Anesth Pain Med.
2021 Jul;16(3):248-257. 10.17085/apm.20097.
Comparison of the effects of normal and low blood pressure regulation on the optic nerve sheath diameter in robot assisted laparoscopic radical prostatectomy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Keimyung University Dongsan Hospital, Daegu, Korea
- KMID: 2519053
- DOI: http://doi.org/10.17085/apm.20097
Abstract
- Background
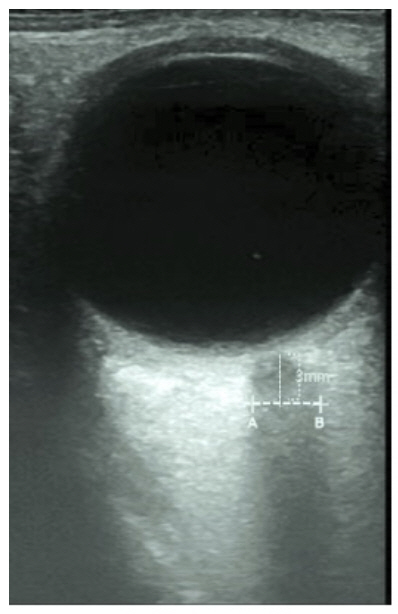
Robot-assisted laparoscopic radical prostatectomy is an advanced and popular surgical technique. However, increased intracranial pressure which is caused by CO2 pneumoperitoneum and Trendelenburg position is the main cerebrovascular effect. Measurement of optic nerve sheath diameter using ocular ultrasound is a noninvasive and reliable method for the assessment of intracranial pressure. The primary endpoint of this study was to identify whether low blood pressure regulation has any benefit in attenuating an increase of optic nerve sheath diameter during robot-assisted laparoscopic radical prostatectomy.
Methods
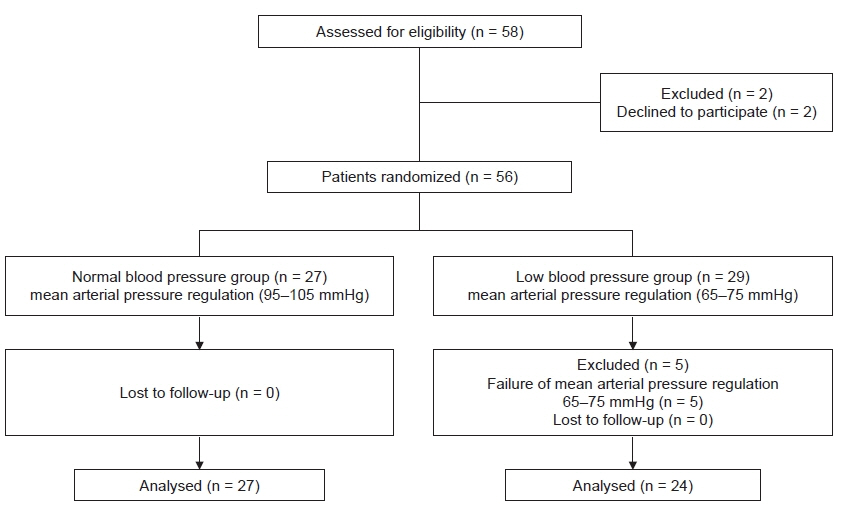
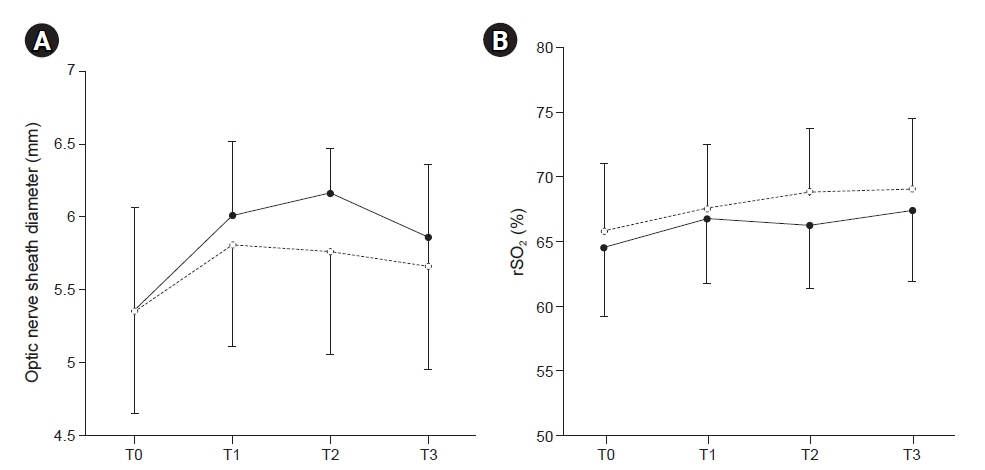
Optic nerve sheath diameter and cerebral oxygen saturation were measured at baseline (supine position), one and two hours after pneumoperitoneum and Trendelenburg position respectively, and after return to supine position in normal (n = 27) and low blood pressure groups (n = 24).
