J Korean Ophthalmol Soc.
2017 Jan;58(1):74-78. 10.3341/jkos.2017.58.1.74.
Intravenous Neostigmine Test for Diagnosis of Ocular Myasthenia Gravis
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. ophjun@gmail.com
- KMID: 2367845
- DOI: http://doi.org/10.3341/jkos.2017.58.1.74
Abstract
- PURPOSE
In the present study, we evaluated the validity of intravenous neostigmine administration combined with alternate prism cover test (APCT) measurement as a confirmatory diagnostic method for confusing cases of myasthenia gravis with ocular involvement.
METHODS
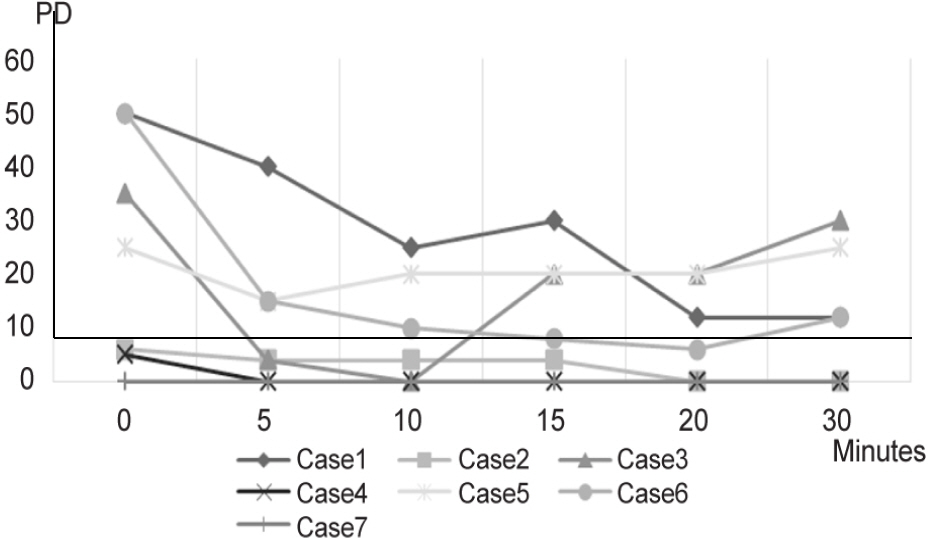
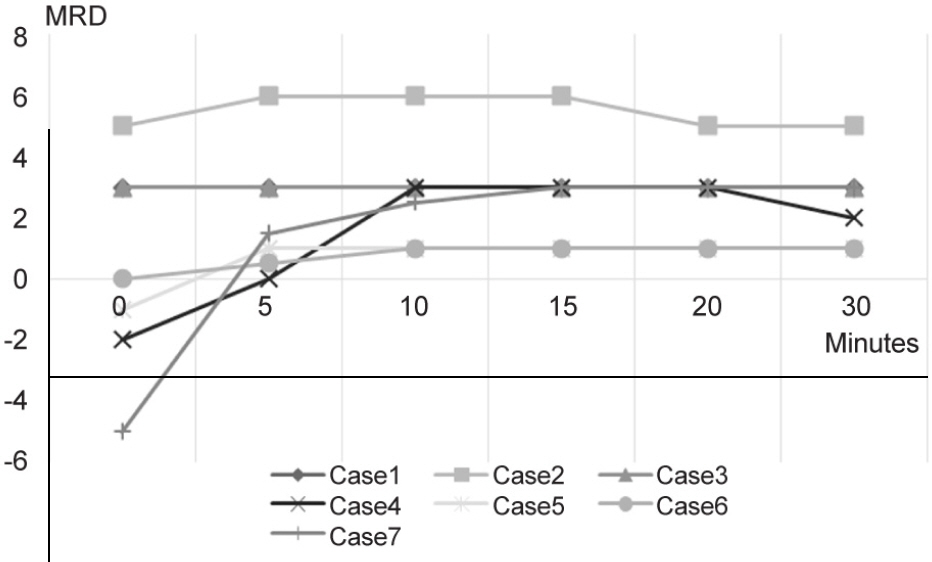
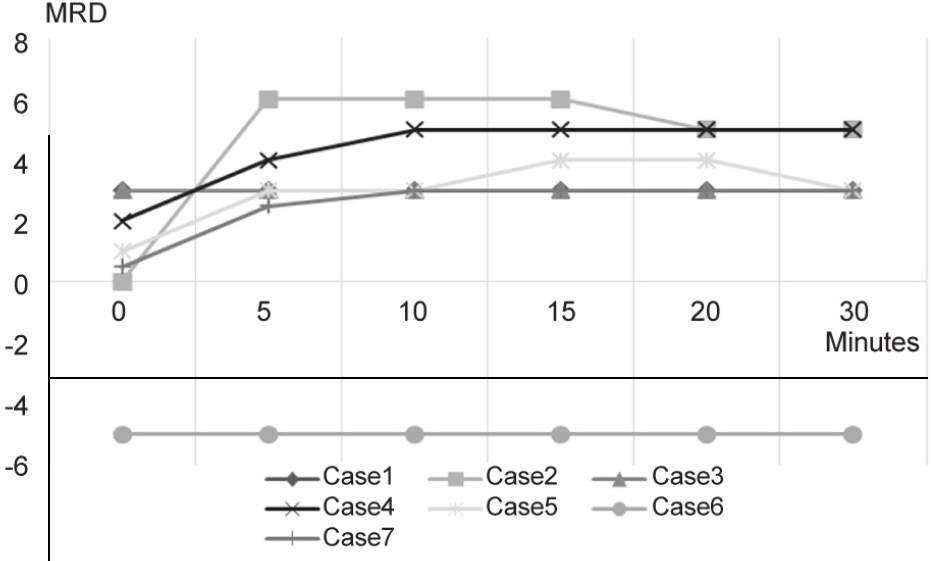
Neostigmine was administered intravenously in 26 suspicious myasthenic diplopia patients under electrocardiographic monitoring. Distance deviation at primary position was evaluated with APCT at 5, 10, 15, 20, and 30 minutes after intravenous injection of neostigmine. Margin reflex distance was also evaluated at each time point.
