Ann Rehabil Med.
2016 Aug;40(4):675-681. 10.5535/arm.2016.40.4.675.
Length of Hospital Stay After Stroke: A Korean Nationwide Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul, Korea. hyungik1@snu.ac.kr
- 2Department of Neurology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Physical Medicine and Rehabilitation, Korea University Anam Hospital, Seoul, Korea.
- KMID: 2356653
- DOI: http://doi.org/10.5535/arm.2016.40.4.675
Abstract
OBJECTIVE
To investigate the length of hospital stay (LOS) after stroke using the database of the Korean Health Insurance Review & Assessment Service.
METHODS
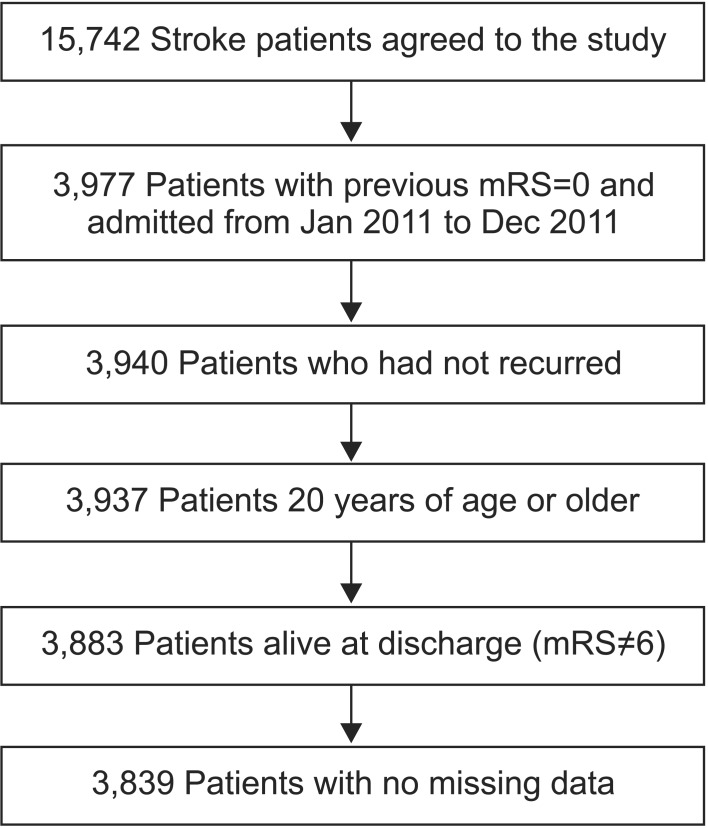
We matched the data of patients admitted for ischemic stroke onset within 7 days in the Departments of Neurology of 12 hospitals to the data from the database of the Korean Health Insurance Review & Assessment Service. We recruited 3,839 patients who were hospitalized between January 2011 and December 2011, had a previous modified Rankin Scale of 0, and no acute hospital readmission after discharge. The patients were divided according to the initial National Institute of Health Stroke Scale score (mild, ≤5; moderate, >5 and ≤13; severe, >13); we compared the number of hospitals that admitted patients and LOS after stroke according to severity, age, and sex.
RESULTS
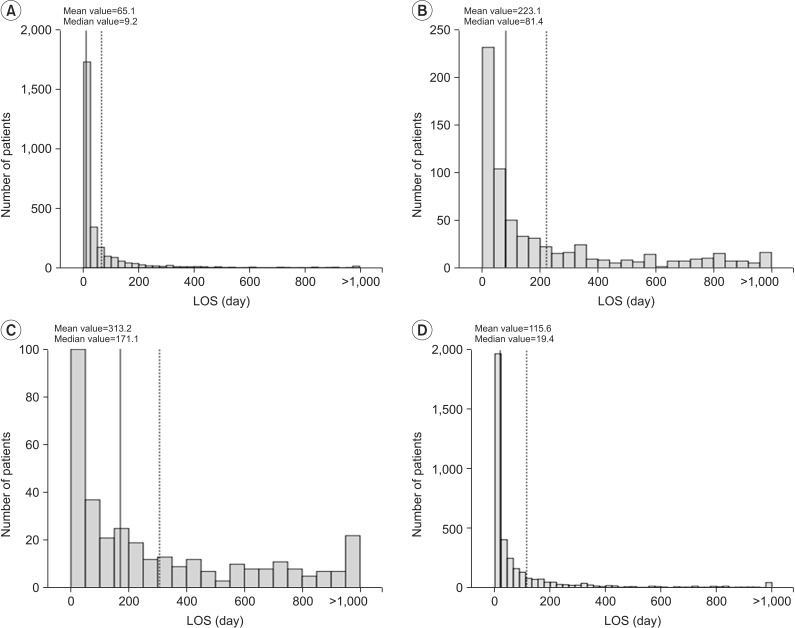
The mean LOS was 115.6±219.0 days (median, 19.4 days) and the mean number of hospitals was 3.3±2.1 (median, 2.0). LOS was longer in patients with severe stroke (mild, 65.1±146.7 days; moderate, 223.1±286.0 days; and severe, 313.2±336.8 days). The number of admitting hospitals was greater for severe stroke (mild, 2.9±1.7; moderate, 4.3±2.6; and severe, 4.5±2.4). LOS was longer in women and shorter in patients less than 65 years of age.
CONCLUSION
LOS after stroke differed according to the stroke severity, sex, and age. These results will be useful in determining the appropriate LOS after stroke in the Korean medical system.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Medical rehabilitation system for patients in acute rehabilitation units
Seung Don Yoo, Yong Seol Jeong, Tae-Woo Kim
J Korean Med Assoc. 2017;60(11):864-869. doi: 10.5124/jkma.2017.60.11.864.An Erratum to Correct Typographical Errors
Ann Rehabil Med. 2016;40(5):959-959. doi: 10.5535/arm.2016.40.5.959.Status of Rehabilitation After Ischemic Stroke: A Korean Nationwide Study
Won-Sep Kim, Hee-Joon Bae, Hyun-Haeng Lee, Hyung Ik Shin
Ann Rehabil Med. 2018;42(4):528-535. doi: 10.5535/arm.2018.42.4.528.
