Ann Dermatol.
2016 Dec;28(6):704-710. 10.5021/ad.2016.28.6.704.
Serum Procalcitonin Level Reflects the Severity of Cellulitis
- Affiliations
-
- 1Department of Dermatology, Wonkwang University School of Medicine, Iksan, Korea. ej2000dr@naver.com
- 2Department of Dermatology, Gunsan Medical Center, Gunsan, Korea.
- KMID: 2368120
- DOI: http://doi.org/10.5021/ad.2016.28.6.704
Abstract
- BACKGROUND
Cellulitis is a common bacterial infection of the superficial skin. Procalcitonin is one of the precursor proteins of calcitonin, its levels are elevated in bacterial infection, and it has been established as a diagnostic marker for severe bacterial infections.
OBJECTIVE
This study evaluated the clinical usefulness of procalcitonin for predicting disease severity and prognosis of cellulitis.
METHODS
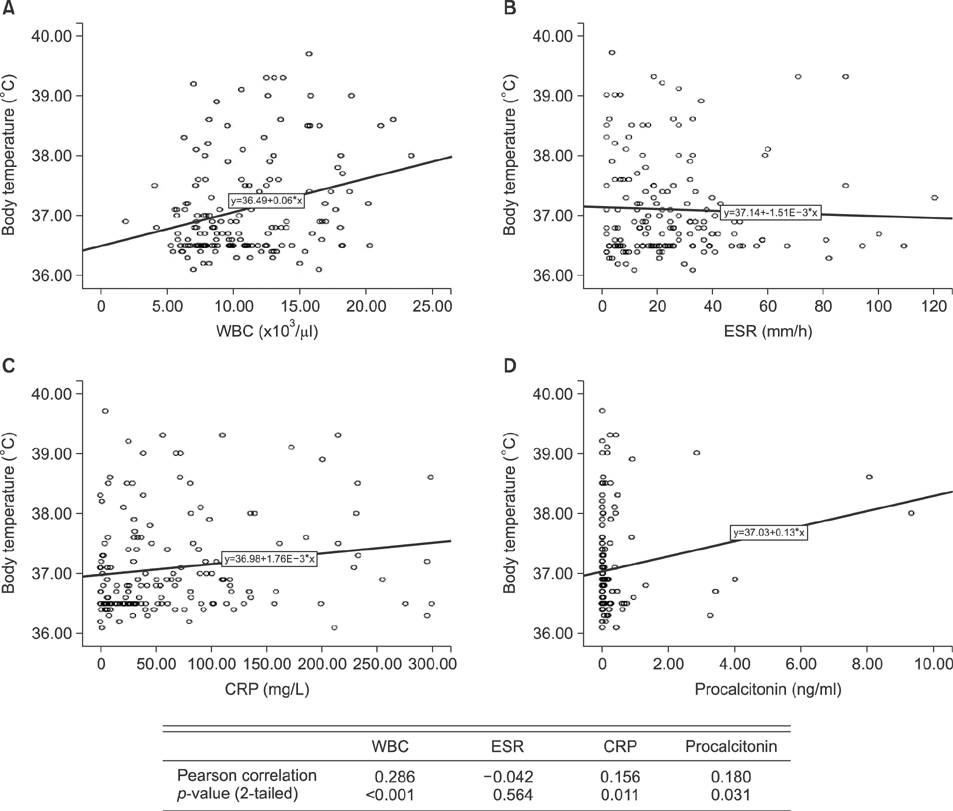
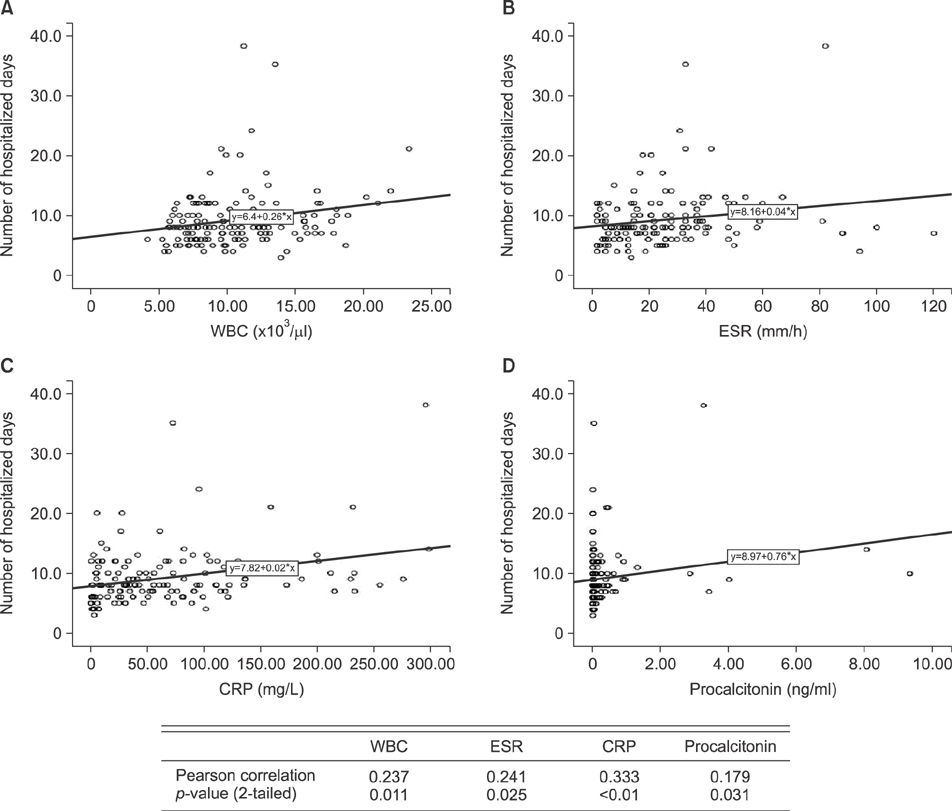
We reviewed the medical records of 160 patients diagnosed with cellulitis in the past 3 years. Body temperature, procalcitonin, white blood cell (WBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels were measured on their first day of admission. The associations of procalcitonin, WBC, ESR, and CRP with the body temperature and the number of hospitalized days were assessed.