Results
Mean optic nerve sheath diameter values measured at one and two hours after pneumoperitoneum and Trendelenburg position were significantly increased compared to the baseline value (P < 0.001 in normal blood pressure group; P = 0.003 in low blood pressure group). However, the mean optic nerve sheath diameter and cerebral oxygen saturation measured at any of the time points as well as degrees of change between the two groups did not show any significant changes. The peak values of optic nerve sheath diameter in normal and low blood pressure groups demonstrated 14.9% and 9.2% increases, respectively.
Conclusions
Low blood pressure group demonstrated an effect in maintaining an increase of optic nerve sheath diameter less than 10% during CO2 pneumoperitoneum and Trendelenburg position.
Keyword
Figure
Reference
-
1. Kim MS, Bai SJ, Lee JR, Choi YD, Kim YJ, Choi SH. Increase in intracranial pressure during carbon dioxide pneumoperitoneum with steep trendelenburg positioning proven by ultrasonographic measurement of optic nerve sheath diameter. J Endourol. 2014; 28:801–6.2. Whiteley JR, Taylor J, Henry M, Epperson TI, Hand WR. Detection of elevated intracranial pressure in robot-assisted laparoscopic radical prostatectomy using ultrasonography of optic nerve sheath diameter. J Neurosurg Anesthesiol. 2015; 27:155–9.3. Choi ES, Jeon YT, Sohn HM, Kim DW, Choi SJ, In CB. Comparison of the effects of desflurane and total intravenous anesthesia on the optic nerve sheath diameter in robot assisted laparoscopic radical prostatectomy: a randomized controlled trial. Medicine (Baltimore). 2018; 97:e12772.4. You AH, Song Y, Kim DH, Suh J, Baek JW, Han DW. Effects of positive end-expiratory pressure on intraocular pressure and optic nerve sheath diameter in robot-assisted laparoscopic radical prostatectomy: a randomized, clinical trial. Medicine (Baltimore). 2019; 98:e15051.5. Kim Y, Choi S, Kang S, Park B. Propofol affects optic nerve sheath diameter less than sevoflurane during robotic surgery in the steep trendelenburg position. Biomed Res Int. 2019; 2019:5617815.6. Robba C, Santori G, Czosnyka M, Corradi F, Bragazzi N, Padayachy L, et al. Optic nerve sheath diameter measured sonographically as non-invasive estimator of intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2018; 44:1284–94.7. Robba C, Bacigaluppi S, Cardim D, Donnelly J, Bertuccio A, Czosnyka M. Non-invasive assessment of intracranial pressure. Acta Neurol Scand. 2016; 134:4–21.8. Robba C, Cardim D, Tajsic T, Pietersen J, Bulman M, Donnelly J, et al. Ultrasound non-invasive measurement of intracranial pressure in neurointensive care: a prospective observational study. PLoS Med. 2017; 14:e1002356.9. Ali MA, Hashmi M, Shamim S, Salam B, Siraj S, Salim B. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure through an external ventricular drain. Cureus. 2019; 11:e5777.10. Ozturk Z, Atalay T, Arhan E, Aydin K, Serdaroglu A, Hirfanoglu T, et al. The efficacy of orbital ultrasonography and magnetic resonance imaging findings with direct measurement of intracranial pressure in distinguishing papilledema from pseudopapilledema. Childs Nerv Syst. 2017; 33:1501–7.11. Dubost C, Le Gouez A, Jouffroy V, Roger-Christoph S, Benhamou D, Mercier FJ, et al. Optic nerve sheath diameter used as ultrasonographic assessment of the incidence of raised intracranial pressure in preeclampsia: a pilot study. Anesthesiology. 