J Clin Neurol.
2017 Jan;13(1):84-90. 10.3988/jcn.2017.13.1.84.
Human Umbilical Cord Blood CD34-Positive Cells as Predictors of the Incidence and Short-Term Outcome of Neonatal Hypoxic-Ischemic Encephalopathy: A Pilot Study
- Affiliations
-
- 1Department of Pediatrics, Faculty of Medicine, Ain Shams University, Cairo, Egypt. saharhassanein@med.asu.edu.eg
- 2Department of Obstetrics and Gynecology, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
- 3Department of Clinical Pathology, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
- 4Neonatal Unit, the Queen Elizabeth Hospital, King's Lynn, UK.
- 5Department of Community Medicine, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
- 6MOH, Cairo, Egypt.
- KMID: 2364902
- DOI: http://doi.org/10.3988/jcn.2017.13.1.84
Abstract
- BACKGROUND AND PURPOSE
Neonatal hypoxic-ischemic encephalopathy (HIE) is one of the leading causes of neurological handicap in developing countries. Human umbilical cord blood (hUCB) CD34-positive (CD34âº) stem cells exhibit the potential for neural repair. We tested the hypothesis that hUCB CD34⺠stem cells and other cell types [leukocytes and nucleated red blood cells (NRBCs)] that are up-regulated during the acute stage of perinatal asphyxia (PA) could play a role in the early prediction of the occurrence, severity, and mortality of HIE.
METHODS
This case-control pilot study investigated consecutive neonates exposed to PA. The hUCB CD34⺠cell count in mononuclear layers was assayed using a flow cytometer. Twenty full-term neonates with PA and 25 healthy neonates were enrolled in the study.
RESULTS
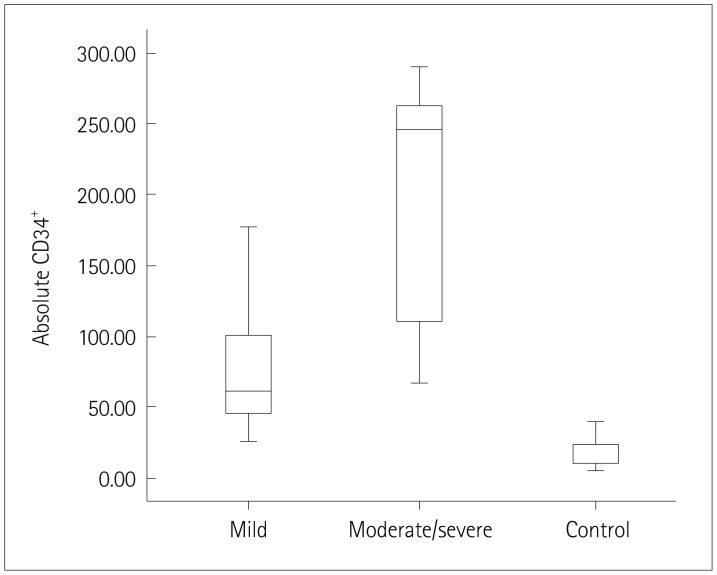
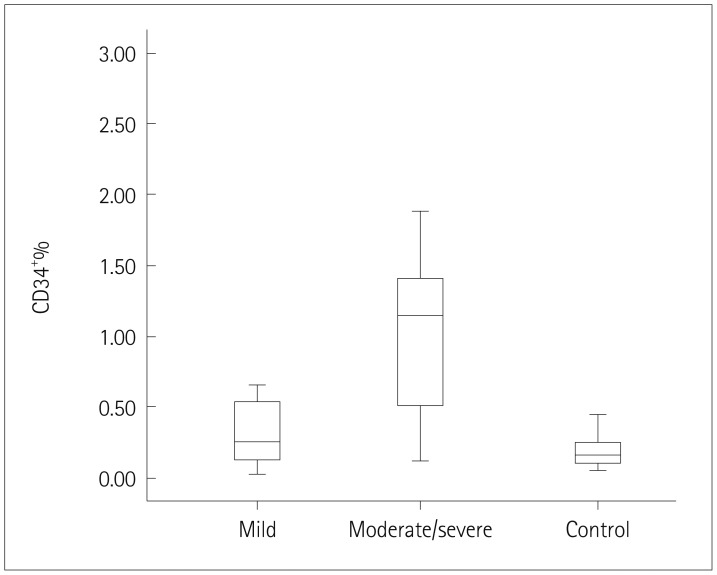
The absolute CD34⺠cell count (p=0.02) and the relative CD34⺠cell count (CD34+%) (p<0.001) in hUCB were higher in the HIE patients (n=20) than the healthy controls. The hUCB absolute CD34⺠cell count (p=0.04), CD34âº% (p<0.01), and Hobel risk scores (p=0.04) were higher in patients with moderate-to-severe HIE (n=9) than in those with mild HIE (n=11). The absolute CD34⺠cell count was strongly correlated with CD34âº% (p<0.001), Hobel risk score (p=0.04), total leukocyte count (TLC) (p<0.001), and NRBC count (p=0.01). CD34+% was correlated with TLC (p=0.02).
