Trends in Survival and Incidence of Bronchopulmonary Dysplasia in Extremely Preterm Infants at 23-26 Weeks Gestation
- Affiliations
-
- 1Department of Pediatrics, Chonbuk National University School of Medicine, Jeonju, Korea.
- 2Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea.
- 3Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wonspark@skku.edu
- KMID: 2363504
- DOI: http://doi.org/10.3346/jkms.2016.31.3.423
Abstract
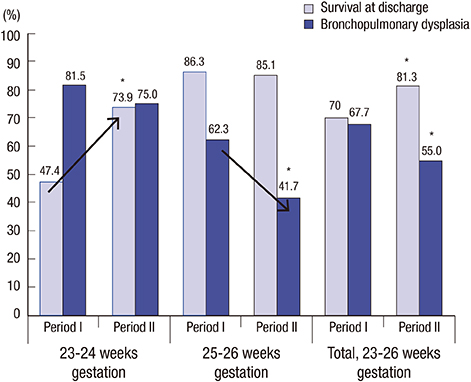
- The aim of this study was to investigate the relationship between survival and incidence of bronchopulmonary dysplasia (BPD) in extremely premature infants, and identify clinical factors responsible for this association. Medical records of 350 infants at 23-26 weeks gestation from 2000 to 2005 (period I, n = 137) and 2006 to 2010 (period II, n = 213) were retrospectively reviewed. The infants were stratified into 23-24 and 25-26 weeks gestation, and the survival, BPD incidence, and clinical characteristics were analyzed. BPD was defined as oxygen dependency at 36 weeks postmenstrual age. The overall survival rate was significantly improved in period II compared to period I (80.3% vs. 70.0%, respectively; P = 0.028), especially in infants at 23-24 weeks gestation (73.9% vs. 47.4%, respectively; P = 0.001). The BPD incidence in survivors during period II (55.0%) was significantly decreased compared to period I (67.7%; P = 0.042), especially at 25-26 weeks gestation (41.7% vs. 62.3%, respectively; P = 0.008). Significantly improved survival at 23-24 weeks gestation was associated with a higher antenatal steroid use and an improved 5-minute Apgar score. A significant decrease in BPD incidence at 25-26 weeks gestation was associated with early extubation, prolonged use of less invasive continuous positive airway pressure, and reduced supplemental oxygen. Improved perinatal and neonatal care can simultaneously lead to improved survival and decreased BPD incidence in extremely premature infants.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
The Impact of Surgical Intervention on Neurodevelopmental Outcomes in Very Low Birth Weight Infants: a Nationwide Cohort Study in Korea
Se In Sung, Na Hyun Lee, Hyun Ho Kim, Hye Seon Kim, Yea Seul Han, Misun Yang, So Yoon Ahn, Yun Sil Chang, Won Soon Park
J Korean Med Sci. 2019;34(43):. doi: 10.3346/jkms.2019.34.e271.Neonatal Outcomes of Very Low Birth Weight Infants in Korean Neonatal Network from 2013 to 2016
Jang Hoon Lee, O Kyu Noh, Yun Sil Chang,
J Korean Med Sci. 2019;34(5):. doi: 10.3346/jkms.2019.34.e40.Clinical characteristics of lower respiratory infections in preterm children with bronchopulmonary dysplasia
Na Hyun Lee, Se Jin Kim, Hee Joung Choi
Allergy Asthma Respir Dis. 2017;5(2):92-98. doi: 10.4168/aard.2017.5.2.92.Continuous Renal Replacement Therapy in Preterm Infants
Eu Seon Noh, Hyun Ho Kim, Hye Seon Kim, Yea Seul Han, Misun Yang, So Yoon Ahn, Se In Sung, Yun Sil Chang, Won Soon Park
Yonsei Med J. 2019;60(10):984-991. doi: 10.3349/ymj.2019.60.10.984.
