Ann Pediatr Endocrinol Metab.
2016 Dec;21(4):235-239. 10.6065/apem.2016.21.4.235.
An 11-month-old girl with central precocious puberty caused by hypothalamic hamartoma
- Affiliations
-
- 1Department of Pediatrics, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. pedendo@paik.ac.kr
- KMID: 2366816
- DOI: http://doi.org/10.6065/apem.2016.21.4.235
Abstract
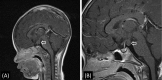
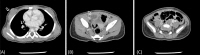
- Central precocious puberty (CPP) is caused by premature activation of the hypothalamic-gonadal axis, and must be treated adequately. In particular, CPP that occurs at a relatively young age or in boys is likely to be caused by an organic lesion. Hypothalamic hamartoma (HH) is the most common organic cause of CPP. The present case report describes an 11-month-old female infant who presented with vaginal bleeding and rapidly progressive secondary sex characteristics from the age of 6 months. She was diagnosed with CPP following the detection of HH via magnetic resonance imaging. The infant girl was successfully treated with gonadotropin-releasing hormone agonist. After 6 months, her breast had regressed and clinical and radiological follow-up demonstrated stable findings with no evidence of tumor growth or secondary sexual characteristics until the fourth year after the initiation of treatment. This patient is the one of the youngest infants presenting with CPP and HH in Korea; treatment was successful over a relatively long follow-up period.
Figure
Reference
-
1. Pescovitz OH, Comite F, Hench K, Barnes K, McNemar A, Foster C, et al. The NIH experience with precocious puberty: diagnostic subgroups and response to short-term luteinizing hormone releasing hormone analogue therapy. J Pediatr. 1986; 108:47–54. PMID: 3080571.
Article2. Shenoy SN, Raja A. Hypothalamic hamartoma with precocious puberty. Pediatr Neurosurg. 2004; 40:249–252. PMID: 15687741.
Article3. Jung H, Parent AS, Ojeda SR. Hypothalamic hamartoma: a paradigm/model for studying the onset of puberty. Endocr Dev. 2005; 8:81–93. PMID: 15722619.4. Ng SM, Kumar Y, Cody D, Smith CS, Didi M. Cranial MRI scans are indicated in all girls with central precocious puberty. Arch Dis Child. 2003; 88:414–418. PMID: 12716713.
Article5. Rousso IH, Kourti M, Papandreou D, Tragiannidis A, Athanasiadou F. Central precocious puberty due to hypothalamic hamartoma in a 7-month-old infant girl. Eur J Pediatr. 2008; 167:583–585. PMID: 17541635.
Article6. Han SK, Chae JH, Kim KJ, Hwang YS, Han TI, Kim IO. Hypothalamic hamartoma: clinical and MRI features and outcome. J Korean Child Neurol Soc. 1997; 5:69–75.7. Lee J, Yu HJ, Kim JY, Kim JH, Lee JI, Shin HJ, et al. Clinical manifestations and treatment of hypothalamic Hamartoma. J Korean Epilepsy Soc. 2013; 17:8–16.8. Debeneix C, Bourgeois M, Trivin C, Sainte-Rose C, Brauner R. Hypothalamic hamartoma: comparison of clinical presentation and magnetic resonance images. Horm Res. 2001; 56:12–18. PMID: 11815722.
Article9. Freeman JL, Coleman LT, Wellard RM, Kean MJ, Rosenfeld JV, Jackson GD, et al. MR imaging and spectroscopic study of epileptogenic hypothalamic hamartomas: analysis of 72 cases. AJNR Am J Neuroradiol. 2004; 25:450–462. PMID: 15037472.10. Kameyama S, Murakami H, Masuda H, Sugiyama I. Minimally invasive magnetic resonance imaging-guided stereotactic radiofrequency thermocoagulation for epileptogenic hypothalamic hamartomas. Neurosurgery. 2009; 65:438–449. PMID: 19687687.
Article11. Mittal S, Mittal M, Montes JL, Farmer JP, Andermann F. Hypothalamic hamartomas. Part 1. Clinical, neuroimaging, and neurophysiological characteristics. Neurosurg Focus. 2013; 34:E6.
Article12. Judge DM, Kulin HE, Page R, Santen R, Trapukdi S. Hypothalamic hamartoma: a source of luteinizing-hormone-releasing factor in precocious puberty. N Engl J Med. 1977; 296:7–10. PMID: 318592.13. Boyko OB, Curnes JT, Oakes WJ, Burger PC. Hamartomas of the tuber cinereum: CT, MR, and pathologic findings. AJNR Am J Neuroradiol. 1991; 12:309–314. PMID: 1902033.14. Striano S, Striano P, Sarappa C, Boccella P. The clinical spectrum and natural history of gelastic epilepsy-hypothalamic hamartoma syndrome. Seizure. 2005; 14:232–239. PMID: 15911357.
Article15. Kuiri-Hänninen T, Sankilampi U, Dunkel L. Activation of the hypothalamic-pituitary-gonadal axis in infancy: minipuberty. Horm Res Paediatr. 2014; 82:73–80. PMID: 25012863.
Article16. de Lange AH, Bocca G. Vaginal bleeding in a 4-month-old preterm girl: extreme minipuberty mimicking central precocious puberty. J Pediatr Endocrinol Metab. 2013; 26:595–597. PMID: 23640937.
Article17. Vogiatzi MG, Pitt M, Oberfield S, Alter CA. Menstrual bleeding as a manifestation of mini-puberty of infancy in severe prematurity. J Pediatr. 2016; 178:292–295. PMID: 27593439.
Article18. Carel JC, Eugster EA, Rogol A, Ghizzoni L, Palmert MR, et al. ESPE-LWPES GnRH Analogs Consensus Conference Group. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics. 2009; 123:e752–e762. PMID: 19332438.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypothalamic hamartoma associated with precocious puberty: case report
- A Case Report of Precocious Puberty in Children Associated with Hypothalamic Hamartoma in Neurofibromatosis Type 1
- Hypothalamic Tumors Causing Precocious Puberty
- A Case of Gelastic Seizure and Hypothalamic Hamartoma
- Treatment of Hypothalamic Hamartoma