Clin Exp Otorhinolaryngol.
2016 Dec;9(4):339-345. 10.21053/ceo.2015.01641.
The Lung Function Impairment in Non-Atopic Patients With Chronic Rhinosinusitis and Its Correlation Analysis
- Affiliations
-
- 1Department of Otolaryngology, First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China. zlh268401@163.com
- 2Department of Otolaryngology-Head and Neck Surgery, Beijing Tongren Hospital, Capital Medical University, Ministry of Education, Beijing, China.
- KMID: 2360765
- DOI: http://doi.org/10.21053/ceo.2015.01641
Abstract
OBJECTIVES
Chronic rhinosinusitis (CRS) is common disease in otorhinolaryngology and will lead to lower airway abnormality. However, the only lung function in CRS patients and associated factors have not been much studied.
METHODS
One hundred patients with CRS with nasal polyps (CRSwNP group), 40 patients with CRS without nasal polyps (CRSsNP group), and 100 patients without CRS were enrolled. The difference in lung function was compared. Meanwhile, CRSwNP and CRSsNP group were required to undergo a bronchial provocation or dilation test. Additionally, subjective and objective outcomes were measured by the visual analogue scale (VAS), 20-item Sino-Nasal Outcome Test (SNOT-20), Lund-Mackay score, Lund-Kennedy endoscopic score. The correlation and regression methods were used to analyze the relationship between their lung function and the above parameters.
RESULTS
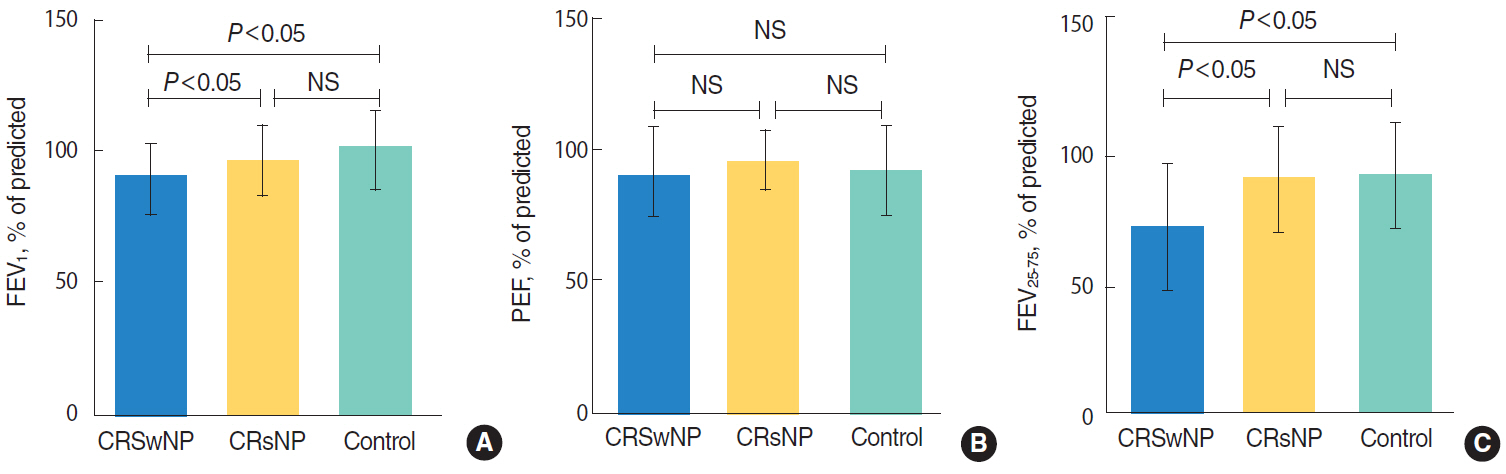
The forced expiratory volume in 1 second (FEV1) and forced expiratory flow between 25% and 75% of forced vital capacity (FEF25-75) of CRSwNP group were significantly lower than other groups (P<0.05). On peak expiratory flow, there was no difference between three groups. In CRSwNP group, FEV1 was negatively correlated with peripheral blood eosinophil count (PBEC) and duration of disease (r=-0.348, P=0.013 and r=-0.344, P=0.014, respectively), FEF25-75 negatively with VAS, SNOT-20 (r=-0.490, P=0.028 and r=-0.478, P=0.033, respectively) in CRSsNP group. The incidence of positive bronchial provocation and dilation test was lower in CRSwNP group (10% and 0%, respectively), with both 0% in CRSsNP group. The multiple linear regression analysis indicated that change ratio of FEV1 before and after bronchial provocation or dilation test were correlated with PBEC in CRSwNP group (β=0.403, P=0.006).
CONCLUSION
CRS leading to impaired maximum ventilation and small airway is associated with the existence of nasal polyp. Lung function impairments can be reflected by PBEC, duration, VAS, and SNOT-20. In CRSwNP patients, PBEC is independent predictor of FEVâ‚ change ratio.
Keyword
MeSH Terms
Figure
Reference
-
1. Rosenfeld RM, Andes D, Bhattacharyya N, Cheung D, Eisenberg S, Ganiats TG, et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007; 137(3 Suppl):S1–31.
Article2. Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2000 summary. Adv Data. 2002; (328):1–32.3. Anon JB, Jacobs MR, Poole MD, Ambrose PG, Benninger MS, Hadley JA, et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004; 130(1 Suppl):1–45.
Article4. Bousquet J, van Cauwenberge P, Khahaev N. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001; 108(5 Suppl):S147–334.
