Pediatr Infect Vaccine.
2016 Dec;23(3):172-179. 10.14776/piv.2016.23.3.172.
Molecular Epidemiology of Bacillus cereus in a Pediatric Cancer Center
- Affiliations
-
- 1Department of Pediatrics, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea.
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. yaejeankim@skku.edu
- 3Center for Clinical Research, Samsung Biomedical Research Institute, Seoul, Korea.
- 4Department of Pediatrics, Good Gang-An Hospital, Busan, Korea.
- 5Department of Laboratory Medicine and Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2362475
- DOI: http://doi.org/10.14776/piv.2016.23.3.172
Abstract
- PURPOSE
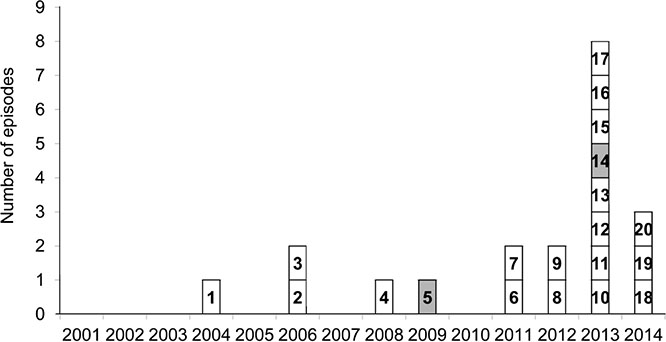
Bacillus cereus has been reported as the cause of nosocomial infections in cancer patients. In our pediatric cancer ward, a sudden rise in the number of patients with B. cereus bacteremia was observed in 2013 to 2014. This study was performed to investigate the molecular epidemiology of increased B. cereus bacteremia cases in our center.
METHODS
Pediatric cancer patients who developed B. cereus bacteremia were identified from January 2001 to June 2014. The B. cereus bacteremia in this study was defined as a case in which at least one B. cereus identified in blood cultures, regardless of true bacteremia. Available isolates were further tested by multilocus sequence typing (MLST) analysis. A retrospective chart review was performed.
RESULTS
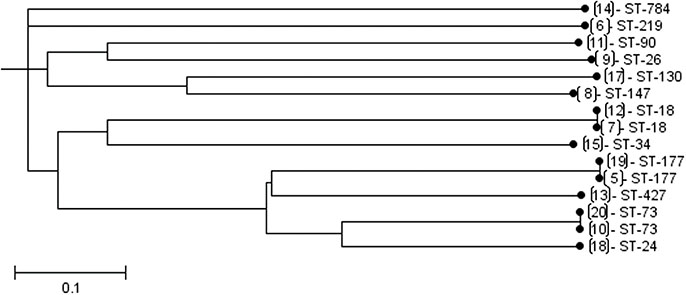
Nineteen patients developed B. cereus bacteremia during the study period. However, in 2013, a sudden increase in the number of patients with B. cereus bacteremia was observed. In addition, three patients developed B. cereus bacteremia within 1 week in July and the other three patients within 1 week in October, respectively, during emergency room renovation. However, MLST analysis revealed different sequence types without consistent patterns. Before 2013, five tested isolates were ST18, ST26, ST177, and ST147-like type, and ST219-like type. Isolates from 2013 were ST18, ST73, ST90, ST427, ST784, ST34-like type, and ST130-like type.
CONCLUSIONS
MLST analyses showed variable ST distribution of B. cereus isolates. Based on this study, there was no significant evidence suggesting a true outbreak caused by a single ST among patients who developed B. cereus bacteremia.
MeSH Terms
Figure
Reference
-
1. Drobniewski FA. Bacillus cereus and related species. Clin Microbiol Rev. 1993; 6:324–338.
Article2. Pirttijarvi TS, Andersson MA, Scoging AC, Salkinoja-Salonen MS. Evaluation of methods for recognising strains of the Bacillus cereus group with food poisoning potential among industrial and environmental contaminants. Syst Appl Microbiol. 1999; 22:133–144.
Article3. Slaten DD, Oropeza RI, Werner SB. An outbreak of Bacillus cereus food poisoning: are caterers supervised sufficiently. Public Health Rep. 1992; 107:477–480.4. Ozkocaman V, Ozcelik T, Ali R, Ozkalemkas F, Ozkan A, Ozakin C, et al. Bacillus spp. among hospitalized patients with haematological malignancies: clinical features, epidemics and outcomes. J Hosp Infect. 2006; 64:169–176.
Article5. Akiyama N, Mitani K, Tanaka Y, Hanazono Y, Motoi N, Zarkovic M, et al. Fulminant septicemic syndrome of Bacillus cereus in a leukemic patient. Intern Med. 1997; 36:221–226.
Article6. Arnaout MK, Tamburro RF, Bodner SM, Sandlund JT, Rivera GK, Pui CH, et al. Bacillus cereus causing fulminant sepsis and hemolysis in two patients with acute leukemia. J Pediatr Hematol Oncol. 1999; 21:431–435.
