Imaging Sci Dent.
2016 Dec;46(4):285-290. 10.5624/isd.2016.46.4.285.
Incidental finding of an extensive oropharyngeal mass in magnetic resonance imaging of a patient with temporomandibular disorder: A case report
- Affiliations
-
- 1Department of Oral Medicine, School of Dental Medicine, University of Pennsylvania, Philadelphia, PA, USA. akintoye@upenn.edu
- KMID: 2362748
- DOI: http://doi.org/10.5624/isd.2016.46.4.285
Abstract
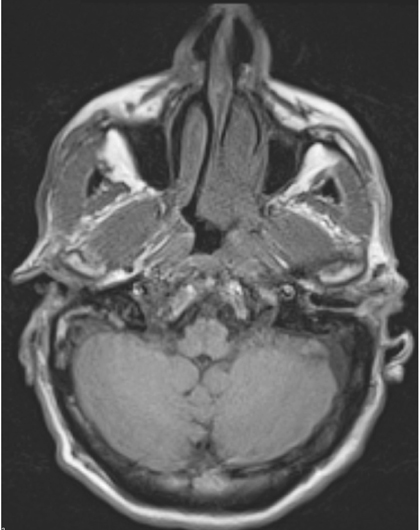
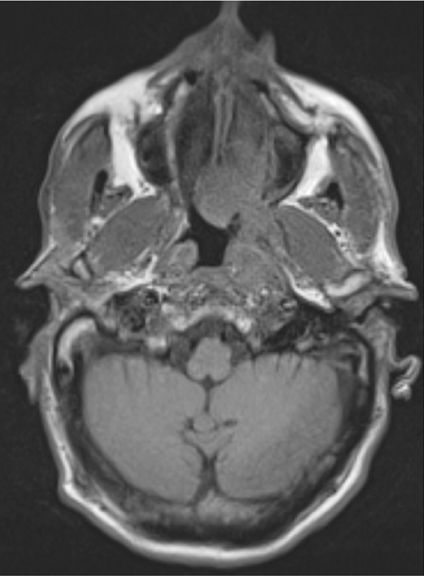
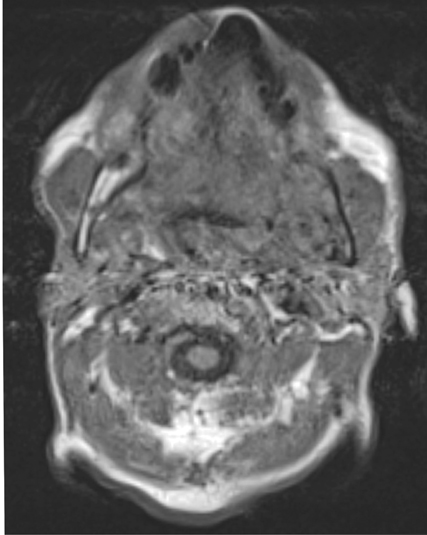
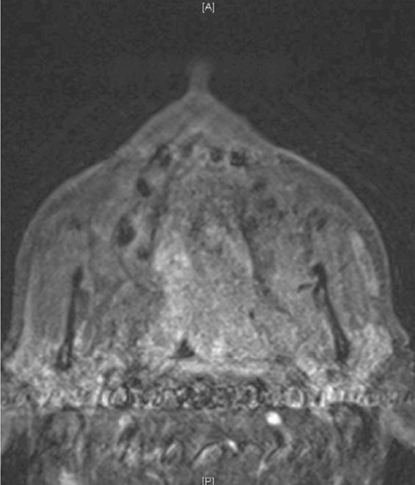
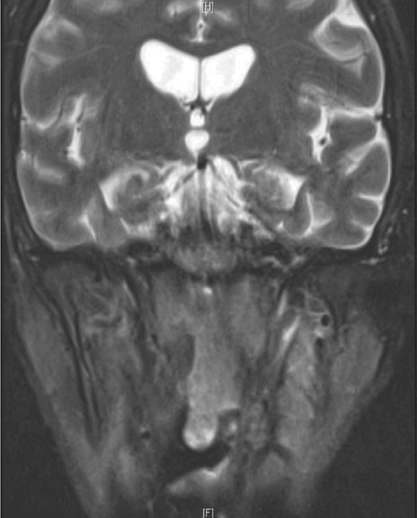
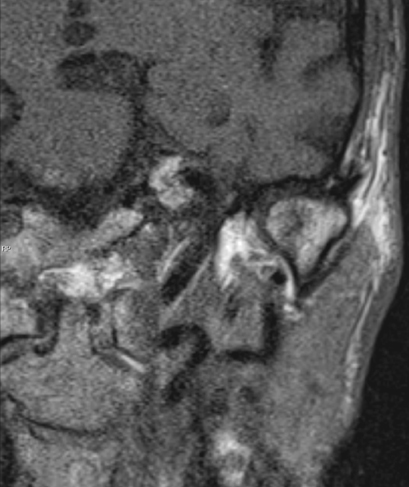
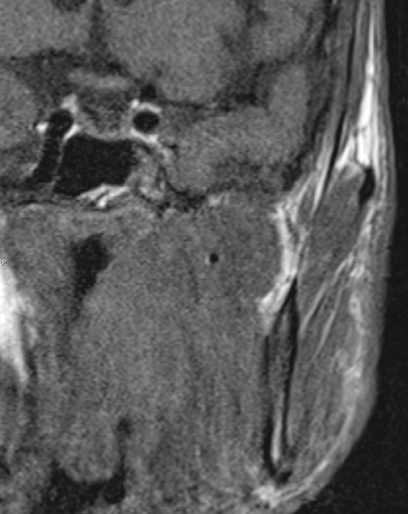
- In this report, we describe the incidental finding of an oropharyngeal mass in a patient who presented with a chief complaint of temporomandibular pain. The patient was initially evaluated by an otorhinolaryngologist for complaints of headaches, earache, and sinus congestion. Due to worsening headaches and trismus, he was further referred for the management of temporomandibular disorder. The clinical evaluation was uneventful except for limited mouth opening (trismus). An advanced radiological evaluation using magnetic resonance imaging revealed a mass in the nasopharyngeal/oropharyngeal region. The mass occupied the masticatory space and extended superioinferiorly from the skull base to the mandible. A diagnostic biopsy of the lesion revealed a long-standing human papilloma virus (HPV-16)-positive squamous cell carcinoma of the oropharynx. This case illustrates the need for the timely radiological evaluation of seemingly innocuous orofacial pain.
