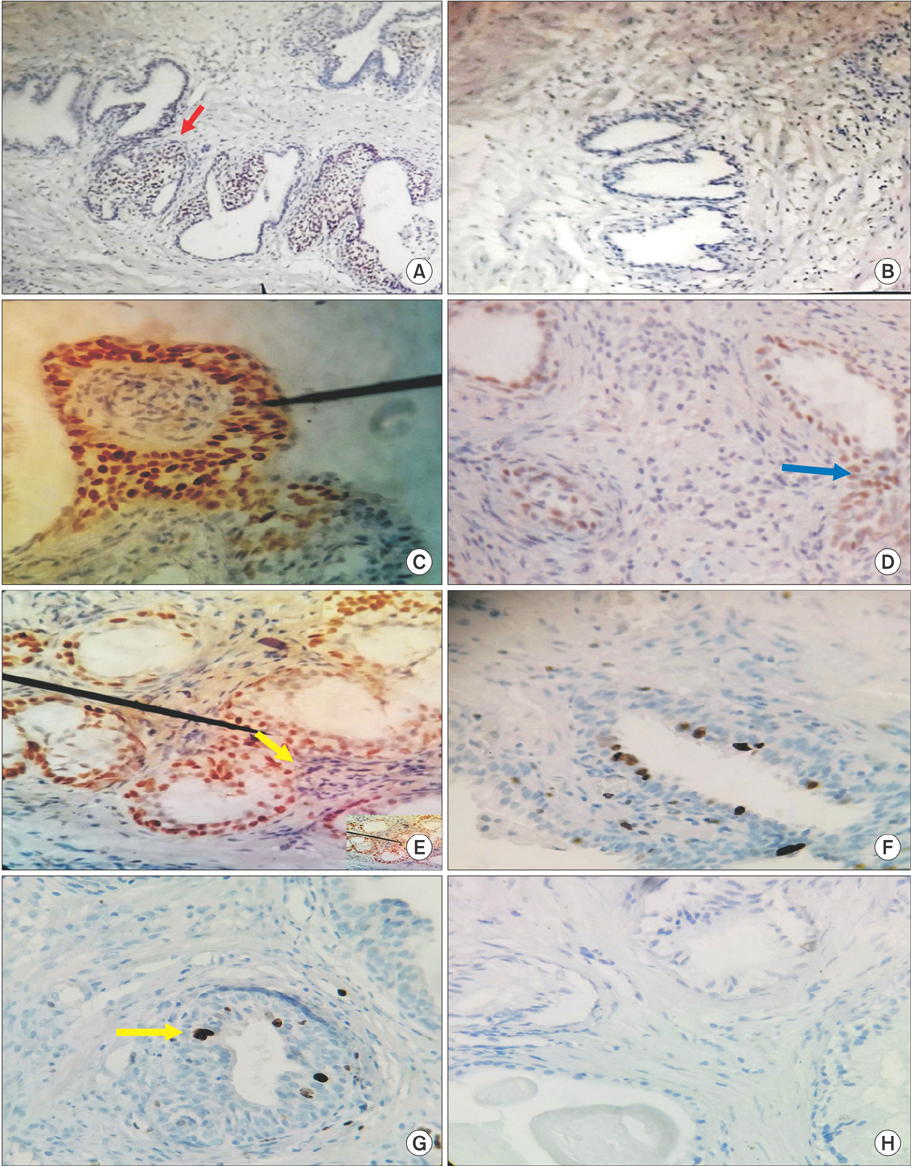
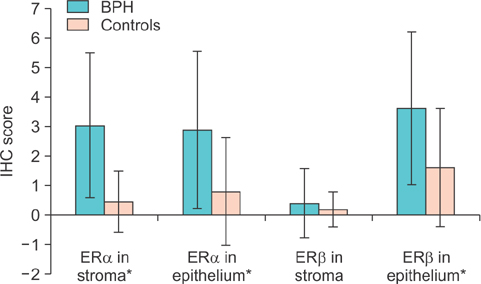
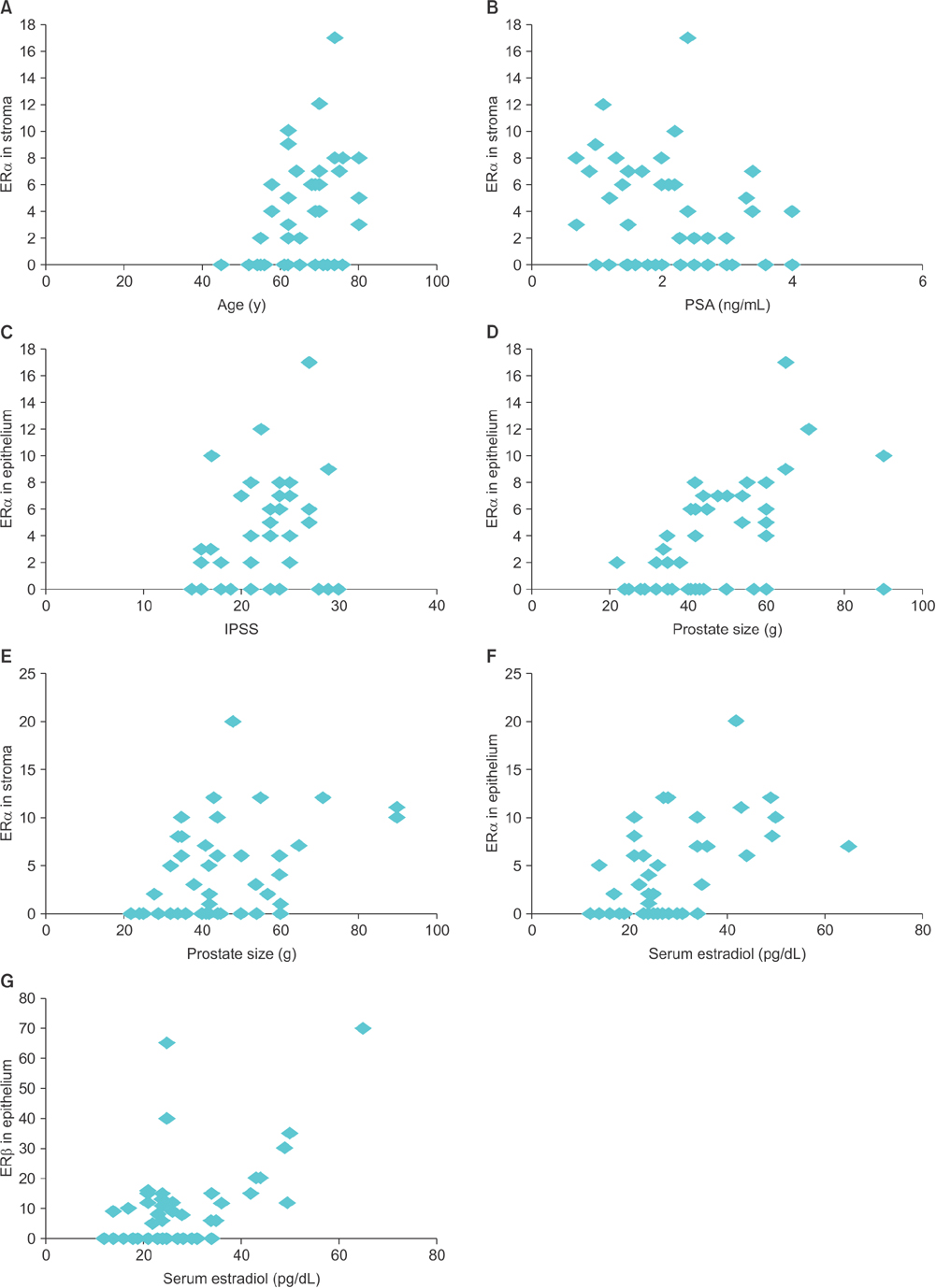
A total of 45 patients with BPH undergoing transurethral resection of the prostate and 22 patients with bladder cancer with normal prostate undergoing surveillance cystoscopy were studied as cases and controls, respectively. Quantitative immunolabeling of ER subtypes was scored by use of a semiquantitative scale. Also, correlations were assessed between ER levels in prostate and various measures of BPH.
