J Clin Neurol.
2016 Jan;12(1):49-56. 10.3988/jcn.2016.12.1.49.
A Retrospective 10-Year, Single-Institution Study of Carotid Endarterectomy with a Focus on Elderly Patients
- Affiliations
-
- 1Department of Surgery, Ulsan University Hospital, Ulsan, Korea.
- 2Division of Vascular Surgery, Department of Surgery, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea. twkwon2@amc.seoul.kr
- 3Department of Neurology, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- 4Department of Surgery, Pusan National University Hospital, Busan, Korea.
- KMID: 2364919
- DOI: http://doi.org/10.3988/jcn.2016.12.1.49
Abstract
- BACKGROUND AND PURPOSE
This study evaluated the outcome following surgery for carotid artery stenosis in a single institution during a 10-year period and the relevance of aging to access to surgery.
METHODS
Between January 2001 and December 2010, 649 carotid endarterectomies (CEAs) were performed in 596 patients for internal carotid artery occlusive disease at our institution; 596 patients received unilateral CEAs and 53 patients received bilateral CEAs. Data regarding patient characteristics, comorbidities, stroke, mortality, restenosis, and other surgical complications were obtained from a review of medical records. Since elderly and high-risk patients comprise a significant proportion of the patient group undergoing CEAs, differences in comorbidity and mortality were evaluated according to age when the patients were divided into three age groups: <70 years, 70-79 years, and > or =80 years.
RESULTS
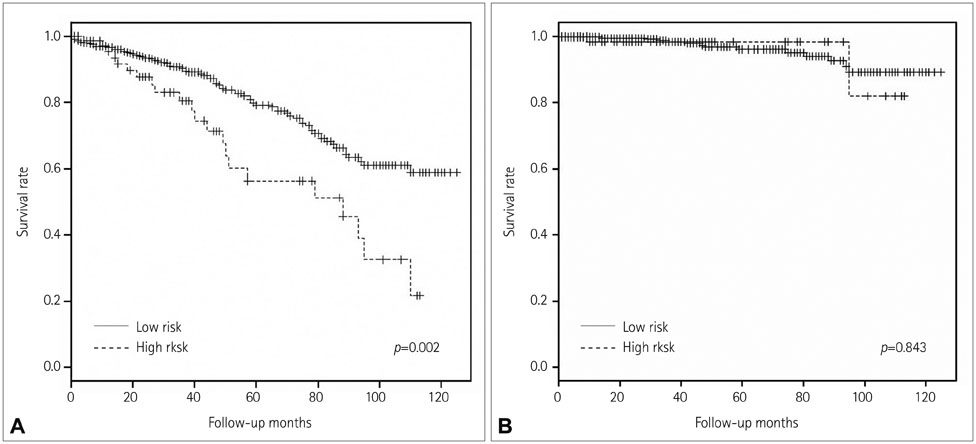
The mean age of the included patients was 67.5 years, and 88% were men. Symptomatic carotid stenosis was observed in 65.7% of patients. The rate of perioperative stroke and death (within 30 days of the procedure) was 1.84%. The overall mortality rate was higher among patients in the 70-79 years and >80 years age groups than among those in the <70 years age group, but there was no significant difference in stroke-related mortality among these three groups.
CONCLUSIONS
CEA over a 10-year period has yielded acceptable outcomes in terms of stroke and mortality. Therefore, since CEA is a safe and effective strategy, it can be performed in elderly patients with acceptable life expectancy.
Keyword
MeSH Terms
Figure
Reference
-
1. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean Stroke Society and clinical research center for stroke. J Stroke. 2013; 15:2–20.
Article2. Eastcott HH, Pickering GW, Rob CG. Reconstruction of internal carotid artery in a patient with intermittent attacks of hemiplegia. Lancet. 1954; 267:994–996.
Article3. Duncan JM, Reul GJ, Ott DA, Kincade RC, Davis JW. Outcomes and risk factors in 1,609 carotid endarterectomies. Tex Heart Inst J. 2008; 35:104–110.4. Ferguson GG, Eliasziw M, Barr HW, Clagett GP, Barnes RW, Wallace MC, et al. The North American Symptomatic Carotid Endarterectomy Trial: surgical results in 1415 patients. Stroke. 1999; 30:1751–1758.
Article5. Lovrencic-Huzjan A, Rundek T, Katsnelson M. Recommendations for management of patients with carotid stenosis. Stroke Res Treat. 2012; 2012:175869.
Article6. Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. Stroke. 2011; 42:e420–e463.7. Shin S, Kwon TW, Cho YP, Shin JH, Yi A, Kim H, et al. Preoperative magnetic resonance angiography as a predictive test for cerebral ischemia during carotid endarterectomy. World J Surg. 2013; 37:663–670.
Article8. Kim JH, Cho YP, Kwon TW, Kim H, Kim GE. Ten-year comparative analysis of bovine pericardium and autogenous vein for patch angioplasty in patients undergoing carotid endarterectomy. Ann Vasc Surg. 2012; 26:353–358.
Article9. Dahl T, Aasland J, Romundstad P, Johnsen HJ, Myhre HO. Carotid endarterectomy: time-trends and results during a 20-year period. Int Angiol. 2006; 25:241–248.10. Cunningham EJ, Bond R, Mayberg MR, Warlow CP, Rothwell PM. Risk of persistent cranial nerve injury after carotid endarterectomy. J Neurosurg. 2004; 101:445–448.
Article11. Ballotta E, Da Giau G, Renon L, Narne S, Saladini M, Abbruzzese E, et al. Cranial and cervical nerve injuries after carotid endarterectomy: a prospective study. Surgery. 1999; 125:85–91.
Article12. Barnett HJ, Meldrum HE, Eliasziw M. North American Symptomatic Carotid Endarterectomy Trial (NASCET) collaborators. The appropriate use of carotid endarterectomy. CMAJ. 2002; 166:1169–1179.13. Halm EA, Tuhrim S, Wang JJ, Rockman C, Riles TS, Chassin MR. Risk factors for perioperative death and stroke after carotid endarterectomy: results of the new york carotid artery surgery study. Stroke. 2009; 40:221–229.
Article14. Brinjikji W, Rabinstein AA, Meyer FB, Piepgras DG, Lanzino G. Risk of early carotid endarterectomy for symptomatic carotid stenosis. Stroke. 2010; 41:2186–2190.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Carotid Stenting a Reasonable Alternative to Carotid Endarterectomy?
- Microsurgical Endarterectomy for Symptomatic Carotid Artery Stenosis
- Carotid Endarterectomy in Bilateral Carotid Stenosis: Case Report
- Symptomatic Post Endarterectomy Common Carotid Artery Pseudoaneurysm Treated with Combination of Flow Diverter Implantation and Carotid Stenting
- Complication of Carotid Endarterectomy