RESULTS
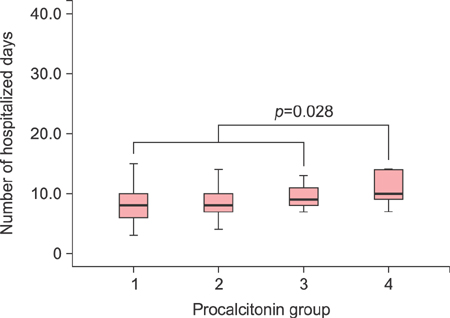
Procalcitonin, WBC, and CRP showed a positive correlation with body temperature. In addition, procalcitonin, WBC, ESR, and CRP showed a positive correlation with number of hospitalized days (p<0.05).
CONCLUSION
In patients diagnosed with cellulitis, proclacitonin was a helpful parameter to indicate the severity of disease and also a useful predictor of prognosis.
Keyword
MeSH Terms
Figure
Reference
-
1. van Rossum AM, Wulkan RW, Oudesluys-Murphy AM. Procalcitonin as an early marker of infection in neonates and children. Lancet Infect Dis. 2004; 4:620–630.
Article2. Russwurm S, Wiederhold M, Oberhoffer M, Stonans I, Zipfel PF, Reinhart K. Molecular aspects and natural source of procalcitonin. Clin Chem Lab Med. 1999; 37:789–797.
Article3. Müller B, White JC, Nylén ES, Snider RH, Becker KL, Habener JF. Ubiquitous expression of the calcitonin-i gene in multiple tissues in response to sepsis. J Clin Endocrinol Metab. 2001; 86:396–404.
Article4. Schuetz P, Albrich W, Christ-Crain M, Chastre J, Mueller B. Procalcitonin for guidance of antibiotic therapy. Expert Rev Anti Infect Ther. 2010; 8:575–587.