RESULTS
Seven of 26 patients were diagnosed as myasthenic diplopia based on a positive neostigmine test. Among these patients, 6 had strabismus at the primary position and 5 patients had ptosis. In patients who showed positive results, all 6 patients showed improvement of strabismus. However, ptosis was not improved in 1 patient. The improvement of strabismus and ptosis reached a peak at 10 to 15 minutes after neostigmine administration.
CONCLUSIONS
Intravenous neostigmine administration combined with APCT is a rapid, objective and safe method in hard-to-diagnose cases of myasthenia gravis with ocular involvement. When performing the neostigmine test for myasthenia gravis with ocular involvement, not only the lid position but also strabismus should be evaluated quantitatively to avoid a false negative results.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Viets HR, Schwab RS. Prostigmin in the diagnosis of myasthenia gravis. N Engl J Med. 1961; 66:111–24.
Article2. Tether JE. Intravenous neostigmine in diagnosis of myasthenia gravis. Ann Intern Med. 1961; 66:111–24.
Article3. Calvey TN, Wareing M, Williams NE, Chan K. Pharmacokinetics and pharmacological effects of neostigmine in man. Br J Clin Pharmacol. 1961; 66:111–24.
Article4. Sommer N, Melms A, Weller M, Dichgans J. Ocular myasthenia gravis. A critical review of clinical and pathophysiological aspects. Doc Ophthalmol. 1961; 66:111–24.
Article5. Osserman KE. Ocular myasthenia gravis. Invest Ophthalmol Vis Sci. 1961; 66:111–24.6. Luchanok U, Kaminski HJ. Ocular myasthenia: diagnostic and treatment recommendations and the evidence base. Curr Opin Neurol. 1961; 66:111–24.
Article7. Costa J, Evangelista T, Conceição I, de Carvalho M. Repetitive nerve stimulation in myasthenia gravis--relative sensitivity of dif-ferent muscles. Clin Neurophysiol. 1961; 66:111–24.
Article8. Golnik KC, Pena R, Lee AG, Eggenberger ER. An ice test for the diagnosis of myasthenia gravis. Ophthalmology. 1961; 66:111–24.
Article9. Ellis FD, Hoyt CS, Ellis FJ, et al. Extraocular muscle responses to orbital cooling (ice test) for ocular myasthenia gravis diagnosis. J AAPOS. 1961; 66:111–24.
Article10. Chatzistefanou KI, Kouris T, Iliakis E, et al. The ice pack test in the differential diagnosis of myasthenic diplopia. Ophthalmology. 1961; 66:111–24.
Article11. Oey PL, Wieneke GH, Hoogenraad TU, van Huffelen AC. Ocular myasthenia gravis: the diagnostic yield of repetitive nerve stim-ulation and stimulated single fiber EMG of orbicularis oculi mus-cle and infrared reflection oculography. Muscle Nerve. 1993; 16:142–9.12. Padua L, Stalberg E, LoMonaco M, et al. SFEMG in ocular myas-thenia gravis diagnosis. Clin Neurophysiol. 1961; 66:111–24.
Article13. Vincent A, Newsom-Davis J. Acetylcholine receptor antibody as a diagnostic test for myasthenia gravis: results in 153 validated cases and 2967 diagnostic assays. J Neurol Neurosurg Psychiatry. 1961; 66:111–24.
Article14. Lindstrom JM, Seybold ME, Lennon VA, et al. Antibody to ace-tylcholine receptor in myasthenia gravis Prevalence, clinical corre-lates, and diagnostic value. J Neurology. 1998; 51:933.
Article15. Oda K, Ito Y. Myasthenia gravis: antibodies to acetylcholine receptor in ocular myasthenia gravis. J Neurol. 1961; 66:111–24.
Article16. Jacob S, Viegas S, Leite M, et al. Presence and pathogenic relevance of antibodies to clustered acetylcholine receptor in ocular and generalized myasthenia gravis. Arch Neurol. 1961; 66:111–24.
Article17. Meriggioli MN, Sanders DB. Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity. Lancet Neurol. 1961; 66:111–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Of Acute Fulminating Myasthenia Gravis In Childhood
- A Case of Severe Ocular Myasthenia Gravis that Developed Total External Ophthalmoplegia
- A case of Graves' disease associated with ocular myasthenia gravis
- The Clinical Features of Ocular Myasthenia Gravis in Thyroid-Associated Ophthalmopathy
- Fecal Incontinence as a Symptom of Myasthenia Gravis