J Korean Med Sci.
2017 Feb;32(2):287-295. 10.3346/jkms.2017.32.2.287.
Characteristics of Adenovirus Pneumonia in Korean Military Personnel, 2012–2016
- Affiliations
-
- 1Department of Emergency Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. byungwoo.jhun@gmail.com
- 3Division of Pulmonary and Critical Care Medicine, Department of Medicine, The Armed Forces Capital Hospital, Seongnam, Korea.
- 4Department of Public Health and Operation, The Armed Forces Medical Command, Seongnam, Korea.
- KMID: 2364173
- DOI: http://doi.org/10.3346/jkms.2017.32.2.287
Abstract
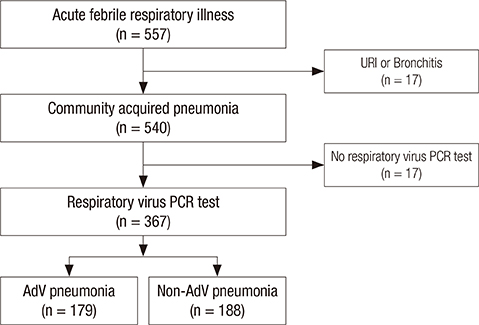
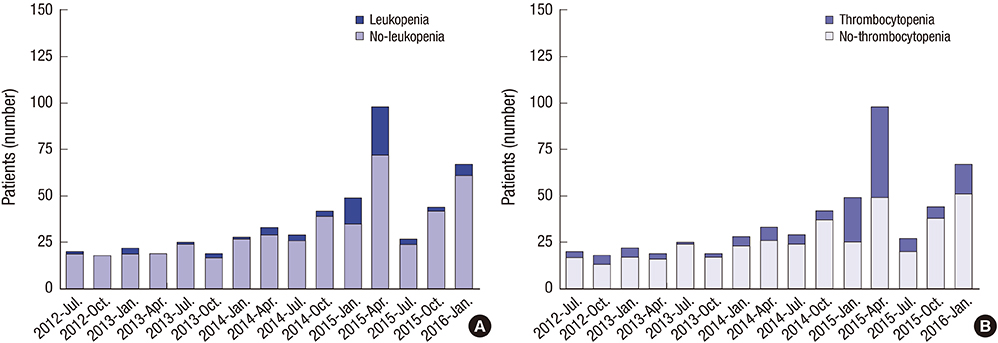
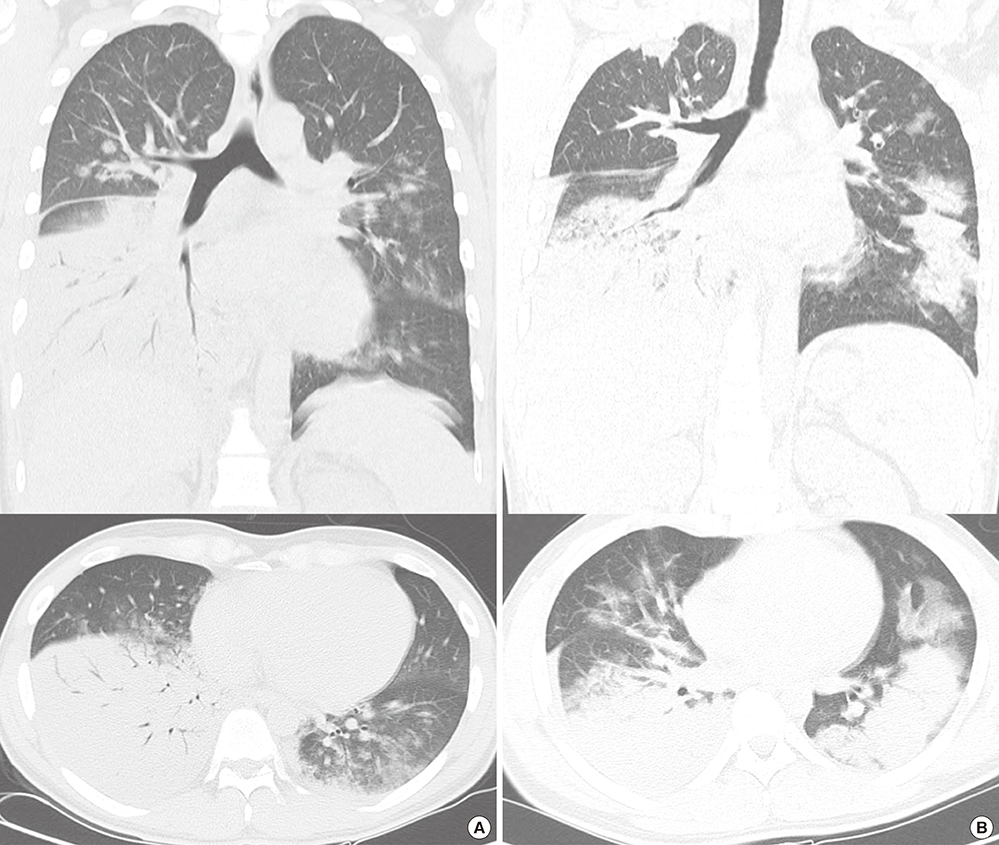
- Adenovirus (AdV) can cause severe pneumonia in non-immunocompromised host, but limited data exist on the distinctive characteristics of AdV pneumonia in non-immunocompromised patients. We evaluated distinctive clinico-laboratory and radiological characteristics and outcomes of AdV pneumonia (n = 179), compared with non-AdV pneumonia (n = 188) in Korean military personnel between 2012 and 2016. AdV pneumonia patients had a higher rate of consolidation with ground-glass opacity (101/152) in lobar distribution (89/152) on computed tomography (CT) (P < 0.001). Laboratory findings showed a higher incidence of unusual blood profiles such as leukopenia (55/179, P < 0.001) or thrombocytopenia (100/179, P < 0.001). The patients had more systemic symptoms such as myalgia (82/179, P = 0.001) or diarrhea (23/179, P < 0.001), compared with non-AdV pneumonia patients. Bacterial co-infection was identified in 28.5% of AdV pneumonia. Most of the AdV isolates typed (69/72, 95.8%) were AdV-55. Patients with a pneumonia severity index ≥ class III were more commonly observed in AdV pneumonia patients compared with non-AdV pneumonia patients (11.2% vs. 2.1%, P < 0.001), and time to clinical stabilization from admission was longer in the AdV pneumonia patients compared with the non-AdV pneumonia patients (3.8 vs. 2.6 days, P < 0.001). Mechanical ventilation (n = 6) was only required in AdV pneumonia patients, one of whom died due to AdV-55. Our data showed that AdV pneumonia in non-immunocompromised patients had distinct characteristics and most of the isolates typed in our study were AdV-55. It is suggested that AdV-55 is an important pathogen of pneumonia in Korean military personnel.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Epidemiological Investigation of the Outbreak of Acute Respiratory Infection caused by Adenovirus Type B55 in a Physical Education School in 2017
Jeongsuk Song, Hyerim Lee, Enhi Cho
