J Korean Assoc Pediatr Surg.
2016 Dec;22(2):59-62. 10.13029/jkaps.2016.22.2.59.
A Case of Pediatric Nodal Marginal Zone Lymphoma
- Affiliations
-
- 1Department of Pediatric Surgery, Seoul National University Children's Hospital, Seoul, Korea. spkhy02@snu.ac.kr
- KMID: 2363026
- DOI: http://doi.org/10.13029/jkaps.2016.22.2.59
Abstract
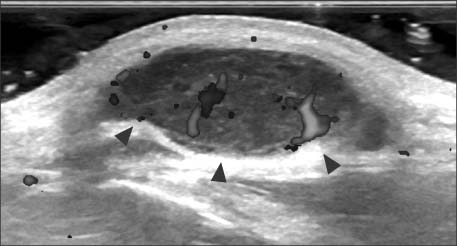
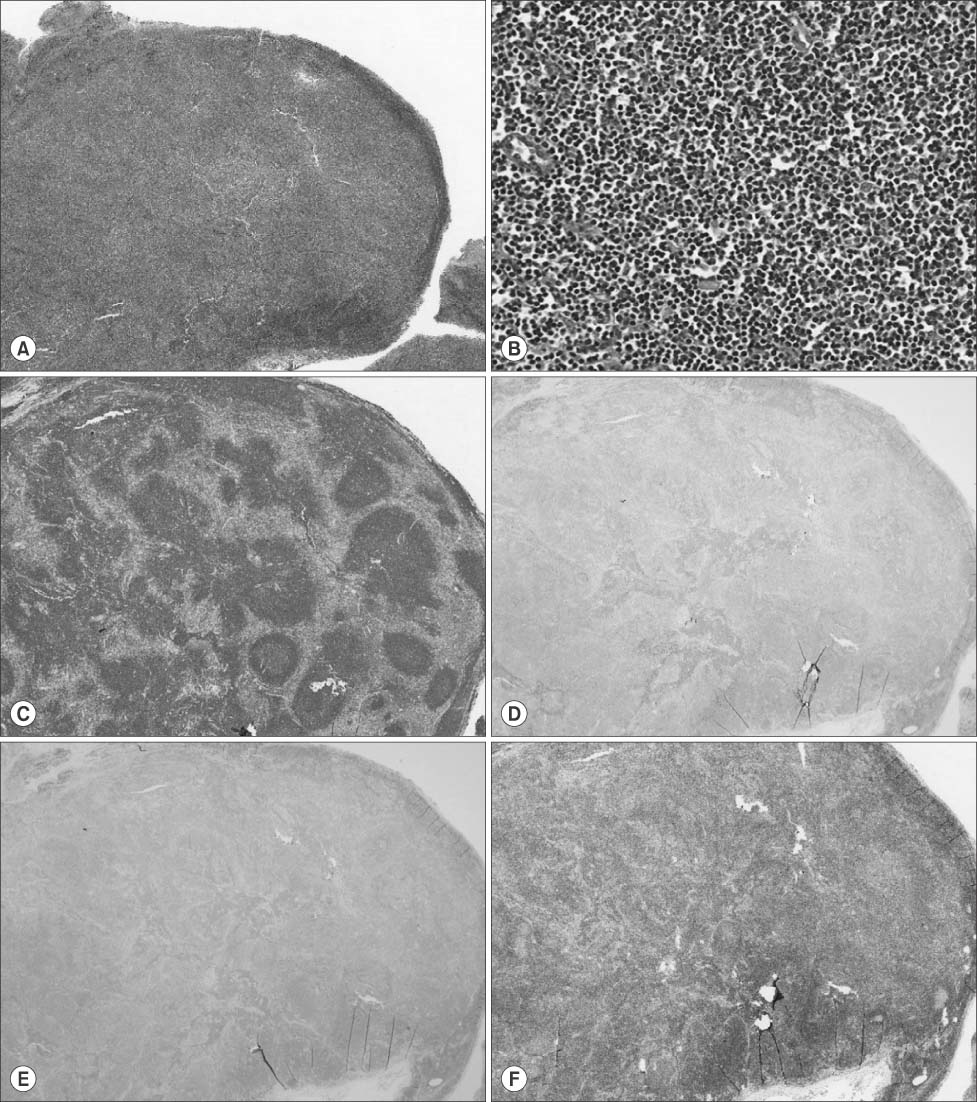
- Lymph node enlargement is a common finding in children suggesting normal or benign. Palpable nodes which are large, hard or fixed must be examined carefully to rule out malignant diseases. In this case, a 15-year-old boy presented to our hospital to inspect the palpable mass at his post-auricular area being found 2 months ago. It was diagnosed as nodal marginal zone lymphoma (NMZL) through excisional biopsy and immunohistochemistry. NMZL is very rare, especially in children and young adults, but occurs locally in most cases with a good prognosis compared to adults. We described a rare case of NMZL diagnosed in adolescent.
