Ann Dermatol.
2017 Feb;29(1):26-32. 10.5021/ad.2017.29.1.26.
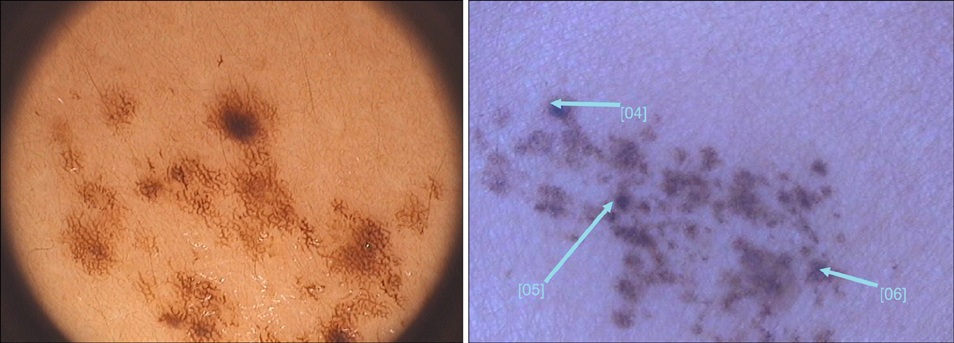
Dermoscopic Features of Small, Medium, and Large-Sized Congenital Melanocytic Nevi
- Affiliations
-
- 1Department of Dermatology, Bezmialem Vakif University, Istanbul, Turkey. fpelinozgen@hotmail.com
- KMID: 2368024
- DOI: http://doi.org/10.5021/ad.2017.29.1.26
Abstract
- BACKGROUND
Congenital melanocytic nevi (CMN) are present at birth. It is well known that the presence of large-sized congenital nevus in early life could predict a major risk of developing melanoma.
OBJECTIVE
To investigate the clinical and dermoscopic features of the CMN, to search for and highlight any differences between small-sized, medium-sized, large-sized CMN.
METHODS
A nonrandomized observational study was performed. A total of 108 melanocytic nevi were analysed by clinical and dermoscopic examination.
RESULTS
Of the subjects, 57.4% were aged less than 16 years, 42.6% were aged 16 and more. Of the nevi, 26 had reticular pattern (24.1%), 35 had globular pattern (32.4%), 13 had reticular-globular pattern (12.0%), 16 had homogeneous pattern (14.8%), 6 had reticular-homogeneous pattern (5.6%), 2 had globular-homogeneous pattern (1.9%), 7 had cobblestone pattern (6.5%), 3 had reticular patchy pattern (2.8%). Atypical dots and globules, focal hypopigmentation and perifollicular hypopigmentation are the most common dermoscopic features of CMN. The rarest dermoscopic feature is the blue-whitish veil.
CONCLUSION
Most of the dermoscopic features related with dysplastic nevi up to the present, such as atypical dots and globules, focal hypopigmentation, perifollicular hypopigmentation were observed in CMN, in our study. Congenital nevus and dysplastic nevi may share the same dermoscopic features, therefore it is important to know it is found at birth or not.
Keyword
MeSH Terms
Figure
Reference
-
1. Marghoob AA. Congenital melanocytic nevi. Evaluation and management. Dermatol Clin. 2002; 20:607–616.2. Makkar HS, Frieden IJ. Congenital melanocytic nevi: an update for the pediatrician. Curr Opin Pediatr. 2002; 14:397–403.
Article3. Castilla EE, da Graça Dutra M, Orioli-Parreiras IM. Epidemiology of congenital pigmented naevi: I. incidence rates and relative frequencies. Br J Dermatol. 1981; 104:307–315.
Article4. Ingordo V, Gentile C, Iannazzone SS, Cusano F, Naldi L. Congenital melanocytic nevus: an epidemiologic study in Italy. Dermatology. 2007; 214:227–230.
Article5. Tannous ZS, Mihm MC Jr, Sober AJ, Duncan LM. Congenital melanocytic nevi: clinical and histopathologic features, risk of melanoma, and clinical management. J Am Acad Dermatol. 2005; 52:197–203.6. Clemmensen OJ, Kroon S. The histology of “congenital features” in early acquired melanocytic nevi. J Am Acad Dermatol. 1988; 19:742–746.
Article7. Mizushima J, Nogita T, Higaki Y, Horikoshi T, Kawashima M. Dormant melanocytes in the dermis: do dermal melanocytes of acquired dermal melanocytosis exist from birth? Br J Dermatol. 1998; 139:349–350.