Reference
-
1. Botet F, Figueras-Aloy J, Miracle-Echegoyen X, Rodríguez-Miguélez JM, Salvia-Roiges MD, Carbonell-Estrany X. Trends in survival among extremely-low-birth-weight infants (less than 1000 g) without significant bronchopulmonary dysplasia. BMC Pediatr. 2012; 12:63–69.2. Coalson JJ. Pathology of new bronchopulmonary dysplasia. Semin Neonatol. 2003; 8:73–81.3. Geary C, Caskey M, Fonseca R, Malloy M. Decreased incidence of bronchopulmonary dysplasia after early management changes, including surfactant and nasal continuous positive airway pressure treatment at delivery, lowered oxygen saturation goals, and early amino acid administration: a historical cohort study. Pediatrics. 2008; 121:89–96.4. Eichenwald EC, Stark AR. Management and outcomes of very low birth weight. N Engl J Med. 2008; 358:1700–1711.5. Parker RA, Lindstrom DP, Cotton RB. Improved survival accounts for most, but not all, of the increase in bronchopulmonary dysplasia. Pediatrics. 1992; 90:663–668.6. Shah PS, Sankaran K, Aziz K, Allen AC, Seshia M, Ohlsson A, Lee SK, Lee SK, Shah PS, Andrews W, et al. Outcomes of preterm infants <29 weeks gestation over 10-year period in Canada: a cause for concern? J Perinatol. 2012; 32:132–138.7. Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, Bauer CR, Donovan EF, Korones SB, Laptook AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007; 196:147.e1–147.e8.8. Smith VC, Zupancic JA, McCormick MC, Croen LA, Greene J, Escobar GJ, Richardson DK. Trends in severe bronchopulmonary dysplasia rates between 1994 and 2002. J Pediatr. 2005; 146:469–473.9. Berger TM, Bachmann II, Adams M, Schubiger G. Impact of improved survival of very low-birth-weight infants on incidence and severity of bronchopulmonary dysplasia. Biol Neonate. 2004; 86:124–130.10. Herber-Jonat S, Schulze A, Kribs A, Roth B, Lindner W, Pohlandt F. Survival and major neonatal complications in infants born between 22 0/7 and 24 6/7 weeks of gestation (1999-2003). Am J Obstet Gynecol. 2006; 195:16–22.11. Park SE, Jeon GW, Choi CW, Hwang JH, Koo SH, Kim YJ, Lee CH, Chang YS, Park WS. Evaluation of perinatal and management factors associated with improved survival in extremely low birth weight infants. Korean J Pediatr. 2005; 48:1324–1329.12. Seri I, Evans J. Limits of viability: definition of the gray zone. J Perinatol. 2008; 28:Suppl 1. S4–S8.13. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010; 126:443–456.14. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–1729.15. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92:529–534.16. Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, Brotherton T. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978; 187:1–7.17. Garner A, Ben-Sira I, Deutman A, Fledelius H, Flynn J, Gole G, Hindle NW, Ideta H, Kinghan J, Koerner F, et al. An international classification of retinopathy of prematurity. Pediatrics. 1984; 74:127–133.18. Choi SH, Seo HJ, Yoo HS, Ahn SY, Chang YS, Park WS. Neonatal resuscitation at delivery room in “gray zone” extremely low birth-weight infants (gestational age ≤24 weeks). Korean J Perinatol. 2010; 21:155–164.19. Klinger G, Sokolover N, Boyko V, Sirota L, Lerner-Geva L, Reichman B. Israel Neonatal Network. Perinatal risk factors for bronchopulmonary dysplasia in a national cohort of very-low-birthweight infants. Am J Obstet Gynecol. 2013; 208:115.e1–115.e9.20. Trembath A, Laughon MM. Predictors of bronchopulmonary dysplasia. Clin Perinatol. 