J Korean Ophthalmol Soc.
2016 Nov;57(11):1817-1820. 10.3341/jkos.2016.57.11.1817.
A Case of Migraine with Aura Related to the Percutaneous Closure of Atrial Septal Defect
- Affiliations
-
- 1Department of Ophthalmology, Chung-Ang University College of Medicine, Seoul, Korea. yschun100@hanmail.net
- 2Department of Cardiology, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2357743
- DOI: http://doi.org/10.3341/jkos.2016.57.11.1817
Abstract
- PURPOSE
To report a case of migraine attacks with aura that occurred after percutaneous closure of an atrial septal defect (ASD) with the Amplatzer septal occluder device.
CASE SUMMARY
A 58-year-old female presented with glare and scintillation that lasted 3 days. She had a history of percutaneous ASD intervention 3 weeks prior. Because ophthalmologic examination revealed nothing remarkable, the patient underwent observation. However, two months later, she revisited our department, presenting with aggravated glare, scintillation, and severe photophobia. Also, she presented with scintillation followed by a headache starting from the right temporal area extending to the occipital area. The patient was diagnosed with migraine with aura, which was newly developed after percutaneous ASD closure. After switching medication from acetylsalicylic acid to clopidogrel, the frequency and intensity of the headaches were reduced. No recurrence of ophthalmic symptoms or headache was observed during the 1-year follow-up.
CONCLUSIONS
Percutaneous closure of ASD can be complicated by the appearance of migraine attacks with aura. When patients present with glare and scintillation, ophthalmologists must consider the possibility of migraine with aura and migraine induced by secondary causes. Thus, detailed history taking should be taken in order to make an early diagnosis of migraine.
Keyword
MeSH Terms
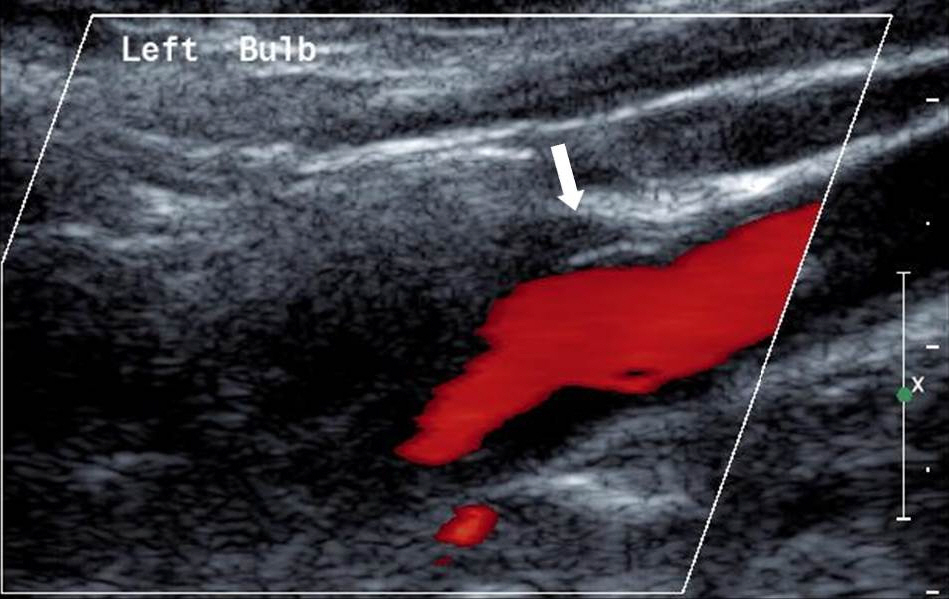
Figure
Reference
-
References
1. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013; 33:629–808.2. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380:2163–96.3. Roh JK, Kim JS, Ahn YO. Epidemiological and clinical abdominal of migraine in Korea. J Korean Neurol Assoc. 1997; 15:1–18.4. Dafer RM, Jay WM. Headache and the eye. Curr Opin Ophthalmol. 2009; 20:520–4.
