J Korean Ophthalmol Soc.
2016 Dec;57(12):1946-1952. 10.3341/jkos.2016.57.12.1946.
Three Cases of Periorbital Nodular Fasciitis
- Affiliations
-
- 1Department of Ophthalmology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea. minjounglee77@gmail.com
- 2Department of Pathology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- KMID: 2362714
- DOI: http://doi.org/10.3341/jkos.2016.57.12.1946
Abstract
- PURPOSE
Herein, we report 3 cases of nodular fasciitis presenting with periorbital mass.
CASE SUMMARY
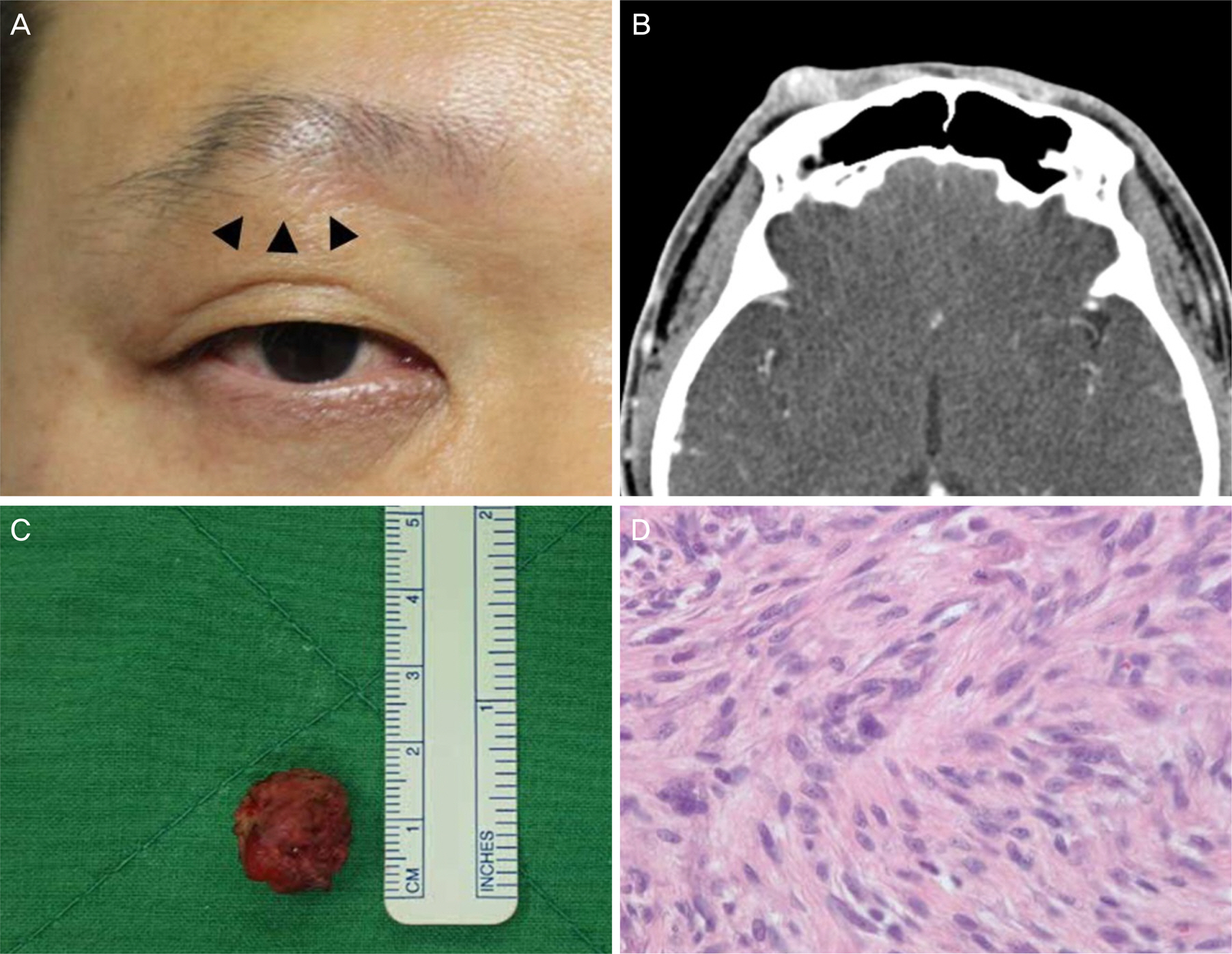
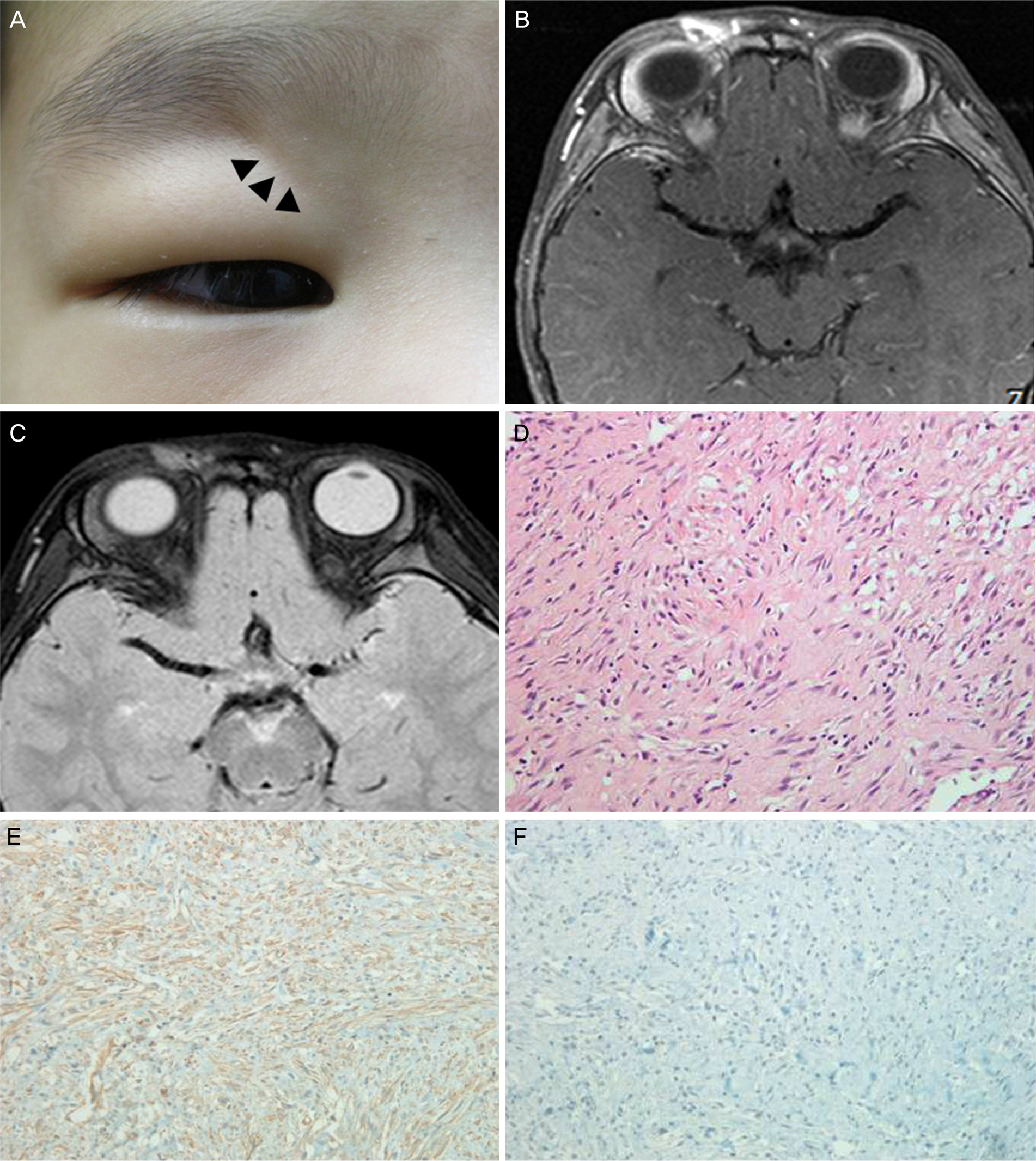
An 18-year-old male presented with a mass in his left lateral temple area 3 months in duration. On physical examination, a subcutaneous mass approximately 20 mm in size was palpable with upper eyelid swelling. Orbital magnetic resonance imaging (MRI) showed T1 isointensity and T2 hyper intensity and a well-circumscribed enhancing lesion. A 36-year-old male presented with a 6-month history of a bump under his right upper eyelid. External examination revealed a 15 mm-sized subcutaneous mass in the right central sub-brow area. Orbital computed tomography showed a homogenous, well-circumscribed mass with moderate enhancement. A 3-year-old boy presented with a mass in his right upper eyelid 4 months in duration. A subcutaneous mass approximately 10 mm in size was palpated at the medial superior orbital rim. Orbital MRI revealed an enhanced mass of irregular shape. Surgical excision was performed for all cases. Histopathological examination showed pathognomonic proliferation of spindle cells and immunohistochemical stains showed the spindle cells were positive for smooth muscle actin, negative for S-100 and negative for CD34, consistent with nodular fasciitis. Recurrence of the tumors after excision in the 3 cases was not observed after 4 months, 3 months and 48 months, respectively.