2012; 116:1066–71.12. Lee SU, Jeon JP, Lee H, Han JH, Seo M, Byoun HS, et al. Optic nerve sheath diameter threshold by ocular ultrasonography for detection of increased intracranial pressure in Korean adult patients with brain lesions. Medicine (Baltimore). 2016; 95:e5061.13. Lee B, Koo BN, Choi YS, Kil HK, Kim MS, Lee JH. Effect of caudal block using different volumes of local anaesthetic on optic nerve sheath diameter in children: a prospective, randomized trial. Br J Anaesth. 2017; 118:781–7.14. Padayachy LC, Padayachy V, Galal U, Gray R, Fieggen AG. The relationship between transorbital ultrasound measurement of the optic nerve sheath diameter (ONSD) and invasively measured ICP in children: part I: repeatability, observer variability and general analysis. Childs Nerv Syst. 2016; 32:1769–78.15. Cimilli Ozturk T, Demir H, Yorulmaz R, Ozdemir S, Isat G, Ecmel Onur O. Assessment of intra-interobserver reliability of the sonographic optic nerve sheath diameter measurement. Kaohsiung J Med Sci. 2015; 31:432–6.16. Matsuoka T, Ishiyama T, Shintani N, Kotoda M, Mitsui K, Matsukawa T. Changes of cerebral regional oxygen saturation during pneumoperitoneum and Trendelenburg position under propofol anesthesia: a prospective observational study. BMC Anesthesiol. 2019; 19:72.17. Hong JH, Jung SW, Park JH. The effect of speed of normal saline injection on optic nerve sheath diameter in thoracic epidural anesthesia. Pain Physician. 2019; 22:E325–32.18. Moretti R, Pizzi B. Ultrasonography of the optic nerve in neurocritically ill patients. Acta Anaesthesiol Scand. 2011; 55:644–52.19. Yin G, Wang YX, Zheng ZY, Yang H, Xu L, Jonas JB; Beijing Eye Study Group. Ocular axial length and its associations in Chinese: the Beijing eye study. PLoS One. 2012; 7:e43172.20. Choi SH, Lee SJ, Rha KH, Shin SK, Oh YJ. The effect of pneumoperitoneum and Trendelenburg position on acute cerebral blood flow-carbon dioxide reactivity under sevoflurane anaesthesia. Anaesthesia. 2008; 63:1314–8.21. Wilson MH. Monro-Kellie 2.0: the dynamic vascular and venous pathophysiological components of intracranial pressure. J Cereb Blood Flow Metab. 2016; 36:1338–50.22. Tanaka N, Yamamoto M, Abe T, Osawa T, Matsumoto R, Shinohara N, et al. Changes of cerebral blood volume during robot-assisted laparoscopic radical prostatectomy: observational prospective study using near-infrared time-resolved spectroscopy. J Endourol. 2019; 33:995–1001.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Robot-Assisted Laparoscopic Radical Prostatectomy
- A Case of Robot-Assisted Laparoscopic Radical Prostatectomy in Primary Small Cell Prostate Cancer
- Robot-Assisted Laparoscopic Radical Prostatectomy
- Robot-Assisted Laparoscopic Radical Prostatectomy: Four Cases
- Floating Hem-o-Lok Clips in the Bladder without Stone Formation after Robot-Assisted Laparoscopic Radical Prostatectomy