Article5. Kim SI, Shim BY, You HY, Jung J, Wie SH, Kim YR, et al. Clinical usefulness of procalcitonin in febrile Patients; comparison with erythrocyte sedimentation rate and C-reactive protein. Korean J Infect Dis. 2000; 32:129–134.6. Zeng M, Guo Z, Shen S, Liu S. Value of serum procalcitonin and interleukin-6 in patients with bullous impetigo and staphylococcal scalded skin syndrome. J Dermatol. 2014; 41:1028–1029.
Article7. Saeed K, Ahmad N, Dryden M. The value of procalcitonin measurement in localized skin and skin structure infection, diabetic foot infections, septic arthritis and osteomyelitis. Expert Rev Mol Diagn. 2014; 14:47–54.
Article8. Eder J, Hlavin G, Haushofer A, Trubert-Exinger D, Trautinger F. Correlation of serum procalcitonin with the severity of skin and skin structure infections-a pilot study. J Dtsch Dermatol Ges. 2012; 10:564–571.9. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993; 341:515–518.
Article10. Gendrel D, Bohuon C. Procalcitonin, a marker of bacterial infection. Infection. 1997; 25:133–134.
Article11. Schröder J, Staubach KH, Zabel P, Stüber F, Kremer B. Procalcitonin as a marker of severity in septic shock. Langenbecks Arch Surg. 1999; 384:33–38.
Article12. Ugarte H, Silva E, Mercan D, De Mendonça A, Vincent JL. Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med. 1999; 27:498–504.
Article13. Viallon A, Zeni F, Lambert C, Pozzetto B, Tardy B, Venet C, et al. High sensitivity and specificity of serum procalcitonin levels in adults with bacterial meningitis. Clin Infect Dis. 1999; 28:1313–1316.
Article14. Brunkhorst FM, Heinz U, Forycki ZF. Kinetics of procalcitonin in iatrogenic sepsis. Intensive Care Med. 1998; 24:888–889.
Article15. Jaye DL, Waites KB. Clinical applications of C-reactive protein in pediatrics. Pediatr Infect Dis J. 1997; 16:735–746.
Article16. Korppi M, Heiskanen-Kosma T, Leinonen M. White blood cells, C-reactive protein and erythrocyte sedimentation rate in pneumococcal pneumonia in children. Eur Respir J. 1997; 10:1125–1129.
Article17. Grønlie M, Hjortdahl P. The erythrocyte sedimentation rate; its use and usefulness in primary health care. Scand J Prim Health Care. 1991; 9:97–102.
Article18. Melbye H, Straume B, Brox J. Laboratory tests for pneumonia in general practice: the diagnostic values depend on the duration of illness. Scand J Prim Health Care. 1992; 10:234–240.
Article19. Hirschmann JV, Raugi GJ. Lower limb cellulitis and its mimics: part I. Lower limb cellulitis. J Am Acad Dermatol. 2012; 67:163.e1-e12. quiz 175-176.20. Na SY, Lee HY, Baek JO, Roh JY, Lee JR. A case of cellulitis associated with coral injury. Ann Dermatol. 2008; 20:212–215.
Article21. Lazzarini L, Conti E, Tositti G, de Lalla F. Erysipelas and cellulitis: clinical and microbiological spectrum in an Italian tertiary care hospital. J Infect. 2005; 51:383–389.
Article22. Rast AC, Knobel D, Faessler L, Kutz A, Felder S, Laukemann S, et al. Use of procalcitonin, C-reactive protein and white blood cell count to distinguish between lower limb erysipelas and deep vein thrombosis in the emergency department: a prospective observational study. J Dermatol. 2015; 42:778–785.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Klebsiella pneumoniae Cellulitis Associated with Osteomyelitis was Suspected by Highly Elevated Inflammatory Marker Serum Procalcitonin
- Role of the Neutrophil-to-Lymphocyte Ratio as a Predictor of Prognosis in Cellulitis
- A Comparative Study between Cellulitis and Necrotizing Fasciitis
- Usefulness of Measuring Serum Procalcitonin Levels in Patients with Inflammatory Bowel Disease
- Predictive value of procalcitonin for bacteremia in patients with pneumonia in the emergency department