Infect Chemother. 2019;51(2):119-129. doi: 10.3947/ic.2019.51.2.119.
Reference
-
1. Lynch JP 3rd, Fishbein M, Echavarria M. Adenovirus. Semin Respir Crit Care Med. 2011; 32:494–511.2. Simsir A, Greenebaum E, Nuovo G, Schulman LL. Late fatal adenovirus pneumonitis in a lung transplant recipient. Transplantation. 1998; 65:592–594.3. Doan ML, Mallory GB, Kaplan SL, Dishop MK, Schecter MG, McKenzie ED, Heinle JS, Elidemir O. Treatment of adenovirus pneumonia with cidofovir in pediatric lung transplant recipients. J Heart Lung Transplant. 2007; 26:883–889.4. Mayeur N, Srairi M, Tetu L, Guilbeau Frugier C, Fourcade O, Dahan M. Lethal hemorrhagic alveolitis after adenovirus pneumonia in a lung transplant recipient. Heart Lung. 2012; 41:401–403.5. Levin S, Dietrich J, Guillory J. Fatal nonbacterial pneumonia associated with adenovirus type 4. Occurrence in an adult. JAMA. 1967; 201:975–977.6. Tate JE, Bunning ML, Lott L, Lu X, Su J, Metzgar D, Brosch L, Panozzo CA, Marconi VC, Faix DJ, et al. Outbreak of severe respiratory disease associated with emergent human adenovirus serotype 14 at a US air force training facility in 2007. J Infect Dis. 2009; 199:1419–1426.7. Klinger JR, Sanchez MP, Curtin LA, Durkin M, Matyas B. Multiple cases of life-threatening adenovirus pneumonia in a mental health care center. Am J Respir Crit Care Med. 1998; 157:645–649.8. Ryu JS, Cho JH, Han HS, Jung MH, Yoon YH, Song ES, Lee JY, Kim SY, Lee KW, Kwak SM, et al. Acute respiratory distress syndrome induced by adenovirus in an otherwise healthy woman. Yonsei Med J. 2003; 44:732–735.9. Chen WW, Nie WM, Xu W, Xie YX, Tu B, Zhao P, Qin EQ, Zhang YH, Zhang X, Li WG, et al. Cross-sectional study of the relationship of peripheral blood cell profiles with severity of infection by adenovirus type 55. BMC Infect Dis. 2014; 14:147.10. Lewis PF, Schmidt MA, Lu X, Erdman DD, Campbell M, Thomas A, Cieslak PR, Grenz LD, Tsaknardis L, Gleaves C, et al. A community-based outbreak of severe respiratory illness caused by human adenovirus serotype 14. J Infect Dis. 2009; 199:1427–1434.11. Gu L, Liu Z, Li X, Qu J, Guan W, Liu Y, Song S, Yu X, Cao B. Severe community-acquired pneumonia caused by adenovirus type 11 in immunocompetent adults in Beijing. J Clin Virol. 2012; 54:295–301.12. Cao B, Huang GH, Pu ZH, Qu JX, Yu XM, Zhu Z, Dong JP, Gao Y, Zhang YX, Li XH, et al. Emergence of community-acquired adenovirus type 55 as a cause of community-onset pneumonia. Chest. 