RESULTS
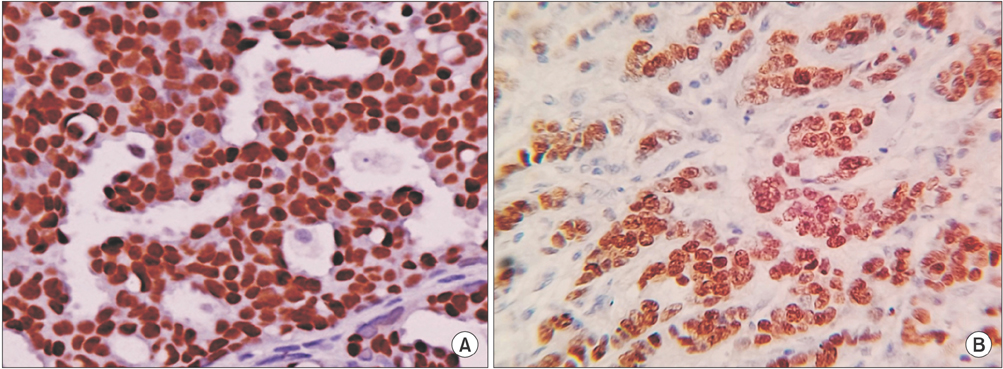
Overall, we found strong immunostaining for ERα in stroma and for ERβ in epithelium, respectively. The IHC score for ERα differed significantly between BPH patients and controls in both stroma (p≤0.001) and epithelium (p=0.008), respectively. The ERβ IHC score was also significantly higher in the epithelium of BPH patients (p=0.01). Also, we found a significant correlation between prostatic ER levels and various clinical measures of BPH.
CONCLUSIONS
ERs may play an important role in the pathogenesis of BPH.
Keyword
MeSH Terms
Figure
Reference
-
1. Barry MJ. Epidemiology and natural history of benign prostatic hyperplasia. Urol Clin North Am. 1990; 17:495–507.2. Castagnetta LA, Carruba G. Human prostate cancer: a direct role for oestrogens. In : Bock GR, Goode JA, editors. Non-reproductive actions of sex steroids. Chichester: John Wiley Sons;1995. p. 269–289.3. Prins GS, Korach KS. The role of estrogens and estrogen receptors in normal prostate growth and disease. Steroids. 2008; 73:233–244.4. Risbridger GP, Bianco JJ, Ellem SJ, McPherson SJ. Oestrogens and prostate cancer. Endocr Relat Cancer. 2003; 10:187–191.5. Greene GL, Gilna P, Waterfield M, Baker A, Hort Y, Shine J. Sequence and expression of human estrogen receptor complementary DNA. Science. 1986; 231:1150–1154.6. Mosselman S, Polman J, Dijkema R. ER beta: identification and characterization of a novel human estrogen receptor. FEBS Lett. 1996; 392:49–53.7. Tsurusaki T, Aoki D, Kanetake H, Inoue S, Muramatsu M, Hishikawa Y, et al. Zone-dependent expression of estrogen receptors alpha and beta in human benign prostatic hyperplasia. J Clin Endocrinol Metab. 2003; 88:1333–1340.8. Schulze H, Claus S. Histological localization of estrogen receptors in normal and diseased human prostates by immunocytochemistry. Prostate. 1990; 16:331–343.9. Brenner RM, West NB, McClellan MC. Estrogen and progestin receptors in the reproductive tract of male and female primates. Biol Reprod. 1990; 42:11–19.10. Royuela M, de Miguel MP, Bethencourt FR, Sánchez-Chapado M, Fraile B, Arenas MI, et al. Estrogen receptors alpha and beta in the normal, hyperplastic and carcinomatous human prostate. J Endocrinol. 2001; 168:447–454.11. Ehara H, Koji T, Deguchi T, Yoshii A, Nakano M, Nakane PK, et al. Expression of estrogen receptor in diseased human prostate assessed by non-radioactive in situ hybridization and immunohistochemistry. Prostate. 1995; 27:304–313.12. Prins GS, Marmer M, Woodham C, Chang W, Kuiper G, Gustafsson JA, et al. Estrogen receptor-beta messenger ribonucleic acid ontogeny in the prostate of normal and neonatally estrogenized rats. Endocrinology. 1998; 139:874–883.13. Mäkelä S, Strauss L, Kuiper G, Valve E, Salmi S, Santti R, et al. Differential expression of estrogen receptors alpha and beta in adult rat accessory sex glands and lower urinary tract. Mol Cell Endocrinol. 2000; 164:109–116.14. Fixemer T, Remberger K, Bonkhoff H. Differential expression of the estrogen receptor beta (ERbeta) in human prostate tissue, premalignant changes, and in primary, metastatic, and recurrent prostatic adenocarcinoma. Prostate. 2003; 54:79–87.15. Lau KM, LaSpina M, Long J, Ho SM. Expression of estrogen receptor (ER)-alpha and ER-beta in normal and malignant prostatic epithelial cells: regulation by methylation and involvement in growth regulation. Cancer Res. 2000; 60:3175–3182.16. Fujimura T, Takahashi S, Urano T, Ogawa S, Ouchi Y, Kitamura T, et al. Differential expression of estrogen receptor beta (ERbeta) and its C-terminal truncated splice variant ERbetacx as prognostic predictors in human prostatic cancer. Biochem Biophys Res Commun. 