J Korean Med Sci.
2017 Feb;32(2):278-286. 10.3346/jkms.2017.32.2.278.
From Visiting a Physician to Expecting Antibiotics: Korean Perspectives and Practices toward Respiratory Tract Infections
- Affiliations
-
- 1Department of Preventive Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. kimcb@yonsei.ac.kr
- 2Institute for Poverty Alleviation and International Development, Yonsei University, Wonju, Korea.
- 3Department of Biostatistics, School of Public Health, Iran University of Medical Sciences, Tehran, Iran.
- 4Institute of Occupation and Environmental Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 5Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2364172
- DOI: http://doi.org/10.3346/jkms.2017.32.2.278
Abstract
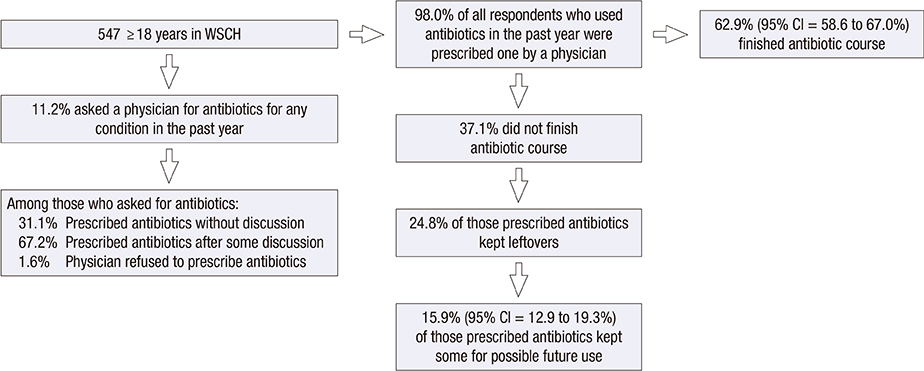
- Antibiotic resistance is steadily rising worldwide. Respiratory tract infections (RTIs) are common indications, mostly imprudent, for antibiotic prescriptions in outpatient setting. In Korea, antibiotic prescription rate for RTIs is still high. As physician visit and antibiotic prescribing are influenced by patient's perceptions and beliefs, we aimed to explore the general public's perspectives and practices toward RTIs and to develop the "˜RTI clinical iceberg.' A cross-sectional survey was conducted in Wonju Severance Christian Hospital (WSCH) among 550 adults attending outpatient departments during January 2016. Differences in distributions between groups were examined using two-tailed Pearson χ² test. Using the Andersen's behavioral model as a conceptual framework, we constructed logistic regression models to assess factors associated with physician visit. Of 547 participants with complete questionnaires, 62.9% reported having experienced an RTI in the previous six months; 59.3% visited a physician for the illness, most commonly because the symptoms were severe or prolonged, and approximately 16% of them expected an antibiotic prescription from the visit. Perceptions of symptoms severity, the need factor, most strongly influenced physician visit. Predisposing and enabling factors such as inappropriate expectations for antibiotic for a sore throat or having national health insurance also influenced physician visit. Almost all participants who reported asking for an antibiotic were prescribed one, with a 37.1% non-adherence rate. Conclusively, public education on self-care for RTI symptoms that addresses their main concerns may reduce physician visits. Improving physician-patient relationship and informing patients about the lack of antibiotic benefit for most RTIs may also reduce antibiotic prescriptions.