CONCLUSIONS
hUCB CD34⺠cells can be used to predict the occurrence, severity, and mortality of neonatal HIE after PA.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee AC, Kozuki N, Blencowe H, Vos T, Bahalim A, Darmstadt GL, et al. Intrapartum-related neonatal encephalopathy incidence and impairment at regional and global levels for 2010 with trends from 1990. Pediatr Res. 2013; 74(Suppl 1):50–72. PMID: 24366463.
Article2. Itoo BA, Al-Hawsawi ZM, Khan AH. Hypoxic ischemic encephalopathy, Incidence and risk factors in North Western Saudi Arabia. Neurosciences (Riyadh). 2003; 8:113–119. PMID: 23649029.3. Dixon BJ, Reis C, Ho WM, Tang J, Zhang JH. Neuroprotective strategies after neonatal hypoxic ischemic encephalopathy. Int J Mol Sci. 2015; 16:22368–22401. PMID: 26389893.4. El Shimi MS, Awad HA, Hassanein SM, Gad GI, Imam SS, Shaaban HA, et al. Single dose recombinant erythropoietin versus moderate hypothermia for neonatal hypoxic ischemic encephalopathy in low resource settings. J Matern Fetal Neonatal Med. 2014; 27:1295–1300. PMID: 24134405.
Article5. Serpero LD, Bellissima V, Colivicchi M, Sabatini M, Frigiola A, Ricotti A, et al. Next generation biomarkers for brain injury. J Matern Fetal Neonatal Med. 2013; 26(Suppl 2):44–49.
Article6. Hassanein SM, Deifalla SM, El-Houssinie M, Mokbel SA. Safety and efficacy of cerebrolysin in infants with communication defects due to severe perinatal brain insult: a randomized controlled clinical trial. J Clin Neurol. 2016; 12:79–84. PMID: 26365023.
Article7. Chalak LF, DuPont TL, Sánchez PJ, Lucke A, Heyne RJ, Morriss MC, et al. Neurodevelopmental outcomes after hypothermia therapy in the era of Bayley-III. J Perinatol. 2014; 34:629–633. PMID: 24743133.
Article8. Horn AR, Swingler GH, Myer L, Linley LL, Raban MS, Joolay Y, et al. Early clinical signs in neonates with hypoxic ischemic encephalopathy predict an abnormal amplitude-integrated electroencephalogram at age 6 hours. BMC Pediatr. 2013; 13:52. PMID: 23574923.
Article9. Hayakawa M, Ito Y, Saito S, Mitsuda N, Hosono S, Yoda H, et al. Incidence and prediction of outcome in hypoxic-ischemic encephalopathy in Japan. Pediatr Int. 2014; 56:215–221. PMID: 24127879.10. Menticoglou SM. How often do perinatal events at full term cause cerebral palsy? J Obstet Gynaecol Can. 2008; 30:396–403. PMID: 18505663.
Article11. Bhongir AV, Yakama AV, Saha S, Radia SB, Pabbati J. The urinary uric acid/creatinine ratio is an adjuvant marker for perinatal asphyxia. Eur J Pharm Med Res. 2015; 2:520–528. PMID: 26998526.12. Goel M, Dwivedi R, Gohiya P, Hegde D. Nucleated red blood cell in cord blood as a marker of perinatal asphyxia. J Clin Neonatol. 2013; 2:179–182. PMID: 24404530.
Article13. Aly H, Hassanein S, Nada A, Mohamed MH, Atef SH, Atiea W. Vascular endothelial growth factor in neonates with perinatal asphyxia. Brain Dev. 2009; 31:600–604. PMID: 18926648.
Article14. Reali C, Scintu F, Pillai R, Cabras S, Argiolu F, Ristaldi MS, et al. Differentiation of human adult CD34+ stem cells into cells with a neural phenotype: role of astrocytes. Exp Neurol. 2006; 197:399–406. PMID: 16298364.15. Hobel CJ, Youkeles L, Forsythe A. Prenatal and intrapartum high-risk screening. II. Risk factors reassessed. Am J Obstet Gynecol. 1979; 135:1051–1056. PMID: 517589.16. Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976; 33:696–705. PMID: 987769.17. Thompson CM, Puterman AS, Linley LL, Hann FM, van der Elst CW, Molteno CD, et al. The value of a scoring system for hypoxic ischaemic encephalopathy in predicting neurodevelopmental outcome. Acta Paediatr. 1997; 86:757–761. PMID: 9240886.
Article18. Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005; 353:1574–1584. PMID: 16221780.
Article19. Denning-Kendall PA, Horsley H, Donaldson C, Bradley B, Hows JM. Different behaviour of fresh and cultured CD34+ cells during immunomagnetic separation. Br J Haematol. 1999; 105:780–785. PMID: 10354147.20. van Laerhoven H, de Haan TR, Offringa M, Post B, van der Lee JH. Prognostic tests in term neonates with hypoxic-ischemic encephalopathy: a systematic review. Pediatrics. 2013; 131:88–98. PMID: 23248219.