2012; 39:585–601.21. Smith PB, Ambalavanan N, Li L, Cotten CM, Laughon M, Walsh MC, Das A, Bell EF, Carlo WA, Stoll BJ, et al. Approach to infants born at 22 to 24 weeks' gestation: relationship to outcomes of more-mature infants. Pediatrics. 2012; 129:e1508–e1516.22. Hack M, Fanaroff AA. Outcomes of children of extremely low birthweight and gestational age in the 1990's. Early Hum Dev. 1999; 53:193–218.23. Jo HS, Cho KH, Cho SI, Song ES, Kim BI. Recent changes in the incidence of bronchopulmonary dysplasia among very low birth weight infants in Korea. J Korean Med Sci. 2015; 30:Suppl 1. S81–S87.24. Northway WH Jr, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967; 276:357–368.25. Keszler M. State of the art in conventional mechanical ventilation. J Perinatol. 2009; 29:262–275.26. Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A, Everette R, Peters N, Miller N, Muran G, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 2004; 114:1305–1311.27. Payne NR, LaCorte M, Karna P, Chen S, Finkelstein M, Goldsmith JP, Carpenter JH. Breathsavers Group, Vermont Oxford Network Neonatal Intensive Care Quality Improvement Collaborative. Reduction of bronchopulmonary dysplasia after participation in the Breathsavers Group of the Vermont Oxford Network Neonatal Intensive Care Quality Improvement Collaborative. Pediatrics. 2006; 118:Suppl 2. S73–S77.28. Payne NR, LaCorte M, Sun S, Karna P, Lewis-Hunstiger M, Goldsmith JP. Breathsavers Group. Evaluation and development of potentially better practices to reduce bronchopulmonary dysplasia in very low birth weight infants. Pediatrics. 2006; 118:Suppl 2. S65–S72.29. Choi CW, Kim BI, Kim EK, Song ES, Lee JJ. Incidence of bronchopulmonary dysplasia in Korea. J Korean Med Sci. 2012; 27:914–921.30. Sandri F, Plavka R, Ancora G, Simeoni U, Stranak Z, Martinelli S, Mosca F, Nona J, Thomson M, Verder H, et al. CURPAP Study Group. Prophylactic or early selective surfactant combined with nCPAP in very preterm infants. Pediatrics. 2010; 125:e1402–e1409.31. Kraybill EN, Runyan DK, Bose CL, Khan JH. Risk factors for chronic lung disease in infants with birth weights of 751 to 1000 grams. J Pediatr. 1989; 115:115–120.32. Korhonen P, Tammela O, Koivisto AM, Laippala P, Ikonen S. Frequency and risk factors in bronchopulmonary dysplasia in a cohort of very low birth weight infants. Early Hum Dev. 1999; 54:245–258.33. Stevens TP, Blennow M, Soll RF. Early surfactant administration with brief ventilation vs selective surfactant and continued mechanical ventilation for preterm infants with or at risk for RDS. Cochrane Database Syst Rev. 2002; CD003063.34. Doyle LW, Roberts G, Anderson PJ. Victorian Infant Collaborative Study Group. Changing long-term outcomes for infants 500-999 g birth weight in Victoria, 1979-2005. Arch Dis Child Fetal Neonatal Ed. 2011; 96:F443–F447.35. Wilson-Costello D. Is there evidence that long-term outcomes have improved with intensive care? Semin Fetal Neonatal Med. 2007; 12:344–354.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Survival and Cause of Death among Extremely Preterm Infants Near the Limit of Viability
- Prevention and Treatment of Bronchopulmonary Dysplasia
- Changes in the Incidence of Bronchopulmonary Dysplasia among Preterm Infants in a Single Center over 10 Years
- Association of Positive Ureaplasma in Gastric Fluid with Clinical Features in Preterm Infants
- Neonatal Outcomes according to the Latent Period from Membrane Rupture to Delivery among Extremely Preterm Infants Exposed to Preterm Premature Rupture of Membrane: a Nationwide Cohort Study