Reference
-
1. Rhie KS, Rah UW, Lee IY, Yim SY, Kim KM, Moon DJ, et al. The discharge destination of rehabilitation inpatients in a tertiary hospital. J Korean Acad Rehabil Med. 2005; 29:135–140.2. Kang EK, Kim WS, Jeong SH, Shin HI, Han TR. Desire for rehabilitation services of stroke patients admitted in post-acute rehabilitation facilities. J Korean Acad Rehabil Med. 2007; 31:404–409.3. Jung SH, Lee KM, Park SW, Chun MH, Jung HY, Kim IS, et al. Inpatient course and length of hospital stay in patients with brain disorders in South Korea: a population-based registry study. Ann Rehabil Med. 2012; 36:609–617. PMID: 23185724.
Article4. Appelros P. Prediction of length of stay for stroke patients. Acta Neurol Scand. 2007; 116:15–19. PMID: 17587250.
Article5. Chang KC, Tseng MC, Weng HH, Lin YH, Liou CW, Tan TY. Prediction of length of stay of first-ever ischemic stroke. Stroke. 2002; 33:2670–2674. PMID: 12411659.
Article6. Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS. Acute stroke care and rehabilitation: an analysis of the direct cost and its clinical and social determinants. The Copenhagen Stroke Study. Stroke. 1997; 28:1138–1141. PMID: 9183339.7. Schlegel D, Kolb SJ, Luciano JM, Tovar JM, Cucchiara BL, Liebeskind DS, et al. Utility of the NIH Stroke Scale as a predictor of hospital disposition. Stroke. 2003; 34:134–137. PMID: 12511764.
Article8. Zizza CA, Ellison KJ, Wernette CM. Total water intakes of community-living middle-old and oldest-old adults. J Gerontol A Biol Sci Med Sci. 2009; 64:481–486. PMID: 19213852.
Article9. Saxena SK, Koh GC, Ng TP, Fong NP, Yong D. Determinants of length of stay during post-stroke rehabilitation in community hospitals. Singapore Med J. 2007; 48:400–407. PMID: 17453097.10. Tan WS, Heng BH, Chua KS, Chan KF. Factors predicting inpatient rehabilitation length of stay of acute stroke patients in Singapore. Arch Phys Med Rehabil. 2009; 90:1202–1207. PMID: 19577034.
Article11. Svendsen ML, Ehlers LH, Andersen G, Johnsen SP. Quality of care and length of hospital stay among patients with stroke. Med Care. 2009; 47:575–582. PMID: 19365293.
Article12. Miyai I, Sonoda S, Nagai S, Takayama Y, Inoue Y, Kakehi A, et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair. 2011; 25:540–547. PMID: 21451116.
Article13. van Straten A, van der Meulen JH, van den Bos GA, Limburg M. Length of hospital stay and discharge delays in stroke patients. Stroke. 1997; 28:137–140. PMID: 8996502.
Article14. Hakim EA, Bakheit AM. A study of the factors which influence the length of hospital stay of stroke patients. Clin Rehabil. 1998; 12:151–156. PMID: 9619657.
Article15. Granger CV, Reistetter TA, Graham JE, Deutsch A, Markello SJ, Niewczyk P, et al. The Uniform Data System for Medical Rehabilitation: report of patients with hip fracture discharged from comprehensive medical programs in 2000-2007. Am J Phys Med Rehabil. 2011; 90:177–189. PMID: 21297397.16. Kim JS, Lee EH. Cultural and noncultural predictors of health outcomes in Korean daughter and daughter-in-law caregivers. Public Health Nurs. 2003; 20:111–119. PMID: 12588428.
Article17. Feigenson JS, McDowell FH, Meese P, McCarthy ML, Greenberg SD. Factors influencing outcome and length of stay in a stroke rehabilitation unit. Part 1. Analysis of 248 unscreened patients: medical and functional prognostic indicators. Stroke. 1977; 8:651–656. PMID: 929650.18. Monane M, Kanter DS, Glynn RJ, Avorn J. Variability in length of hospitalization for stroke. The role of managed care in an elderly population. Arch Neurol. 1996; 53:875–880. PMID: 8815852.19. Saxena SK, Ng TP, Yong D, Fong NP, Gerald K. Total direct cost, length of hospital stay, institutional discharges and their determinants from rehabilitation settings in stroke patients. Acta Neurol Scand. 2006; 114:307–314. PMID: 17022777.
Article20. Turner-Stokes L, Sutch S, Dredge R. Healthcare tariffs for specialist inpatient neurorehabilitation services: rationale and development of a UK casemix and costing methodology. Clin Rehabil. 2012; 26:264–279. PMID: 21971751.
Article21. Turner-Stokes L, Scott H, Williams H, Siegert R. The Rehabilitation Complexity Scale: extended version. Detection of patients with highly complex needs. Disabil Rehabil. 2012; 34:715–720. PMID: 22115200.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association Between Length of Stay in the Intensive Care Unit and Sarcopenia Among Hemiplegic Stroke Patients
- The Effect of Complications of Stroke Patients on Prognosis during Rehabilitation Management
- Effects of Full-Time Integrated Self Upper-Extremity Training Program on Functional Recovery and Length of Stay in Stroke Patients
- Neurologic Complications of Extracorporeal Membrane Oxygenation
- The Determinants of Length of Stay in a University Hospital