2014; 145:79–86.13. Sun B, He H, Wang Z, Qu J, Li X, Ban C, Wan J, Cao B, Tong Z, Wang C. Emergent severe acute respiratory distress syndrome caused by adenovirus type 55 in immunocompetent adults in 2013: a prospective observational study. Crit Care. 2014; 18:456.14. Scott MK, Chommanard C, Lu X, Appelgate D, Grenz L, Schneider E, Gerber SI, Erdman DD, Thomas A. Human adenovirus associated with severe respiratory infection, Oregon, USA, 2013-2014. Emerg Infect Dis. 2016; 22:1044–1051.15. Heo JY, Lee JE, Kim HK, Choe KW. Acute lower respiratory tract infections in soldiers, South Korea, April 2011-March 2012. Emerg Infect Dis. 2014; 20:875–877.16. Kim SJ, Kim K, Park SB, Hong DJ, Jhun BW. Outcomes of early administration of cidofovir in non-immunocompromised patients with severe adenovirus pneumonia. PLoS One. 2015; 10:e0122642.17. Yoon H, Jhun BW, Kim SJ, Kim K. Clinical characteristics and factors predicting respiratory failure in adenovirus pneumonia. Respirology. 2016; 21:1243–1250.18. Halm EA, Fine MJ, Marrie TJ, Coley CM, Kapoor WN, Obrosky DS, Singer DE. Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA. 1998; 279:1452–1457.19. Barker JH, Luby JP, Sean Dalley A, Bartek WM, Burns DK, Erdman DD. Fatal type 3 adenoviral pneumonia in immunocompetent adult identical twins. Clin Infect Dis. 2003; 37:e142–6.20. Hakim FA, Tleyjeh IM. Severe adenovirus pneumonia in immunocompetent adults: a case report and review of the literature. Eur J Clin Microbiol Infect Dis. 2008; 27:153–158.21. Miller WT Jr, Mickus TJ, Barbosa E Jr, Mullin C, Van Deerlin VM, Shiley KT. CT of viral lower respiratory tract infections in adults: comparison among viral organisms and between viral and bacterial infections. AJR Am J Roentgenol. 2011; 197:1088–1095.22. Falsey AR, Becker KL, Swinburne AJ, Nylen ES, Formica MA, Hennessey PA, Criddle MM, Peterson DR, Baran A, Walsh EE. Bacterial complications of respiratory tract viral illness: a comprehensive evaluation. J Infect Dis. 2013; 208:432–441.23. Cillóniz C, Ewig S, Menéndez R, Ferrer M, Polverino E, Reyes S, Gabarrús A, Marcos MA, Cordoba J, Mensa J, et al. Bacterial co-infection with H1N1 infection in patients admitted with community acquired pneumonia. J Infect. 2012; 65:223–230.24. Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008; 198:962–970.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe Adenovirus Pneumonia
- A Clinical features of Severe Adenovirus Pneumonia among Members of the Korea Military: A Case Series
- Pneumonia Caused by Adenovirus Genotype 55 in an Army Recruit Training Center
- Qualitative Analysis of the Tetanus Antibody in Korean Army personnel after Visiting a Tertiary Armed Forces Hospital
- Depressive Symptoms and Mental Health of Military Social Service Personnel