MeSH Terms
Figure
Cited by 1 articles
-
Clinical diagnostic guidelines of allergic rhinitis: comprehensive treatment and consideration of special circumstances
Young Hyo Kim, Sang Min Lee, Mi-Ae Kim, Hyeon-Jong Yang, Jeong-Hee Choi, Dong-Kyu Kim, Young Yoo, Bong-Seong Kim, Won-Young Kim, Jeong Hee Kim, So Yeon Park, Keejae Song, Min-Suk Yang, Young-Mok Lee, Hyun Jong Lee, Jae-Hong Cho, Hye Mi Jee, Yang Park, Woo Yong Bae, Young-Il Koh,
J Korean Med Assoc. 2017;60(3):257-269. doi: 10.5124/jkma.2017.60.3.257.
Reference
-
1. Grosskopf CC, Kuperstein AS, O'Malley BW Jr, Sollecito TP. Parapharyngeal space tumors: another consideration for otalgia and temporomandibular disorders. Head Neck. 2013; 35:E153–E156.
Article2. Reiter S, Gavish A, Emodi-Perlman A, Eli I. Nasopharyngeal carcinoma mimicking a temporomandibular disorder: a case report. J Orofac Pain. 2006; 20:74–81.3. Lewis A, Kang R, Levine A, Maghami E. The new face of head and neck cancer: the HPV epidemic. Oncology (Williston Park). 2015; 29:616–626.4. Omolehinwa TT, Musbah T, Desai B, O'Malley BW Jr, Stoopler ET. Neuralgia associated with transcutaneous electrical nerve stimulation therapy in a patient initially diagnosed with temporomandibular disorder. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015; 119:e101–e104.
Article5. Sari-Rieger A, Hassfeld S, Junker K, Rustemeyer J. Adenoid cystic carcinoma of the skull base mimicking temporomandibular disorder. Oral Maxillofac Surg. 2014; 18:115–118.
Article6. Schneider A, Forstner R. The value of MRI in imaging malignant head and neck tumours. Imaging Decis MRI. 2007; 11:3–10.
Article7. Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. 2006; 102:1867–1878.
Article8. Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011; 29:4294–4301.
Article9. Lewis JS Jr, Thorstad WL, Chernock RD, Haughey BH, Yip JH, Zhang Q, et al. p16 positive oropharyngeal squamous cell carcinoma: an entity with a favorable prognosis regardless of tumor HPV status. Am J Surg Pathol. 2010; 34:1088–1096.10. Chen RC, Khorsandi AS, Shatzkes DR, Holliday RA. The radiology of referred otalgia. AJNR Am J Neuroradiol. 2009; 30:1817–1823.
Article11. Pitiyage G, Lei M, Guererro Urbano T, Odell E, Thavaraj S. Biphenotypic human papillomavirus-associated head and neck squamous cell carcinoma: a report of two cases. Diagn Pathol. 2015; 10:97.
Article12. Hennessey PT, Westra WH, Califano JA. Human papillomavirus and head and neck squamous cell carcinoma: recent evidence and clinical implications. J Dent Res. 2009; 88:300–306.
Article13. Deschler DG, Richmon JD, Khariwala SS, Ferris RL, Wang MB. The “new” head and neck cancer patient-young, nonsmoker, nondrinker, and HPV positive: evaluation. Otolaryngol Head Neck Surg. 2014; 151:375–380.14. Lorincz BB, Jowett N, Knecht R. Decision management in transoral robotic surgery: indications, individual patient selection, and role in the multidisciplinary treatment for head and neck cancer from a European perspective. Head Neck. 2016; 38:Suppl 1. E2190–E2196.
Article15. Agulnik M, Epstein JB. Nasopharyngeal carcinoma: current management, future directions and dental implications. Oral Oncol. 2008; 44:617–627.
Article16. Fischer DJ, Klasser GD, Epstein JB. Cancer and orofacial pain. Oral Maxillofac Surg Clin North Am. 2008; 20:287–301.
Article17. Kamran SC, Riaz N, Lee N. Nasopharyngeal carcinoma. Surg Oncol Clin N Am. 2015; 24:547–561.
Article18. Khan J, Quek SY, Markman S. Nasopharyngeal carcinoma masquerading as TMJ orofacial pain. Quintessence Int. 2010; 41:387–389.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Analysis of Incidental Findings on Temporomandibular Joint Magnetic Resonance Imaging
- A case of Bell’s palsy with an incidental finding of facial nerve schwannoma: comparison of magnetic resonance imaging findings
- Heterotopic Pancreas with Abundant Fat Tissue in the Stomach: A Case Report
- MR Imaging and Ultrasonographic Findings of Tensor Fasciae Suralis Muscle: A Case Report
- Organized hematoma of temporomandibular joint