J Clin Neurol.
2015 Oct;11(4):383-389. 10.3988/jcn.2015.11.4.383.
Neurologic Complications of Extracorporeal Membrane Oxygenation
- Affiliations
-
- 1Department of Neurology, Mayo Clinic, Rochester, MN, USA. nasr.deena@mayo.edu
- KMID: 2179759
- DOI: http://doi.org/10.3988/jcn.2015.11.4.383
Abstract
- BACKGROUND AND PURPOSE
The rate and outcomes of neurologic complications of patients receiving extracorporeal membrane oxygenation (ECMO) are poorly understood. The purpose of this study was to identify these parameters in ECMO patients.
METHODS
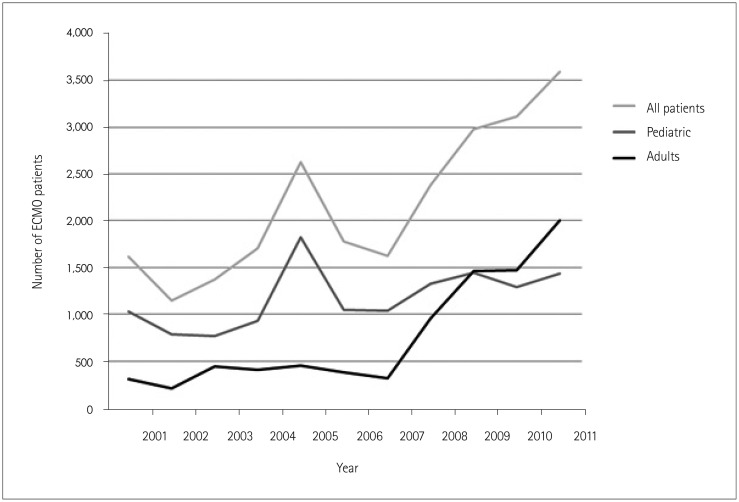
All patients receiving ECMO were selected from the Nationwide Inpatient Sample between 2001-2011. The rate and outcomes of neurologic complications [acute ischemic stroke, intracranial hemorrhage (ICH), and seizures] among these patients was determined. Discharge status, mortality, length of stay, and hospitalization costs were compared between patients with and without neurologic complications using chi-squared tests for categorical variables and Student's t-test for continuous variables.
RESULTS
In total, 23,951 patients were included in this study, of which 2,604 (10.9%) suffered neurologic complications of seizure (4.1%), stroke (4.1%), or ICH (3.6%). When compared to patients without neurologic complications, acute ischemic stroke patients had significantly higher rates of discharge to a long-term facility (12.2% vs. 6.8%, p<0.0001) and a significantly longer mean length of stay (41.6 days vs. 31.9 days, p<0.0001). ICH patients had significantly higher rates of discharge to a long-term facility (9.5% vs. 6.8%, p=0.007), significantly higher mortality rates (59.7% vs. 50.0%, p<0.0001), and a significantly longer mean length of stay (41.8 days vs. 31.9 days) compared to patients without neurologic complications. These outcomes did not differ significantly between seizure patients and patients without neurologic complications.
CONCLUSIONS
Given the increasing utilization of ECMO and the high costs and poor outcomes associated with neurologic complications, more research is needed to help determine the best way to prevent these sequelae in this patient population.
Keyword
MeSH Terms
Figure
Reference
-
1. Marasco SF, Lukas G, McDonald M, McMillan J, Ihle B. Review of ECMO (extra corporeal membrane oxygenation) support in critically ill adult patients. Heart Lung Circ. 2008; 17(Suppl 4):S41–S47. PMID: 18964254.2. Bulas DI, Taylor GA, O'Donnell RM, Short BL, Fitz CR, Vezina G. Intracranial abnormalities in infants treated with extracorporeal membrane oxygenation: update on sonographic and CT findings. AJNR Am J Neuroradiol. 1996; 17:287–294. PMID: 8938301.3. Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators. Davies A, Jones D, Bailey M, Beca J, Bellomo R, et al. Extracorporeal Membrane Oxygenation for 2009 Influenza A(H1N1) Acute Respiratory Distress Syndrome. JAMA. 2009; 302:1888–1895. PMID: 19822628.4. Mateen FJ, Muralidharan R, Shinohara RT, Parisi JE, Schears GJ, Wijdicks EF. Neurological injury in adults treated with extracorporeal membrane oxygenation. Arch Neurol. 2011; 68:1543–1549. PMID: 21825216.5. Graziani LJ, Gringlas M, Baumgart S. Cerebrovascular complications and neurodevelopmental sequelae of neonatal ECMO. Clin Perinatol. 1997; 24:655–675. PMID: 9394865.6. Risnes I, Wagner K, Nome T, Sundet K, Jensen J, Hynås IA, et al. Cerebral outcome in adult patients treated with extracorporeal membrane oxygenation. Ann Thorac Surg. 2006; 81:1401–1406. PMID: 16564280.7. Cardarelli MG, Young AJ, Griffith B. Use of extracorporeal membrane oxygenation for adults in cardiac arrest (E-CPR): a meta-analysis of observational studies. ASAIO J. 2009; 55:581–586. PMID: 19770800.8. Paden ML, Conrad SA, Rycus PT, Thiagarajan RR. ELSO Registry. Extracorporeal Life Support Organization Registry Report 2012. ASAIO J. 2013; 59:202–210. PMID: 23644605.9. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383. PMID: 3558716.10. Lan C, Tsai PR, Chen YS, Ko WJ. Prognostic factors for adult patients receiving extracorporeal membrane oxygenation as mechanical circulatory support--a 14-year experience at a medical center. Artif Organs. 2010; 34:E59–E64. PMID: 20420591.11. Liebeskind DS, Sanossian N, Sapo ML, Saver JL. Cerebral microbleeds after use of extracorporeal membrane oxygenation in children. J Neuroimaging. 2013; 23:75–78. PMID: 22606942.12. Fischer S, Bohn D, Rycus P, Pierre AF, de Perrot M, Waddell TK, et al. Extracorporeal membrane oxygenation for primary graft dysfunction after lung transplantation: analysis of the Extracorporeal Life Support Organization (ELSO) registry. J Heart Lung Transplant. 2007; 26:472–477. PMID: 17449416.13. Li J, Long C, Lou S, Hei F, Yu K, Wang S, et al. Venoarterial extracorporeal membrane oxygenation in adult patients: predictors of mortality. Perfusion. 2009; 24:225–230. PMID: 19808747.14. Massetti M, Tasle M, Le Page O, Deredec R, Babatasi G, Buklas D, et al. Back from irreversibility: extracorporeal life support for prolonged cardiac arrest. Ann Thorac Surg. 2005; 79:178–183. discussion 183-184PMID: 15620939.15. Cheng R, Hachamovitch R, Kittleson M, Patel J, Arabia F, Moriguchi J, et al. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: a meta-analysis of 1,866 adult patients. Ann Thorac Surg. 2014; 97:610–616. PMID: 24210621.16. Rehder KJ, Turner DA, Cheifetz IM. Extracorporeal membrane oxygenation for neonatal and pediatric respiratory failure: an evidence-based review of the past decade (2002-2012). Pediatr Crit Care Med. 2013; 14:851–861. PMID: 24108118.17. Cengiz P, Seidel K, Rycus PT, Brogan TV, Roberts JS. Central nervous system complications during pediatric extracorporeal life support: incidence and risk factors. Crit Care Med. 2005; 33:2817–2824. PMID: 16352965.18. Hervey-Jumper SL, Annich GM, Yancon AR, Garton HJ, Muraszko KM, Maher CO. Neurological complications of extracorporeal membrane oxygenation in children. J Neurosurg Pediatr. 2011; 7:338–344. PMID: 21456903.19. Kugelman A, Gangitano E, Pincros J, Tantivit P, Taschuk R, Durand M. Venovenous versus venoarterial extracorporeal membrane oxygenation in congenital diaphragmatic hernia. J Pediatr Surg. 2003; 38:1131–1136. PMID: 12891480.20. Rais-Bahrami K, Van Meurs KP. Venoarterial versus venovenous ECMO for neonatal respiratory failure. Semin Perinatol. 2014; 38:71–77. PMID: 24580762.21. Zahraa JN, Moler FW, Annich GM, Maxvold NJ, Bartlett RH, Custer JR. Venovenous versus venoarterial extracorporeal life support for pediatric respiratory failure: are there differences in survival and acute complications? Crit Care Med. 2000; 28:521–525. PMID: 10708194.22. Lazar EL, Abramson SJ, Weinstein S, Stolar CJ. Neuroimaging of brain injury in neonates treated with extracorporeal membrane oxygenation: lessons learned from serial examinations. J Pediatr Surg. 1994; 29:186–190. discussion 190-191PMID: 8176589.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Retrieval of a Fractured Guidewire during Extracorporeal Membrane Oxygenator Insertion
- Intracranial Hemorrhage Identified in the Early Stage after Applying Extracorporeal Membrane Oxygenation to Support Cardiopulmonary Resuscitation
- A case of rescuing a patient with acute cardiovascular instability from sudden and massive intraoperative pulmonary thromboembolism by extracorporeal membrane oxygenation
- Extracorporeal Membrane Oxygenation for Complicated Scrub Typhus
- Use of amplitude-integrated electroencephalography in decision-making for extracorporeal membrane oxygenation in comatose cardiac arrest patients whose eventual neurologic recovery is uncertain