Article5. Flammer J, Konieczka K, Flammer AJ. The primary vascular abdominal syndrome: implications for eye diseases. EPMA J. 2013; 4:14.6. Gramer G, Weber BH, Gramer E. Migraine and vasospasm in abdominal: age-related evaluation of 2027 patients with glaucoma or abdominal hypertension. Invest Ophthalmol Vis Sci. 2015; 56:7999–8007.7. Queiroz LP, Friedman DI, Rapoport AM, Purdy RA. Characteristics of migraine visual aura in Southern Brazil and Northern USA. Cephalalgia. 2011; 31:1652–8.
Article8. Koh JS, Kim SJ. Clinical features of patients complaining of visual symptoms and diagnosed with migraine. J Korean Ophthalmol Soc. 2015; 56:1933–8.
Article9. Fernández-Mayoralas DM, Fernández-Jaén A, Muñoz-Jareño N, et al. Migraine symptoms related to the percutaneous closure of an ostium secundum atrial septal defect: report of four paediatric abdominal and review of the literature. Cephalalgia. 2007; 27:550–6.10. Rodés-Cabau J, Molina C, Serrano-Munuera C, et al. Migraine with aura related to the percutaneous closure of an atrial septal defect. Catheter Cardiovasc Interv. 2003; 60:540–2.
Article11. Sztajzel R, Genoud D, Roth S, et al. Patent foramen ovale, a abdominal cause of symptomatic migraine: a study of 74 patients with acute ischemic stroke. Cerebrovasc Dis. 2002; 13:102–6.12. Rodés-Cabau J, Mineau S, Marrero A, et al. Incidence, timing, and predictive factors of new-onset migraine headache attack after transcatheter closure of atrial septal defect or patent foramen ovale. Am J Cardiol. 2008; 101:688–92.
Article13. Kato Y, Kobayashi T, Ishido H, et al. Migraine attacks after abdominal closure of atrial septal defect. Cephalalgia. 2013; 33:1229–37.14. Luermans JG, Post MC, Temmerman F, et al. Is a predominant left-to-right shunt associated with migraine?: A prospective atrial septal defect closure study. Catheter Cardiovasc Interv. 2009; 74:1078–84.
Article15. Kato Y, Hayashi T, Kobayashi T, Tanahashi N. Migraine prevalence in patients with atrial septal defect. J Headache Pain. 2013; 14:63.
Article16. Burstein R, Noseda R, Borsook D. Migraine: multiple processes, complex pathophysiology. J Neurosci. 2015; 35:6619–29.
Article17. Wilmshurst PT, Nightingale S, Walsh KP, et al. Clopidogrel reduces migraine with aura after transcatheter closure of persistent foramen ovale and atrial septal defects. Heart. 2005; 91:1173–5.
Article18. Ferrari J, Baumgartner H, Tentschert S, et al. Cerebral micro-embolism during transcatheter closure of patent foramen ovale. J Neurol. 2004; 251:825–9.
Article19. Wertman B, Azarbal B, Riedl M, Tobis J. Adverse events associated with nickel allergy in patients undergoing percutaneous atrial abdominal defect or patent foramen ovale closure. J Am Coll Cardiol. 2006; 47:1226–7.20. Aiba S, Tatsumoto M, Saisu A, et al. Prevalence of typical migraine aura without headache in Japanese ophthalmology clinics. Cephalalgia. 2010; 30:962–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subacute, Silent Embolization of Amplatzer Atrial Septal Defect Closure Device to the Pulmonary Artery
- Surgical Extraction of an Embolized Atrial Septal Defect Occluder Device into Pulmonary Artery after Percutaneous Closure
- Emergent Surgical Intervention for Embolization of Atrial Septal Defect Closure Device
- Fistula of Ascending Aorta and Right Atrium Following Percutaneous Transcatheter Atrial Septal Defect Closure
- Procedural, Early and Long-term Outcomes after Percutaneous Closure of Atrial Septal Defect: Comparison between Large and Very Large Atrial Septal Defect Groups