2001; 289:692–699.17. Nicholson TM, Sehgal PD, Drew SA, Huang W, Ricke WA. Sex steroid receptor expression and localization in benign prostatic hyperplasia varies with tissue compartment. Differentiation. 2013; 85:140–149.18. Weihua Z, Warner M, Gustafsson JA. Estrogen receptor beta in the prostate. Mol Cell Endocrinol. 2002; 193:1–5.19. Prins GS, Birch L, Couse JF, Choi I, Katzenellenbogen B, Korach KS. Estrogen imprinting of the developing prostate gland is mediated through stromal estrogen receptor alpha: studies with alphaERKO and betaERKO mice. Cancer Res. 2001; 61:6089–6097.20. Dupont S, Krust A, Gansmuller A, Dierich A, Chambon P, Mark M. Effect of single and compound knockouts of estrogen receptors alpha (ERalpha) and beta (ERbeta) on mouse reproductive phenotypes. Development. 2000; 127:4277–4291.21. Nicholson TM, Moses MA, Uchtmann KS, Keil KP, Bjorling DE, Vezina CM, et al. Estrogen receptor-α is a key mediator and therapeutic target for bladder complications of benign prostatic hyperplasia. J Urol. 2015; 193:722–729.22. Allred DC, Bustamante MA, Daniel CO, Gaskill HV, Cruz AB Jr. Immunocytochemical analysis of estrogen receptors in human breast carcinomas. Evaluation of 130 cases and review of the literature regarding concordance with biochemical assay and clinical relevance. Arch Surg. 1990; 125:107–113.23. Pasquali D, Staibano S, Prezioso D, Franco R, Esposito D, Notaro A, et al. Estrogen receptor beta expression in human prostate tissue. Mol Cell Endocrinol. 2001; 178:47–50.24. Leav I, Lau KM, Adams JY, McNeal JE, Taplin ME, Wang J, et al. Comparative studies of the estrogen receptors beta and alpha and the androgen receptor in normal human prostate glands, dysplasia, and in primary and metastatic carcinoma. Am J Pathol. 2001; 159:79–92.25. Shapiro E, Huang H, Masch RJ, McFadden DE, Wilson EL, Wu XR. Immunolocalization of estrogen receptor alpha and beta in human fetal prostate. J Urol. 2005; 174:2051–2053.26. Buchanan DL, Kurita T, Taylor JA, Lubahn DB, Cunha GR, Cooke PS. Role of stromal and epithelial estrogen receptors in vaginal epithelial proliferation, stratification, and cornification. Endocrinology. 1998; 139:4345–4352.27. Risbridger G, Wang H, Young P, Kurita T, Wang YZ, Lubahn D, et al. Evidence that epithelial and mesenchymal estrogen receptor-alpha mediates effects of estrogen on prostatic epithelium. Dev Biol. 2001; 229:432–442.28. Kozák I, Bartsch W, Krieg M, Voigt KD. Nuclei of stroma: site of highest estrogen concentration in human benign prostatic hyperplasia. Prostate. 1982; 3:433–438.29. Imamov O, Morani A, Shim GJ, Omoto Y, Thulin-Andersson C, Warner M, et al. Estrogen receptor beta regulates epithelial cellular differentiation in the mouse ventral prostate. Proc Natl Acad Sci U S A. 2004; 101:9375–9380.30. Krege JH, Hodgin JB, Couse JF, Enmark E, Warner M, Mahler JF, et al. Generation and reproductive phenotypes of mice lacking estrogen receptor beta. Proc Natl Acad Sci U S A. 1998; 95:15677–15682.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Immunocytochemical Study Of Estrogen Receptor In The Prostate
- A Prominently Large Glans penis as a Possible sign of Benign Prostatic Hyperplasia
- The Possibility of the Expert System for Benign Prostatic Hyperplasia in Symptomatic Prostatism, Using Symptom Scores, Prostatic Size and Other Factors
- The influence of age and endocrine factors on the volume of benign prostatic hyperplasia
- The role of serum prostate specific antigen in prostatic cancer and benign prostatic hyperplasia