Ann Rehabil Med.
2021 Feb;45(1):49-56. 10.5535/arm.20111.
Association Between Length of Stay in the Intensive Care Unit and Sarcopenia Among Hemiplegic Stroke Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 2Department of Rehabilitation Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2513230
- DOI: http://doi.org/10.5535/arm.20111
Abstract
Objective
To discuss the association between the length of stay at the intensive care unit (ICU) and sarcopenia among hemiplegic stroke patients.
Methods
This study evaluated 66 hemiplegic stroke patients with history of ICU admission using handgrip strength and bioelectrical impedance analysis to obtain height-adjusted appendicular skeletal muscle mass. The diagnosis of sarcopenia was made according to the muscle mass based on the Asian Working Group for Sarcopenia. The patients were divided into sarcopenic and non-sarcopenic groups. The two groups were statistically analyzed, and the significant factors with differences were studied. A multivariate logistic regression analysis was performed to examine the association between length of stay in the ICU and sarcopenia, after adjusting for potential confounders.
Results
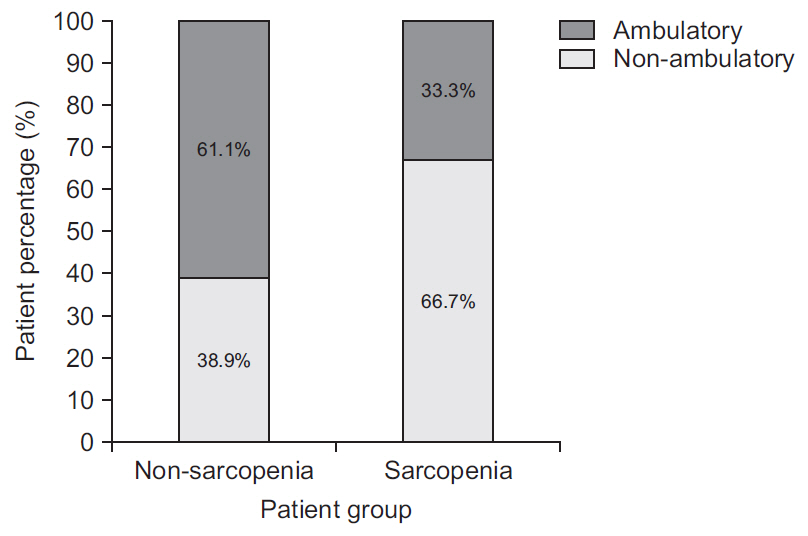
Among 66 hemiplegic patients with an ICU admission history, 12 patients were diagnosed with sarcopenia. Sarcopenia patients showed lower scores on the Korean version of the Modified Barthel Index and the Korean version of the Mini-Mental State Examination. Additionally, patients with sarcopenia had a longer length of stay in the ICU, and univariate and multivariate analyses confirmed that the ICU length of stay was significantly related to sarcopenia (adjusted odds ratio=1.187; 95% confidence interval, 1.019–1.382; p=0.028).
Conclusion
The length of stay in the ICU was significantly associated with sarcopenia in hemiplegic stroke patients.
Figure
Cited by 2 articles
-
Handgrip Strength: An Irreplaceable Indicator of Muscle Function
Sang Yoon Lee
Ann Rehabil Med. 2021;45(3):167-169. doi: 10.5535/arm.21106.Trunk Impairment Scale for Predicting Lumbar Spine Bone Mineral Density in Young Male Patients With Subacute Stroke
Yeon Hee Cho, Hyun Seok, Sang-Hyun Kim, Seung Yeol Lee, Hyun Jung Kim
Ann Rehabil Med. 2023;47(2):98-107. doi: 10.5535/arm.23005.
Reference
-
1. Fearon KC. Cancer cachexia and fat-muscle physiology. N Engl J Med. 2011; 365:565–7.
Article2. Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. J Am Med Dir Assoc. 2011; 12:249–56.3. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:16–31.
Article4. Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997; 127(5 Suppl):990S–991S.
Article5. Bianchi L, Ferrucci L, Cherubini A, Maggio M, Bandinelli S, Savino E, et al. The predictive value of the EWGSOP definition of sarcopenia: results from the InCHIANTI Study. J Gerontol A Biol Sci Med Sci. 2016; 71:259–64.
Article6. Shiraishi A, Yoshimura Y, Wakabayashi H, Tsuji Y. Prevalence of stroke-related sarcopenia and its association with poor oral status in post-acute stroke patients: implications for oral sarcopenia. Clin Nutr. 2018; 37:204–7.