Article5. Kim HY, So YK, Dhong HJ, Chung SK, Choi DC, Kwon NH, et al. Prevalence of lower airway diseases in patients with chronic rhinosinusitis. Acta Otoaryngol. 2007; 127(Suppl 558):110–4.6. Williamson PA, Vaidyanathan S, Clearie K, Barnes M, Lipworth BJ. Airway dysfunction in nasal polyposis: a spectrum of asthmatic disease? Clin Exp Allergy. 2011; 41(10):1379–85.
Article7. Ciprandi G, Cirillo I, Vizzaccaro A, Monardo M, Tosca MA. Early bronchial airflow impairment in patients with persistent allergic rhinitis and bronchial hyperreactivity. Respir Med. 2005; 99(12):1606–12.
Article8. Konstantinou GN, Bousquet PJ, Zuberbier T, Papadopoulos NG. The longest wheal diameter is the optimal measurement for the evaluation of skin prick tests. Int Arch Allergy Immunol. 2010; 151(4):343–5.
Article9. Lim M, Lew-Gor S, Darby Y, Brookes N, Scadding G, Lund VJ. The relationship between subjective assessment instruments in chronic rhinosinusitis. Rhinology. 2007; 45(2):144–7.10. Piccirillo JF, Merritt MG Jr, Richards ML. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol Head Neck Surg. 2002; 126(1):41–7.
Article11. Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg. 1997; 117(3 Pt 2):S35–40.
Article12. Bachert C, Vignola AM, Gevaert P, Leynaert B, Van Cauwenberge P, Bousquet J. Allergic rhinitis, rhinosinusitis, and asthma: one airway disease. Immunol Allergy Clin North Am. 2004; 24(1):19–43.
Article13. Jani AL, Hamilos DL. Current thinking on the relationship between rhinosinusitis and asthma. J Asthma. 2005; 42(1):1–7.
Article14. de Benedictis FM, Bush A. Rhinosinusitis and asthma: epiphenomenon or causal association. Chest. 1999; 115(2):550–6.15. Vizzaccaro A, Cirillo I, Pallestrini E, Ciprandi G. Allergic rhinitis frequently impairs bronchial function. Recenti Prog Med. 2004; 95(5):251–3.16. McCusker CT. Use of mouse models of allergic rhinitis to study the upper and lower airway link. Curr Opin Allergy Clin Immunol. 2004; 4(1):11–6.
Article17. Kariya S, Okano M, Oto T, Higaki T, Makihara S, Haruna T, et al. Pulmonary function in patients with chronic rhinosinusitis and allergic rhinitis. J Laryngol Otol. 2014; 128(3):255–62.
Article18. Lee SY, Yoon SH, Song WJ, Lee SH, Kang HR, Kim SS, et al. Influence of chronic sinusitis and nasal polyp on the lower airway of subjects without lower airway diseases. Allergy Asthma Immunol Res. 2014; 6(4):310–5.
Article19. Ciprandi G, Cirillo I, Pistorio A. Impact of allergic rhinitis on asthma: effects on spirometric parameters. Allergy. 2008; 63(3):255–60.20. Ferguson B, Powell-Davis A. The link between upper and lower respiratory disease. Curr Opin Otolaryngol Head Neck Surg. 2003; 11(3):192–5.
Article21. Okayama M, Iijima H, Shimura S, Shimomura A, Ikeda K, Okayama H, et al. Methacholine bronchial hyperresponsiveness in chronic sinusitis. Respiration. 1998; 65(6):450–7.22. Gu Xiao, Ye Ping, Chen Feng-Yi, Chen Yan-Lin, Yang Yan, Shi Li. The analysis of the characteristics of pulmonary function tests in patients with nasal polyps and clinical value. J Shandong Univ. 2011; 24(10):1–45.23. Shaaban R, Zureik M, Soussan D, Anto JM, Heinrich J, Janson C, et al. Allergic rhinitis and onset of bronchial hyperresponsiveness: a population-based study. Am J Respir Crit Care Med. 2007; 176(7):659–66.24. Kang SH, Kim HY, Seo JH, Kwon JW, Jung YH, Song YH, et al. Bronchial hyperresponsiveness to methacholine and AMP in children with atopic asthma. Allergy Asthma Immunol Res. 2012; 4(6):341–5.
Article25. Tanaka S, Hirota T, Kamijo A, Ishii H, Hatsushika K, Fujieda S, et al. Lung functions of Japanese patients with chronic rhinosinusitis who underwent endoscopic sinus surgery. Allergol Int. 2014; 63(1):27–35.
Article26. Huang Z, Zhou B, Zhang Q, Huang Q, Sun Y, Wang M, et al. The role of upper and lower airway patency in chronic rhinosinusitis with nasal polyps and asthma. Laryngoscope. 2013; 123(3):569–73.
Article27. Fan Y, Chen S, Qu X, Zuo K, Li X, Huang J, et al. A lower prevalence of asthma among patients with chronic rhinosinusitis in southern China. J Allergy Clin Immunol. 2011; 127(2):520–2. e1-5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Case study of ventilatory function of lung cancer, bronchial asthma, chronic bronchitis and lung emphysema -Case Report-
- Medical treatment according to phenotypes of chronic rhinosinusitis
- The Role of Allergy in the Severity of Chronic Rhinosinusitis
- Clinical Characteristics and Treatment of Fungal Rhinosinusitis
- The Clinical Significance of Lund-Mackay CT Staging System in Assessing the Severity of Chronic Rhinosinusitis