Article7. Gaur AH, Patrick CC, McCullers JA, Flynn PM, Pearson TA, Razzouk BI, et al. Bacillus cereus bacteremia and meningitis in immunocompromised children. Clin Infect Dis. 2001; 32:1456–1462.
Article8. Hilliard NJ, Schelonka RL, Waites KB. Bacillus cereus bacteremia in a preterm neonate. J Clin Microbiol. 2003; 41:3441–3444.9. John AB, Razak EA, Razak EE, Al-Naqeeb N, Dhar R. Intractable Bacillus cereus bacteremia in a preterm neonate. J Trop Pediatr. 2007; 53:131–132.
Article10. Kiyomizu K, Yagi T, Yoshida H, Minami R, Tanimura A, Karasuno T, et al. Fulminant septicemia of Bacillus cereus resistant to carbapenem in a patient with biphenotypic acute leukemia. J Infect Chemother. 2008; 14:361–367.
Article11. Orrett FA. Fatal Bacillus cereus bacteremia in a patient with diabetes. J Natl Med Assoc. 2000; 92:206–208.12. Sasahara T, Hayashi S, Morisawa Y, Sakihama T, Yoshimura A, Hirai Y. Bacillus cereus bacteremia outbreak due to contaminated hospital linens. Eur J Clin Microbiol Infect Dis. 2011; 30:219–226.
Article13. Dohmae S, Okubo T, Higuchi W, Takano T, Isobe H, Baranovich T, et al. Bacillus cereus nosocomial infection from reused towels in Japan. J Hosp Infect. 2008; 69:361–367.
Article14. Barrie D, Hoffman PN, Wilson JA, Kramer JM. Contamination of hospital linen by Bacillus cereus. Epidemiol Infect. 1994; 113:297–306.15. Helgason E, Tourasse NJ, Meisal R, Caugant DA, Kolsto AB. Multilocus sequence typing scheme for bacteria of the Bacillus cereus group. Appl Environ Microbiol. 2004; 70:191–201.
Article16. Maiden MC, Bygraves JA, Feil E, Morelli G, Russell JE, Urwin R, et al. Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci U S A. 1998; 95:3140–3145.
Article17. Mignot T, Denis B, Couture-Tosi E, Kolsto AB, Mock M, Fouet A. Distribution of S-layers on the surface of Bacillus cereus strains: phylogenetic origin and ecological pressure. Environ Microbiol. 2001; 3:493–501.
Article18. Berger SA. Pseudobacteremia due to contaminated alcohol swabs. J Clin Microbiol. 1983; 18:974–975.
Article19. Weber DJ, Sickbert-Bennett E, Gergen MF, Rutala WA. Efficacy of selected hand hygiene agents used to remove Bacillus atrophaeus (a surrogate of Bacillus anthracis) from contaminated hands. JAMA. 2003; 289:1274–1277.
Article20. Maki DG. Through a glass darkly. Nosocomial pseudoepidemics and pseudobacteremias. Arch Intern Med. 1980; 140:26–28.
Article21. Ohsaki Y, Koyano S, Tachibana M, Shibukawa K, Kuroki M, Yoshida I, et al. Undetected Bacillus pseudo-outbreak after renovation work in a teaching hospital. J Infect. 2007; 54:617–622.
Article22. Morris T, Brecher SM, Fitzsimmons D, Durbin A, Arbeit RD, Maslow JN. A pseudoepidemic due to laboratory contamination deciphered by molecular analysis. Infect Control Hosp Epidemiol. 1995; 16:82–87.
Article23. Barker M, Thakker B, Priest FG. Multilocus sequence typing reveals that Bacillus cereus strains isolated from clinical infections have distinct phylogenetic origins. FEMS Microbiol Lett. 2005; 245:179–184.
Article24. Vassileva M, Torii K, Oshimoto M, Okamoto A, Agata N, Yamada K, et al. Phylogenetic analysis of Bacillus cereus isolates from severe systemic infections using multilocus sequence typing scheme. Microbiol Immunol. 2006; 50:743–749.
Article25. Raymond B, Wyres KL, Sheppard SK, Ellis RJ, Bonsall MB. Environmental factors determining the epidemiology and population genetic structure of the Bacillus cereus group in the field. PLoS Pathog. 2010; 6:e1000905.
Article26. Klee SR, Ozel M, Appel B, Boesch C, Ellerbrok H, Jacob D, et al. Characterization of Bacillus anthracis-like bacteria isolated from wild great apes from Cote d'Ivoire and Cameroon. J Bacteriol. 2006; 188:5333–5344.
Article27. Loeb M, Wilcox L, Thornley D, Gun-Munro J, Richardson H. Bacillus species pseudobacteremia following hospital construction. Can J Infect Control. 1995; 10:37–40.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraventricular Vancomycin Therapy for Intractable Bacillus cereus Ventriculitis
- Analysis of Kudoa septempunctata as a cause of foodborne illness and its associated differential diagnosis
- A Case of Bacillus Cereus Infection with Pneumonia and Bactermia
- Surveillance of Bacillus cereus Isolates in Korea from 2012 to 2014
- Whole genome sequence analyses of thermotolerant Bacillus sp. isolates from food