Tuberc Respir Dis.
2016 Oct;79(4):241-247. 10.4046/trd.2016.79.4.241.
The Role of Bronchodilators in Preventing Exacerbations of Chronic Obstructive Pulmonary Disease
- Affiliations
-
- 1Insaf Respiratory Research Institute, Wiesbaden, Germany. k.beeh@insaf-wi.de
- KMID: 2365315
- DOI: http://doi.org/10.4046/trd.2016.79.4.241
Abstract
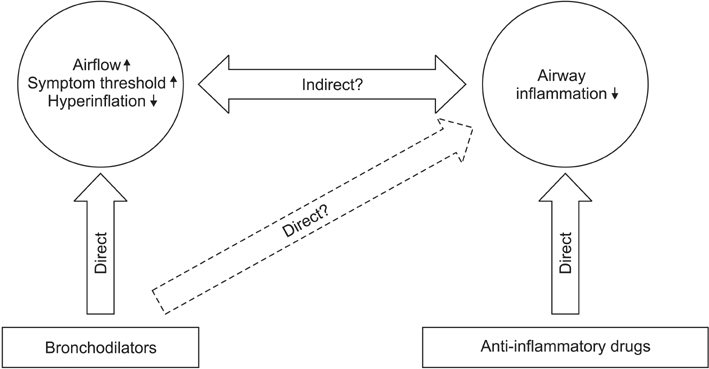
- Bronchodilators are the cornerstone of symptomatic chronic obstructive pulmonary disease (COPD) treatment. They are routinely recommended for symptom reduction, with a preference of long-acting over short-acting drugs. Bronchodilators are classified into two classes based on distinct modes of action, i.e., long-acting antimuscarinics (LAMA, once-daily and twice-daily), and long-acting β2-agonists (LABA, once-daily and twice-daily). In contrast to asthma management, evidence supports the efficacy of both classes of long-acting bronchodilators as monotherapy in preventing COPD exacerbations, with greater efficacy of LAMA drugs versus LABAs. Several novel LAMA/LABA fixed dose combination inhalers are currently approved for COPD maintenance treatment. These agents show superior symptom control to monotherapies, and some of these combinations have also demonstrated superior efficacy in exacerbation prevention versus monotherapies, or combinations of inhaled corticosteroids plus LABA. This review summarizes the current data on clinical effectiveness of bronchodilators alone or in combination to prevent exacerbations of COPD.
MeSH Terms
Figure
Cited by 1 articles
-
Novel glutathione-containing dry-yeast extracts inhibit eosinophilia and mucus overproduction in a murine model of asthma
Yun-Ho Kim, Yean-Jung Choi, Eun-Jung Lee, Min-Kyung Kang, Sin-Hye Park, Dong Yeon Kim, Hyeongjoo Oh, Sang-Jae Park, Young-Hee Kang
Nutr Res Pract. 2017;11(6):461-469. doi: 10.4162/nrp.2017.11.6.461.
Reference
-
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2016 update [Internet]. Global Initiative for Chronic Obstructive Lung Disease;2016. cited 2016 Jul 9. Available from: http://www.goldcopd.org.2. Han MK, Agusti A, Calverley PM, Celli BR, Criner G, Curtis JL, et al. Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med. 2010; 182:598–604.3. Rabe KF, Fabbri LM, Vogelmeier C, Kogler H, Schmidt H, Beeh KM, et al. Seasonal distribution of COPD exacerbations in the Prevention of Exacerbations with Tiotropium in COPD trial. Chest. 2013; 143:711–719.4. Hurst JR, Donaldson GC, Quint JK, Goldring JJ, Baghai-Ravary R, Wedzicha JA. Temporal clustering of exacerbations in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009; 179:369–374.5. Hurst JR, Vestbo J, Anzueto A, Locantore N, Mullerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010; 363:1128–1138.6. Vogelmeier C, Buhl R, Criee CP, Gillissen A, Kardos P, Kohler D, et al. Guidelines for the diagnosis and therapy of COPD issued by Deutsche Atemwegsliga and Deutsche Gesellschaft fur Pneumologie und Beatmungsmedizin. Pneumologie. 2007; 61:e1–e40.7. Appleton S, Poole P, Smith B, Veale A, Lasserson TJ, Chan MM. Long-acting beta2-agonists for poorly reversible chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2006; (3):CD001104.8. Buhl R, Maltais F, Abrahams R, Bjermer L, Derom E, Ferguson G, et al. Tiotropium and olodaterol fixed-dose combination versus mono-components in COPD (GOLD 2-4). Eur Respir J. 2015; 45:969–979.9. Beeh KM, Derom E, Echave-Sustaeta J, Gronke L, Hamilton A, Zhai D, et al. The lung function profile of once-daily tiotropium and olodaterol via Respimat((R)) is superior to that of twice-daily salmeterol and fluticasone propionate via Accuhaler((R)) (ENERGITO((R)) study). Int J Chron Obstruct Pulmon Dis. 2016; 11:193–205.10. Bateman ED, Ferguson GT, Barnes N, Gallagher N, Green Y, Henley M, et al. Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. Eur Respir J. 2013; 42:1484–1494.11. Vogelmeier CF, Bateman ED, Pallante J, Alagappan VK, D'Andrea P, Chen H, et al. Efficacy and safety of once-daily QVA149 compared with twice-daily salmeterol-fluticasone in patients with chronic obstructive pulmonary disease (ILLUMINATE): a randomised, double-blind, parallel group study. Lancet Respir Med. 2013; 1:51–60.12. Wedzicha JA, Decramer M, Seemungal TA. The role of bronchodilator treatment in the prevention of exacerbations of COPD. Eur Respir J. 2012; 40:1545–1554.13. Agarwal R, Aggarwal AN, Gupta D, Jindal SK. Inhaled corticosteroids vs placebo for preventing COPD exacerbations: a systematic review and metaregression of randomized controlled trials. Chest. 2010; 137:318–325.14. Wang J, Nie B, Xiong W, Xu Y. Effect of long-acting beta-agonists on the frequency of COPD exacerbations: a meta-analysis. J Clin Pharm Ther. 2012; 37:204–211.15. Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007; 356:775–789.16. Szafranski W, Cukier A, Ramirez A, Menga G, Sansores R, Nahabedian S, et al. Efficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary disease. Eur Respir J. 2003; 21:74–81.17. Wedzicha JA, Buhl R, Lawrence D, Young D. Monotherapy with indacaterol once daily reduces the rate of exacerbations in patients with moderate-to-severe COPD: Post-hoc pooled analysis of 6 months data from three large phase III trials. Respir Med. 2015; 109:105–111.18. Koch A, Pizzichini E, Hamilton A, Hart L, Korducki L, De Salvo MC, et al. Lung function efficacy and symptomatic benefit of olodaterol once daily delivered via Respimat(R) versus placebo and formoterol twice daily in patients with GOLD 2-4 COPD: results from two replicate 48-week studies. Int J Chron Obstruct Pulmon Dis. 2014; 9:697–714.19. Ferguson GT, Feldman GJ, Hofbauer P, Hamilton A, Allen L, Korducki L, et al. Efficacy and safety of olodaterol once daily delivered via Respimat(R) in patients with GOLD 2-4 COPD: results from two replicate 48-week studies. Int J Chron Obstruct Pulmon Dis. 2014; 9:629–645.20. Vestbo J, Anderson JA, Brook RD, Calverley PM, Celli BR, Crim C, et al. Fluticasone furoate and vilanterol and survival in chronic obstructive pulmonary disease with heightened cardiovascular risk (SUMMIT): a double-blind randomised controlled trial. Lancet. 2016; 387:1817–1826.21. Dusser D, Bravo ML, Iacono P. The effect of tiotropium on exacerbations and airflow in patients with COPD. Eur Respir J. 2006; 27:547–555.22. Niewoehner DE, Rice K, Cote C, Paulson D, Cooper JA Jr, Korducki L, et al. Prevention of exacerbations of chronic obstructive pulmonary disease with tiotropium, a once-daily inhaled anticholinergic bronchodilator: a randomized trial. Ann Intern Med. 2005; 143:317–326.23. Tashkin DP, Celli B, Senn S, Burkhart D, Kesten S, Menjoge S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008; 359:1543–1554.24. Wise RA, Anzueto A, Cotton D, Dahl R, Devins T, Disse B, et al. Tiotropium Respimat inhaler and the risk of death in COPD. N Engl J Med. 2013; 369:1491–1501.25. Vogelmeier C, Hederer B, Glaab T, Schmidt H, Rutten-van Molken MP, Beeh KM, et al. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med. 2011; 364:1093–1103.26. Decramer ML, Chapman KR, Dahl R, Frith P, Devouassoux G, Fritscher C, et al. Once-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGORATE): a randomised, blinded, parallel-group study. Lancet Respir Med. 2013; 1:524–533.27. Wedzicha JA, Calverley PM, Seemungal TA, Hagan G, Ansari Z, Stockley RA, et al. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008; 177:19–26.28. Kerwin E, Hebert J, Gallagher N, Martin C, Overend T, Alagappan VK, et al. Efficacy and safety of NVA237 versus placebo and tiotropium in patients with COPD: the GLOW2 study. Eur Respir J. 2012; 40:1106–1114.29. Feldman G, Maltais F, Khindri S, Vahdati-Bolouri M, Church A, Fahy WA, et al. A randomized, blinded study to evaluate the efficacy and safety of umeclidinium 62.5 mug compared with tiotropium 18 mug in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016; 11:719–730.30. Jones PW, Singh D, Bateman ED, Agusti A, Lamarca R, de Miquel G, et al. Efficacy and safety of twice-daily aclidinium bromide in COPD patients: the ATTAIN study. Eur Respir J. 2012; 40:830–836.31. Institut für Qualität und Wirtschaflichkeit im Gesundheitswesen. Aclidiniumbromid: Nutzenbewertung nach §35 SGB V. A15-45 [Internet]. Köln: IQWIG;2016. cited 2016 Jul 9. Available from: http://www.g-ba.de/downloads/92-975-1206/2016-01-15_Nutzenbewertung-IQWiG_Aclidiniumbromid.pdf.32. Nannini LJ, Lasserson TJ, Poole P. Combined corticosteroid and long-acting beta2-agonist in one inhaler versus long-acting beta2-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012; (9):CD006829.33. Oba Y, Lone NA. Comparative efficacy of inhaled corticosteroid and long-acting beta agonist combinations in preventing COPD exacerbations: a Bayesian network meta-analysis. Int J Chron Obstruct Pulmon Dis. 2014; 9:469–479.34. Calverley P, Pauwels R, Vestbo J, Jones P, Pride N, Gulsvik A, et al. Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 2003; 361:449–456.35. Dransfield MT, Bourbeau J, Jones PW, Hanania NA, Mahler DA, Vestbo J, et al. Once-daily inhaled fluticasone furoate and vilanterol versus vilanterol only for prevention of exacerbations of COPD: two replicate double-blind, parallel-group, randomised controlled trials. Lancet Respir Med. 2013; 1:210–223.36. Petty TL. The combination of ipratropium and albuterol is more effective than either agent alone. Chest. 1995; 107:5 Suppl. 183S–186S.37. Aaron SD, Vandemheen KL, Fergusson D, Maltais F, Bourbeau J, Goldstein R, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2007; 146:545–555.38. Mahler DA, Decramer M, D'Urzo A, Worth H, White T, Alagappan VK, et al. Dual bronchodilation with QVA149 reduces patient-reported dyspnoea in COPD: the BLAZE study. Eur Respir J. 2014; 43:1599–1609.39. Wedzicha JA, Decramer M, Ficker JH, Niewoehner DE, Sandstrom T, Taylor AF, et al. Analysis of chronic obstructive pulmonary disease exacerbations with the dual bronchodilator QVA149 compared with glycopyrronium and tiotropium (SPARK): a randomised, double-blind, parallel-group study. Lancet Respir Med. 2013; 1:199–209.40. Wedzicha JA, Banerji D, Chapman KR, Vestbo J, Roche N, Ayers RT, et al. Indacaterol-Glycopyrronium versus Salmeterol-Fluticasone for COPD. N Engl J Med. 2016; 374:2222–2234.41. Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med. 2015; 3:435–442.42. Institut für Qualität und Wirtschaflichkeit im Gesundheitswesen. Aclidiniumbromid/Formoterol. Nutzenbewertung nach §35 SGB V. A15-06 [Internet]. Köln: IQWIG;2015. cited 2016 Jul 9. Available from: http://www.g-ba.de/downloads/92-975-767/2015-05-04_Nutzenbewertung-IQWiG_A15-06_Aclidiniumbromid-Formoterol.pdf.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pharmacologic Therapies for Preventing Chronic Obstructive Pulmonary Disease Exacerbations: A Comprehensive Review
- Pharmacotherapy for chronic obstructive pulmonary disease
- Pharmacotherapy in Stable Chronic Obstructive Pulmonary Disease
- Sputum Inflammometry to Manage Chronic Obstructive Pulmonary Disease Exacerbations: Beyond Guidelines
- Chronic Obstructive Pulmonary Disease and the Airway Microbiome: What Respirologists Need to Know