Article8. Alikhan A, Ibrahimi OA, Eisen DB. Congenital melanocytic nevi: where are we now? Part I. clinical presentation, epidemiology, pathogenesis, histology, malignant transformation, and neurocutaneous melanosis. J Am Acad Dermatol. 2012; 67:495.e1–495.e17. quiz 512-514.9. Viana AC, Gontijo B, Bittencourt FV. Giant congenital melanocytic nevus. An Bras Dermatol. 2013; 88:863–878.
Article10. Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. 3rd ed. Philadelphia, London: Elsevier Saunders;2012. p. 1871–1876.11. Kovalyshyn I, Braun R, Marghoob A. Congenital melanocytic naevi. Australas J Dermatol. 2009; 50:231–240. quiz 241-242.
Article12. Kittler H, Rosendahl C, Cameron A, Tschandl P. An algorithmic method based on pattern analysis. Dermatoscopy. Vienna: Facultas.wuv;2011. p. 29–35.13. Lin J, Koga H, Takata M, Saida T. Dermoscopy of pigmented lesions on mucocutaneous junction and mucous membrane. Br J Dermatol. 2009; 161:1255–1261.
Article14. Watt AJ, Kotsis SV, Chung KC. Risk of melanoma arising in large congenital melanocytic nevi: a systematic review. Plast Reconstr Surg. 2004; 113:1968–1974.
Article15. Krengel S, Hauschild A, Schäfer T. Melanoma risk in congenital melanocytic naevi: a systematic review. Br J Dermatol. 2006; 155:1–8.
Article16. Sahin S, Levin L, Kopf AW, Rao BK, Triola M, Koenig K, et al. Risk of melanoma in medium-sized congenital melanocytic nevi: a follow-up study. J Am Acad Dermatol. 1998; 39:428–433.
Article17. Zaal LH, Mooi WJ, Klip H, van der Horst CM. Risk of malignant transformation of congenital melanocytic nevi: a retrospective nationwide study from The Netherlands. Plast Reconstr Surg. 2005; 116:1902–1909.
Article18. Yun SJ, Kwon OS, Han JH, Kweon SS, Lee MW, Lee DY, et al. Clinical characteristics and risk of melanoma development from giant congenital melanocytic naevi in Korea: a nationwide retrospective study. Br J Dermatol. 2012; 166:115–123.
Article19. Moscarella E, Zalaudek I, Ferrara G, Manzo M, Savarese I, Argenziano G. Problematic melanocytic lesions in children. Expert Rev Dermatol. 2009; 4:249–261.
Article20. Braun RP, Calza AM, Krischer J, Saurat JH. The use of digital dermoscopy for the follow-up of congenital nevi: a pilot study. Pediatr Dermatol. 2001; 18:277–281.
Article21. Oliveria SA, Geller AC, Dusza SW, Marghoob AA, Sachs D, Weinstock MA, et al. The Framingham school nevus study: a pilot study. Arch Dermatol. 2004; 140:545–551.22. Seidenari S, Pellacani G, Martella A, Giusti F, Argenziano G, Buccini P, et al. Instrument-, age- and site-dependent variations of dermoscopic patterns of congenital melanocytic naevi: a multicentre study. Br J Dermatol. 2006; 155:56–61.
Article23. Changchien L, Dusza SW, Agero AL, Korzenko AJ, Braun RP, Sachs D, et al. Age- and site-specific variation in the dermoscopic patterns of congenital melanocytic nevi: an aid to accurate classification and assessment of melanocytic nevi. Arch Dermatol. 2007; 143:1007–1014.24. Stinco G, Argenziano G, Favot F, Valent F, Patrone P. Absence of clinical and dermoscopic differences between congenital and noncongenital melanocytic naevi in a cohort of 2-year-old children. Br J Dermatol. 2011; 165:1303–1307.
Article25. Haliasos EC, Kerner M, Jaimes N, Zalaudek I, Malvehy J, Hofmann-Wellenhof R, et al. Dermoscopy for the pediatric dermatologist part III: dermoscopy of melanocytic lesions. Pediatr Dermatol. 2013; 30:281–293.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Malignant Melanoma Possibly Arising in a Medium-sized Congenital Melanocytic Nevus
- A Case of Malignant Melanoma Arising in Small Congenital Melanocytic Nevus
- Malignant Melanoma on Congenital Melanocytic Nevus
- A Case of Congenital Melanocytic Nevi with Unusual Cutaneous Manifestation
- Surgical Treatment by Curettage and Dermatome in Two Cases of Giant Congenital Melanocytic Nevi