Anesth Pain Med.
2016 Oct;11(4):362-365. 10.17085/apm.2016.11.4.362.
Hemisphere cerebral infarction after total laparoscopic hysterectomy in the Trendelenburg position: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. hyunkyolim@yonsei.ac.kr
- KMID: 2358332
- DOI: http://doi.org/10.17085/apm.2016.11.4.362
Abstract
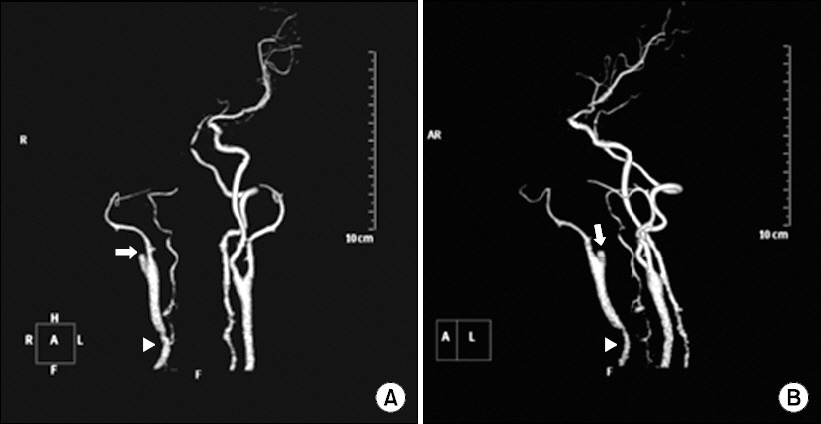
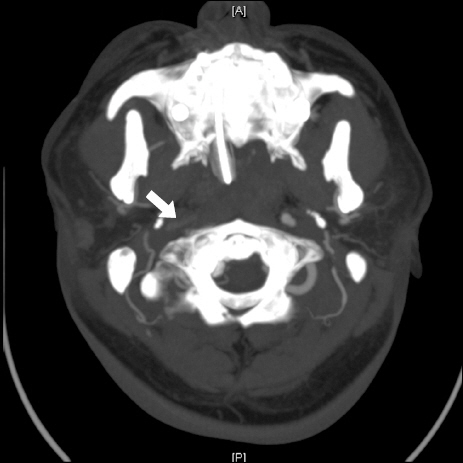
- Perioperative stroke can lead to mortality or serious disability and usually occurs in patients undergoing cardiac, vascular, or neurologic surgery; it is rare in gynecological surgery. We report the case of a patient who suffered life-threatening cerebral infarction after elective laparoscopic hysterectomy. During the surgery, the patient was placed in the Trendelenburg position. On postoperative day one, the patient was diagnosed with right hemisphere cerebral infarction; brain computed tomographic angiography showed proximal right internal carotid artery occlusion. Decompressive craniectomy was performed to resolve brain swelling, but the patient died 10 days later.
MeSH Terms
Figure
Reference
-
1. Ng JL, Chan MT, Gelb AW. Perioperative stroke in noncardiac, nonneurosurgical surgery. Anesthesiology. 2011; 115:879–90. DOI: 10.1097/ALN.0b013e31822e9499. PMID: 21862923.
Article2. Selim M. Perioperative stroke. N Engl J Med. 2007; 356:706–13. DOI: 10.1056/NEJMra062668. PMID: 17301301.
Article3. Lee JW, Kang H, Lim TH, Kim EG. A case of postpartum cerebral angiopathy with intracranial hemorrhage in Cesarean delivery. Anesth Pain Med. 2012; 7:359–62.4. Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Georgia wR. ‘Malignant’ middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996; 53:309–15. DOI: 10.1001/archneur.1996.00550040037012. PMID: 8929152.5. Likosky DS, Marrin CA, Caplan LR, Baribeau YR, Morton JR, Weintraub RM, et al. Determination of etiologic mechanisms of strokes secondary to coronary artery bypass graft surgery. Stroke. 2003; 34:2830–4. DOI: 10.1161/01.STR.0000098650.12386.B3. PMID: 14605327.