Keyword
MeSH Terms
Figure
Reference
-
1. Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, Vlieghe E, Hara GL, Gould IM, Goossens H, et al. Antibiotic resistance-the need for global solutions. Lancet Infect Dis. 2013; 13:1057–1098.2. World Health Organization. The evolving threat of antimicrobial resistance: options for action [Internet]. accessed on 26 May 2016. Available at http://apps.who.int/iris/bitstream/10665/44812/1/9789241503181_eng.pdf.3. Butler CC, Dunstan F, Heginbothom M, Mason B, Roberts Z, Hillier S, Howe R, Palmer S, Howard A. Containing antibiotic resistance: decreased antibiotic-resistant coliform urinary tract infections with reduction in antibiotic prescribing by general practices. Br J Gen Pract. 2007; 57:785–792.4. Monto AS. Epidemiology of viral respiratory infections. Am J Med. 2002; 112:Suppl 6A. 4S–12S.5. Arroll B. Antibiotics for upper respiratory tract infections: an overview of Cochrane reviews. Respir Med. 2005; 99:255–261.6. Smith SM, Fahey T, Smucny J, Becker LA. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2014; CD000245.7. Earnshaw S, Mancarella G, Mendez A, Todorova B, Magiorakos AP, Possenti E, Stryk M, Gilbro S, Goossens H, Albiger B, et al. European antibiotic awareness day: a five-year perspective of Europe-wide actions to promote prudent use of antibiotics. Euro Surveill. 2014; 19:20928.8. Kim B, Kim J, Kim SW, Pai H. A Survey of antimicrobial stewardship programs in Korea, 2015. J Korean Med Sci. 2016; 31:1553–1559.9. Lee K, Yong D, Jeong SH, Chong Y. Multidrug-resistant Acinetobacter spp.: increasingly problematic nosocomial pathogens. Yonsei Med J. 2011; 52:879–891.10. Song JH, Joo EJ. The crisis of antimicrobial resistance: current status and future strategies. J Korean Med Assoc. 2010; 53:999–1005.11. Kwon K, Hwang IG, Kwak HS, Park JS, Kim MG, Lee G. Administration of National Antimicrobial Resistance Experts and Public Campaign Activities. Seoul: Korea Food & Drug Administration;2006.12. Yun JM, Shin DW, Hwang SS, Cho J, Nam YS, Kim JH, Cho BL. Effect of public disclosure on antibiotic prescription rate for upper respiratory tract infections. JAMA Intern Med. 2015; 175:445–447.13. Chung DR, Song JH; The Korean Society of Infectious Diseases. National campaign for appropriate antibiotic use in Korea. Infect Chemother. 2012; 44:164–167.14. Kim BN. Overview of antibiotic use in Korea. Infect Chemother. 2012; 44:250–262.15. Yoon YK, Park GC, An H, Chun BC, Sohn JW, Kim MJ. Trends of antibiotic consumption in Korea according to national reimbursement data (2008–2012): a population-based epidemiologic study. Medicine (Baltimore). 2015; 94:e2100.16. Kim SS, Moon S, Kim EJ. Public knowledge and attitudes regarding antibiotic use in South Korea. J Korean Acad Nurs. 2011; 41:742–749.17. Agency for Healthcare Research and Quality (US). Improving antibiotic prescribing for uncomplicated acute respiratory tract infections [Internet]. Accessed 10 May 2016. Available at https://www.effectivehealthcare.ahrq.gov/ehc/products/561/2112/antibiotics-respiratory-infection-report-160128.pdf.18. Kim JS, Park HN, Cho EM, Park WM, Lee SH, Lee HS, Lee SH. Patient knowledge of upper respiratory infections an unnecessary utilization of antibiotics. J Korean Acad Fam Med. 2001; 22:200–211.19. Coxeter P, Del Mar CB, McGregor L, Beller EM, Hoffmann TC. Interventions to facilitate shared decision making to address antibiotic use for acute respiratory infections in primary care. Cochrane Database Syst Rev. 2015; CD010907.20. McNulty CA, Nichols T, French DP, Joshi P, Butler CC. Expectations for consultations and antibiotics for respiratory tract infection in primary care: the RTI clinical iceberg. Br J Gen Pract. 2013; 63:e429–36.21. Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005; 83:1–24.22. Health Insurance Review & Assessment Service (KR). Comprehensive Quality Report of National Health Insurance 2012. Seoul: Health Insurance Review & Assessment Service;2013.23. Wun YT, Lam TP, Lam KF, Ho PL, Yung WH. The public’s perspectives on antibiotic resistance and abuse among Chinese in Hong Kong. Pharmacoepidemiol Drug Saf. 2013; 22:241–249.24. Korea Centers for Disease Control and Prevention. Community Health Survey 2008-2014: Community Health Statistics at a Glance. Cheongju: Korea Centers for Disease Control and Prevention;2015.25. Dean AG, Arner TG, Sunki GG, Friedman R, Lantinga M, Sangam S, Zubieta JC, Sullivan KM, Brendel KA, Gao Z, et al. Epi Info™, a Database and Statistics Program for Public Health Professionals. Atlanta, GA: Centers for Disease Control and Prevention;2011.26. IBM Corp. (US). IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.;2011.27. Renati S, Linder JA. Necessity of office visits for acute respiratory infections in primary care. Fam Pract. 2016; 33:312–317.28. Lee JY, Jo MW, Yoo WS, Kim HJ, Eun SJ. Evidence of a broken healthcare delivery system in Korea: unnecessary hospital outpatient utilization among patients with a single chronic disease without complications. J Korean Med Sci. 2014; 29:1590–1596.29. van Duijn HJ, Kuyvenhoven MM, Schellevis FG, Verheij TJ. Illness behaviour and antibiotic prescription in patients with respiratory tract symptoms. Br J Gen Pract. 2007; 57:561–568.30. Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmonth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ. 1997; 315:350–352.31. Suh HS, Kang HY, Kim J, Shin E. Effect of health insurance type on health care utilization in patients with hypertension: a national health insurance database study in Korea. BMC Health Serv Res. 2014; 14:570–581.32. Hordijk PM, Broekhuizen BD, Butler CC, Coenen S, Godycki-Cwirko M, Goossens H, Hood K, Smith R, van Vugt SF, Little P, et al. Illness perception and related behaviour in lower respiratory tract infections—a European study. Fam Pract. 2015; 32:152–158.33. van Driel ML, De Sutter A, Deveugele M, Peersman W, Butler CC, De Meyere M, De Maeseneer J, Christiaens T. Are sore throat patients who hope for antibiotics actually asking for pain relief? Ann Fam Med. 2006; 4:494–499.34. Andrews T, Thompson M, Buckley DI, Heneghan C, Deyo R, Redmond N, Lucas PJ, Blair PS, Hay AD. Interventions to influence consulting and antibiotic use for acute respiratory tract infections in children: a systematic review and meta-analysis. PLoS One. 2012; 7:e30334.35. Jang SN, Kim NS. Understanding the culture of antibiotics prescribing of primary physicians for acute upper respiratory infection. J Korean Acad Fam Med. 2004; 25:901–907.36. Cho HJ, Hong SJ, Park S. Knowledge and beliefs of primary care physicians, pharmacists, and parents on antibiotic use for the pediatric common cold. Soc Sci Med. 2004; 58:623–629.37. McCullough AR, Glasziou PP. Delayed antibiotic prescribing strategies--time to implement? JAMA Intern Med. 2016; 176:29–30.38. Butler CC, Kelly MJ, Hood K, Schaberg T, Melbye H, Serra-Prat M, Blasi F, Little P, Verheij T, Mölstad S, et al. Antibiotic prescribing for discoloured sputum in acute cough/lower respiratory tract infection. Eur Respir J. 2011; 38:119–125.39. Kardas P, Devine S, Golembesky A, Roberts C. A systematic review and meta-analysis of misuse of antibiotic therapies in the community. Int J Antimicrob Agents. 2005; 26:106–113.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Survey on Physician Attitude of Antibiotic Prescription for Upper Respiratory Tract Infections
- Factors Influencing Antibiotics Prescribing of Primary Health Physicians in Acute Upper Respiratory Infections
- Prevalence of Antibiotic Use for Pediatric Acute Upper Respiratory Tract Infections in Korea
- Recovery of respiratory syncytial virus, adenovirus, influenza virus , and parainfluenza virus from nasopharyngeal aspirates from children with acute respiratory tract infections
- Clinical evaluation of cefodizime in lower respiratory tract infections