Article21. Surbek DV, Aufderhaar U, Holzgreve W. Umbilical cord blood collection for transplantation: which technique should be preferred? Am J Obstet Gynecol. 2000; 183:1587–1588. PMID: 11120533.
Article22. Axt R, Ertan K, Hendrik J, Wrobel M, Mink D, Schmidt W. Nucleated red blood cells in cord blood of singleton term and post-term neonates. J Perinat Med. 1999; 27:376–381. PMID: 10642958.
Article23. Mehrishi JN, Bakács T. A novel method of CD34+ cell separation from umbilical cord blood. Transfusion. 2013; 53:2675–2680. PMID: 23432618.24. Sutherland DR, Anderson L, Keeney M, Nayar R, Chin-Yee I. The ISHAGE guidelines for CD34+ cell determination by flow cytometry. International Society of Hematotherapy and Graft Engineering. J Hematother. 1996; 5:213–226. PMID: 8817388.25. Sidney LE, Branch MJ, Dunphy SE, Dua HS, Hopkinson A. Concise review: evidence for CD34 as a common marker for diverse progenitors. Stem Cells. 2014; 32:1380–1389. PMID: 24497003.
Article26. Al-Deghaither SY. Impact of maternal and neonatal factors on parameters of hematopoietic potential in umbilical cord blood. Saudi Med J. 2015; 36:704–712. PMID: 25987113.
Article27. Kim JP, Lee YH, Lee YA, Kim YD. A comparison of the kinetics of nucleated cells and CD34+ cells in neonatal peripheral blood and cord blood. Biol Blood Marrow Transplant. 2007; 13:478–485. PMID: 17382254.28. Liang CC, Liu HL, Chang SD, Chen SH, Lee TH. The protective effect of human umbilical cord blood CD34+ cells and estradiol against focal cerebral ischemia in female ovariectomized rat: cerebral MR imaging and immunohistochemical study. PLoS One. 2016; 11:e0147133. PMID: 26760774.
Article29. Tsuji M, Taguchi A, Ohshima M, Kasahara Y, Sato Y, Tsuda H, et al. Effects of intravenous administration of umbilical cord blood CD34(+) cells in a mouse model of neonatal stroke. Neuroscience. 2014; 263:148–158. PMID: 24444827.
Article30. Boltze J, Reich DM, Hau S, Reymann KG, Strassburger M, Lobsien D, et al. Assessment of neuroprotective effects of human umbilical cord blood mononuclear cell subpopulations in vitro and in vivo. Cell Transplant. 2012; 21:723–737. PMID: 21929866.
Article31. Haase VH. Regulation of erythropoiesis by hypoxia-inducible factors. Blood Rev. 2013; 27:41–53. PMID: 23291219.
Article32. Elbuken G, Tanriverdi F, Karaca Z, Eser B, Hasdiraz L, Unluhizarci K, et al. Evaluation of peripheral blood CD34+ cell count in the acute phase of traumatic brain injury and chest trauma. Brain Inj. 2016; 30:179–183. PMID: 26649467.33. Cotten CM, Murtha AP, Goldberg RN, Grotegut CA, Smith PB, Goldstein RF, et al. Feasibility of autologous cord blood cells for infants with hypoxic-ischemic encephalopathy. J Pediatr. 2014; 164:973–979.e1. PMID: 24388332.
Article34. Aly H, Mohsen L, Badrawi N, Gabr H, Ali Z, Akmal D. Viability and neural differentiation of mesenchymal stem cells derived from the umbilical cord following perinatal asphyxia. J Perinatol. 2012; 32:671–676. PMID: 22134676.
Article35. Baburamani AA, Ek CJ, Walker DW, Castillo-Melendez M. Vulnerability of the developing brain to hypoxic-ischemic damage: contribution of the cerebral vasculature to injury and repair? Front Physiol. 2012; 3:424. PMID: 23162470.
Article36. Fan J, Cai H, Tan WS. Role of the plasma membrane ROS-generating NADPH oxidase in CD34+ progenitor cells preservation by hypoxia. J Biotechnol. 2007; 130:455–462. PMID: 17610977.37. Dong W, Yuwen Z, Xiaohui G. The enhanced ability of peripheral mononuclear cells differentiating into neural cells in term infants with good improvement suffering from severe hypoxic ischemic encephalopathy. Iran J Pediatr. 2014; 24:435–440. PMID: 25755867.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In Vitro Culture of Mast Cells from Human Umbilical Cord Blood Cells
- Maternal and Neonatal Predictors of Hematopoietic Potential of Umbilical Cord Blood Units
- Predictors of neurologic handicap in hypoxic ischemic encephalopathy
- The Correlation between CD34+ Cell and Nucleated RBC Counts in Human Cord Blood
- Cord blood-derived CD34(+) cells promotes functional recovery in transient middle cerebral artery occlusion model of rat