Article7. Scherbakov N, von Haehling S, Anker SD, Dirnagl U, Doehner W. Stroke induced sarcopenia: muscle wasting and disability after stroke. Int J Cardiol. 2013; 170:89–94.
Article8. Fanshawe M, Venkatesh B, Boots RJ. Outcome of stroke patients admitted to intensive care: experience from an Australian teaching hospital. Anaesth Intensive Care. 2002; 30:628–32.
Article9. Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, et al. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019; 6:233–46.
Article10. Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020; 21:300–7.
Article11. Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011; 40:423–9.
Article12. Gonzalez MC, Heymsfield SB. Bioelectrical impedance analysis for diagnosing sarcopenia and cachexia: what are we really estimating? J Cachexia Sarcopenia Muscle. 2017; 8:187–9.
Article13. Kim SJ, Yu EH, Min JH, Shin YI, Ko HY, Ko SH. Segmental bioelectrical impedance analysis of the body composition of affected and unaffected limbs after hemiparetic stroke. Am J Phys Med Rehabil. 2020; 99:830–6.14. Kim DY, Kim YH, Lee J, Chang WH, Kim MW, Pyun SB, et al. Clinical practice guideline for stroke rehabilitation in Korea 2016. Brain Neurorehabil. 2017; 10(Suppl 1):e11.15. Stroke Unit Trialists’ Collaboration. Organised inpatient (stroke unit) care for stroke [Internet]. London, UK: Cochrane Library;2013. [cited 2020 Dec 28]. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000197.pub3/full.16. Hachisuka K, Umezu Y, Ogata H. Disuse muscle atrophy of lower limbs in hemiplegic patients. Arch Phys Med Rehabil. 1997; 78:13–8.
Article17. Hunnicutt JL, Gregory CM. Skeletal muscle changes following stroke: a systematic review and comparison to healthy individuals. Top Stroke Rehabil. 2017; 24:463–71.
Article18. De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, et al. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002; 288:2859–67.19. Schefold JC, Bierbrauer J, Weber-Carstens S. Intensive care unit-acquired weakness (ICUAW) and muscle wasting in critically ill patients with severe sepsis and septic shock. J Cachexia Sarcopenia Muscle. 2010; 1:147–57.
Article20. Akahoshi T, Yasuda M, Momii K, Kubota K, Shono Y, Kaku N, et al. Sarcopenia is a predictive factor for prolonged intensive care unit stays in high-energy blunt trauma patients. Acute Med Surg. 2016; 3:326–31.
Article21. Vahlberg B, Lindmark B, Zetterberg L, Hellstrom K, Cederholm T. Body composition and physical function after progressive resistance and balance training among older adults after stroke: an exploratory randomized controlled trial. Disabil Rehabil. 2017; 39:1207–14.
Article22. Chang KV, Wu WT, Huang KC, Han DS. Segmental body composition transitions in stroke patients:trunks are different from extremities and strokes are as important as hemiparesis. Clin Nutr. 2020; 39:1968–73.23. Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012; 40:502–9.24. Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017; 43:171–83.
Article25. Griffiths RD, Palmer TE, Helliwell T, MacLennan P, MacMillan RR. Effect of passive stretching on the wasting of muscle in the critically ill. Nutrition. 1995; 11:428–32.
Article26. Gerovasili V, Stefanidis K, Vitzilaios K, Karatzanos E, Politis P, Koroneos A, et al. Electrical muscle stimulation preserves the muscle mass of critically ill patients: a randomized study. Crit Care. 2009; 13:R161.
Article27. Hwang F, McGreevy CM, Pentakota SR, Verde D, Park JH, Berlin A, et al. Sarcopenia is predictive of functional outcomes in older trauma patients. Cureus. 2019; 11:e6154.
Article28. Jung HJ, Lee YM, Kim M, Uhm KE, Lee J. Suggested assessments for sarcopenia in patients with stroke who can walk independently. Ann Rehabil Med. 2020; 44:20–37.
Article29. Ha L, Hauge T, Iversen PO. Body composition in older acute stroke patients after treatment with individualized, nutritional supplementation while in hospital. BMC Geriatr. 2010; 10:75.
Article30. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M; Educational and Clinical Practice Committee. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003; 22:415–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the Clinical Effect of Intravenous Glutamine on Intensive Care Unit Patients
- Delirium in the intensive care unit
- Influence of sarcopenia focused on critically ill patients
- Factors Influencing Delirium in Neurological Intensive Care Unit Patient
- Nosocomial Infections in Intensive Care Unit: Epidemiology and Control Strategy