Article6. Liapis CD, Bell PR, Mikhailidis D, Sivenius J, Nicolaides A, Fernandese Fernandes J, et al. ESVS guidelines Invasive treatment for carotid stenosis: indications, techniques. Eur J Vasc Endovasc Surg. 2009; 37(4 Suppl):1–19. DOI: 10.1016/j.ejvs.2008.11.006. PMID: 19286127.
Article7. Hofmeijer J, Algra A, Kappelle LJ, van der Worp HB. Predictors of life-threatening brain edema in middle cerebral artery infarction. Cerebrovasc Dis. 2008; 25:176–84. DOI: 10.1159/000113736. PMID: 18212524.
Article8. von Kummer R, Bourquain H, Bastianello S, Bozzao L, Manelfe C, Meier D, et al. Early prediction of irreversible brain damage after ischemic stroke at CT. Radiology. 2001; 219:95–100. DOI: 10.1148/radiology.219.1.r01ap0695. PMID: 11274542.
Article9. Kasner SE, Demchuk AM, Berrouschot J, Schmutzhard E, Harms L, Verro P, et al. Predictors of fatal brain edema in massive hemispheric ischemic stroke. Stroke. 2001; 32:2117–23. DOI: 10.1161/hs0901.095719. PMID: 11546905.
Article10. El-Saed A, Kuller LH, Newman AB, Lopez O, Costantino J, McTigue K, et al. Geographic variations in stroke incidence and mortality among older populations in four US communities. Stroke. 2006; 37:1975–9. DOI: 10.1161/01.STR.0000231453.98473.67.
Article11. Hart R, Hindman B. Mechanisms of perioperative cerebral infarction. Stroke. 1982; 13:766–73. DOI: 10.1161/01.STR.13.6.766. PMID: 7147290.
Article12. Mavrocordatos P, Bissonnette B, Ravussin P. Effects of neck position and head elevation on intracranial pressure in anaesthetized neurosurgical patients: preliminary results. J Neurosurg Anesthesiol. 2000; 12:10–4. DOI: 10.1097/00008506-200001000-00003. PMID: 10636614.13. Dunham CM, Sosnowski C, Porter JM, Siegal J, Kohli C. Correlation of noninvasive cerebral oximetry with cerebral perfusion in the severe head injured patient: a pilot study. J Trauma. 2002; 52:40–6. DOI: 10.1097/00005373-200201000-00009.
Article14. Park EY, Koo BN, Min KT, Nam SH. The effect of pneumoperitoneum in the steep Trendelenburg position on cerebral oxygenation. Acta Anaesthesiol Scand. 2009; 53:895–9. DOI: 10.1111/j.1399-6576.2009.01991.x. PMID: 19426238.
Article15. Hirvonen EA, Nuutinen LS, Kauko M. Hemodynamic changes due to Trendelenburg positioning and pneumoperitoneum during laparoscopic hysterectomy. Acta Anaesthesiol Scand. 1995; 39:949–55. DOI: 10.1111/j.1399-6576.1995.tb04203.x. PMID: 8848897.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of the Effects of Propofol and Sevoflurane Anesthesias on Intraocular Pressure during Laparoscopic Hysterectomy
- The Effect of Cardiovascular and Arterial Blood Gas Changes during Laparoscope Assisted Vaginal Hysterectomy (LAVH)
- The effect of Trendelenburg position and pneumoperitoneum on regional cerebral oxygen saturation during gynecological laparoscopic surgery
- A Case Report of Brachial Plexus Palsy after Laparascopy Assisted Vaginal Hysterectomy
- Comparison of the effects of normal and low blood pressure regulation on the optic nerve sheath diameter in robot assisted laparoscopic radical prostatectomy