MeSH Terms
Figure
Reference
-
1. Ataş E, Kesik V, Fidancı MK, Kısmet E, Köseoğlu V. Evaluation of children with lympadenopathy. Turk Pediatri Ars. 2014; 49:30–35.
Article2. Park YW. Evaluation of neck masses in children. Am Fam Physician. 1995; 51:1904–1912.3. Gosche JR, Vick L. Acute, subacute, and chronic cervical lymphadenitis in children. Semin Pediatr Surg. 2006; 15:99–106.
Article4. Friedmann AM. Evaluation and management of lymphadenopathy in children. Pediatr Rev. 2008; 29:53–60.
Article5. Quintanilla-Martinez L, Sander B, Chan JK, Xerri L, Ott G, Campo E, et al. Indolent lymphomas in the pediatric population: follicular lymphoma, IRF4/MUM1+ lymphoma, nodal marginal zone lymphoma and chronic lymphocytic leukemia. Virchows Arch. 2016; 468:141–157.
Article6. Angelopoulou MK, Kalpadakis C, Pangalis GA, Kyrtsonis MC, Vassilakopoulos TP. Nodal marginal zone lymphoma. Leuk Lymphoma. 2014; 55:1240–1250.
Article7. Taddesse-Heath L, Pittaluga S, Sorbara L, Bussey M, Raffeld M, Jaffe ES. Marginal zone B-cell lymphoma in children and young adults. Am J Surg Pathol. 2003; 27:522–531.
Article8. Petit B, Chaury MP, Le Clorennec C, Jaccard A, Gachard N, Moalic-Judge S, et al. Indolent lymphoplasmacytic and marginal zone B-cell lymphomas: absence of both IRF4 and Ki67 expression identifies a better prognosis subgroup. Haematologica. 2005; 90:200–206.9. van den Brand M, van Krieken JH. Recognizing nodal marginal zone lymphoma: recent advances and pitfalls. A systematic review. Haematologica. 2013; 98:1003–1013.10. Au WY, Ma SY, Chim CS, Choy C, Loong F, Lie AK, et al. Clinicopathologic features and treatment outcome of mature T-cell and natural killer-cell lymphomas diagnosed according to the World Health Organization classification scheme: a single center experience of 10 years. Ann Oncol. 2005; 16:206–214.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of nodal marginal zone B-cell lymphoma of the lower eyelid
- A Case of Primary Nodal Type Marginal Zone B-Cell Lymphoma of the Intra-Parotid Lymph Node Mistaken to Primary Benign Parotid Mass
- A Case of Primary Cutaneous Marginal Zone B-cell Lymphoma
- A Case of Mucosa-Associated Lymphoid Tissue Lymphoma in Nasopharynx and Thyroid Gland
- A Case of Primary Cutaneous Marginal Zone B-cell Lymphoma Showing Monoclonal Rearrangement in Immunoglobulin Light Chain Gene