CONCLUSIONS
Nodular fasciitis is rare but can occur at the periorbital region. In particular, nodular fasciitis should be considered as a differential diagnosis of a subcutaneous mass short in duration in children or young adults.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Case Report of Nodular Fasciitis in the Conjunctiva
Jin-ho Kim, Kyung Sun Na, Chang-hyun Park, Seung Jin Lee, Tae Hoon Oh, Hyun Seung Kim
J Korean Ophthalmol Soc. 2020;61(3):303-306. doi: 10.3341/jkos.2020.61.3.303.
Reference
-
References
1. Riffle JE, Prosser AH, Lee JR, Lynn JJ. Nodular fasciitis of the abdominal: a case report and brief review of the literature. Case Rep Ophthalmol Med. 2011; 2011:235956.2. Yanagisawa A, Okada H. Nodular fasciitis with degeneration and regression. J Craniofac Surg. 2008; 19:1167–70.
Article3. Konwaler BE, Keasbey L, Kaplan L. Subcutaneous pseudosarcom-atous fibromatosis (fasciitis). Am J Clin Pathol. 1955; 25:241–52.
Article4. Yoo G, Baek SO, Jung SN, et al. Nodular fasciitis in the forehead. J Craniofac Surg. 2010; 21:925–6.
Article5. Silva P, Bruce IA, Malik T, et al. Nodular fasciitis of the head and neck. J Laryngol Otol. 2005; 119:8–11.
Article6. DiNardo LJ, Wetmore RF, Potsic WP. Nodular fasciitis of the head and neck in children. A deceptive lesion. Arch Otolaryngol Head Neck Surg. 1991; 117:1001–2.
Article7. Stanley MW, Skoog L, Tani EM, Horwitz CA. Nodular fasciitis: spontaneous resolution following diagnosis by fine-needle aspiration. Diagn Cytopathol. 1993; 9:322–4.
Article8. Font RL, Zimmerman LE. Nodular fasciitis of the eye and adnexa. A report of ten cases. Arch Ophthalmol. 1966; 75:475–81.9. Gupta D, Tailor TD, Keene CD, et al. A case of nodular fasciitis causing compressive optic neuropathy. Ophthal Plast Reconstr Surg. 2014; 30:e47–9.
Article10. Choi HJ, Jung KH, Lee HJ. Nodular fasciitis on temple area abdominal in surgical trauma. J Craniofac Surg. 2014; 25:e546–8.11. de Paula SA, Cruz AA, de Alencar VM, et al. Nodular fasciitis abdominal as a large mass in the upper eyelid. Ophthal Plast Reconstr Surg. 2006; 22:494–5.12. Husain A, Cummings T, Richard MJ, Woodward JA. Nodular abdominal presenting in an adult woman. Ophthal Plast Reconstr Surg. 2011; 27:e168–70.13. Shields JA, Shields CL, Christian C, Eagle RC Jr. Orbital nodular fasciitis simulating a dermoid cyst in an 8-month-old child. Case report and review of the literature. Ophthal Plast Reconstr Surg. 2001; 17:144–8.14. Jung SW, Kang NY. A case of nodular fasciitis in the upper eyelid. J Korean Ophthalmol Soc. 2008; 49:357–61.
Article15. Anzeljc AJ, Oliveira AM, Grossniklaus HE, et al. Nodular fasciitis of the orbit: a case report confirmed by molecular cytogenetic analysis. Ophthal Plast Reconstr Surg. 2016:Feb 12; [Epub ahead of print].
Article16. Damasceno RW, Heindl LM, Szentmáry N, et al. Nodular fasciitis of the eyelid and anterior orbit in children: case report and review of the literature. Ophthalmologe. 2009; 106:829–31.17. Sakamoto T, Ishibashi T, Ohnishi Y, Inomata H. Immunohistological and electron microscopical study of nodular fasciitis of the orbit. Br J Ophthalmol. 1991; 75:636–8.
Article18. Meyer CA, Kransdorf MJ, Jelinek JS, Moser RP Jr. MR and CT abdominal of nodular fasciitis. J Comput Assist Tomogr. 1991; 15:276–9.19. Lin XY, Wang L, Zhang Y, et al. Variable Ki67 proliferative index in 65 cases of nodular fasciitis, compared with fibrosarcoma and fibromatosis. Diagn Pathol. 2013; 8:50.
Article20. Amary MF, Ye H, Berisha F, et al. Detection of USP6 gene re-arrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013; 463:97–8.
Article21. Erickson-Johnson MR, Chou MM, Evers BR, et al. Nodular abdominal: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011; 91:1427–33.22. Vestal KP, Bauer TW, Berlin AJ. Nodular fasciitis presenting as an eyelid mass. Ophthal Plast Reconstr Surg. 1990; 6:130–2.
Article23. Allison DB, Wakely PE Jr, Siddiqui MT, Ali SZ. Nodular fasciitis: a frequent diagnostic pitfall on fine-needle aspiration. Cancer Cytopathol. 2016; Aug 15:doi:. DOI: 10.1002/cncy.21768. [Epub ahead of print].
Article