J Breast Cancer.
2016 Dec;19(4):459-464. 10.4048/jbc.2016.19.4.459.
Increased Malignant Microcalcifications after Neoadjuvant Chemotherapy in Advanced Breast Cancer
- Affiliations
-
- 1Department of Radiology, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. nanbarkym@hanmail.net
- 2Department of Pathology, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 3Department of Surgery, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 4Department of Nuclear Medicine, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2362934
- DOI: http://doi.org/10.4048/jbc.2016.19.4.459
Abstract
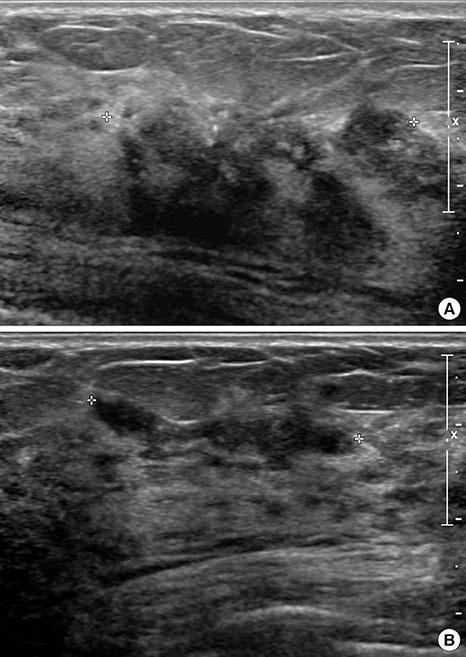
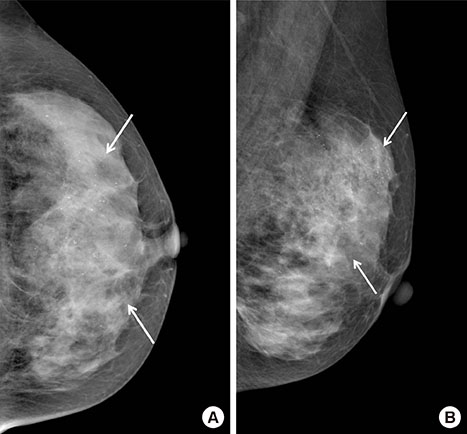
- In patients with advanced breast cancer, most new calcifications detected on a mammogram after neoadjuvant chemotherapy are benign dystrophic calcifications, but this is not always observed. We present a patient with advanced breast cancer who had paradoxically increased malignant microcalcifications concomitant with primary tumor regression after undergoing neoadjuvant chemotherapy. After the neoadjuvant chemotherapy, the follow-up mammogram revealed that local, fine pleomorphic microcalcifications had markedly increased. Pathologically, these calcifications were ductal carcinoma in situ. We concluded that, in patients with breast cancer undergoing neoadjuvant chemotherapy, newly developed microcalcifications on follow-up mammograms should be carefully evaluated, and any suspicious malignant microcalcifications should be included in surgical excision planning.
Keyword
MeSH Terms
Figure
Reference
-
1. Adrada BE, Huo L, Lane DL, Arribas EM, Resetkova E, Yang W. Histopathologic correlation of residual mammographic microcalcifications after neoadjuvant chemotherapy for locally advanced breast cancer. Ann Surg Oncol. 2015; 22:1111–1117.
Article2. Segel MC, Paulus DD, Hortobagyi GN. Advanced primary breast cancer: assessment at mammography of response to induction chemotherapy. Radiology. 1988; 169:49–54.
Article3. Moskovic EC, Mansi JL, King DM, Murch CR, Smith IE. Mammography in the assessment of response to medical treatment of large primary breast cancer. Clin Radiol. 1993; 47:339–344.
Article4. Fadul D, Rapelyea J, Schwartz AM, Brem RF. Development of malignant breast microcalcifications after neoadjuvant chemotherapy in advanced breast cancer. Breast J. 2004; 10:141–145.
Article5. Li JJ, Chen C, Gu Y, Di G, Wu J, Liu G, et al. The role of mammographic calcification in the neoadjuvant therapy of breast cancer imaging evaluation. PLoS One. 2014; 9:e88853.
Article6. Esserman LE, d'Almeida M, Da Costa D, Gerson DM, Poppiti RJ Jr. Mammographic appearance of microcalcifications: can they change after neoadjuvant chemotherapy? Breast J. 2006; 12:86–87.
Article7. Londero V, Bazzocchi M, Del Frate C, Puglisi F, Di Loreto C, Francescutti G, et al. Locally advanced breast cancer: comparison of mammography, sonography and MR imaging in evaluation of residual disease in women receiving neoadjuvant chemotherapy. Eur Radiol. 2004; 14:1371–1379.
Article8. Vinnicombe SJ, MacVicar AD, Guy RL, Sloane JP, Powles TJ, Knee G, et al. Primary breast cancer: mammographic changes after neoadjuvant chemotherapy, with pathologic correlation. Radiology. 1996; 198:333–340.
Article9. Gunia SR, Patel MS, Mamounas EP. Pathologic complete response of HER-2 neu-positive invasive ductal carcinoma and ductal carcinoma in situ following neoadjuvant chemotherapy plus trastuzumab: a case report and review of literature. Case Rep Surg. 2012; 2012:454273.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Mammography in Evaluating Residual Cancer after Neo-adjuvant Chemotherapy of Locally Advanced Breast Carcinoma: Compared with Clinical Examination
- Neoadjuvant Chemotherapy with Docetaxel and Adriamycin in Breast Cancer; Clincopathologic Factors Influencing to Response Rate
- Correlation between Tumor Response to Neoadjuvant Chemotherapy and Patient Outcome in Breast Cancer
- Diagnosis and Treatment of HER2-Positive Breast Cancer
- Predictive and Prognostic Roles of Pathological Indicators for Patients with Breast Cancer on Neoadjuvant Chemotherapy