Ewha Med J.
2016 Oct;39(4):129-132. 10.12771/emj.2016.39.4.129.
Acute Liver Injury Caused by Diffuse Lymphangitic Liver Metastasis from Colon Cancer
- Affiliations
-
- 1Department of Internal Medicine, National Cancer Center Hospital, Goyang, Korea.
- 2Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. cathykimmd@gmail.com
- 3Center for Colorectal Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 4Center for Liver Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- KMID: 2356386
- DOI: http://doi.org/10.12771/emj.2016.39.4.129
Abstract
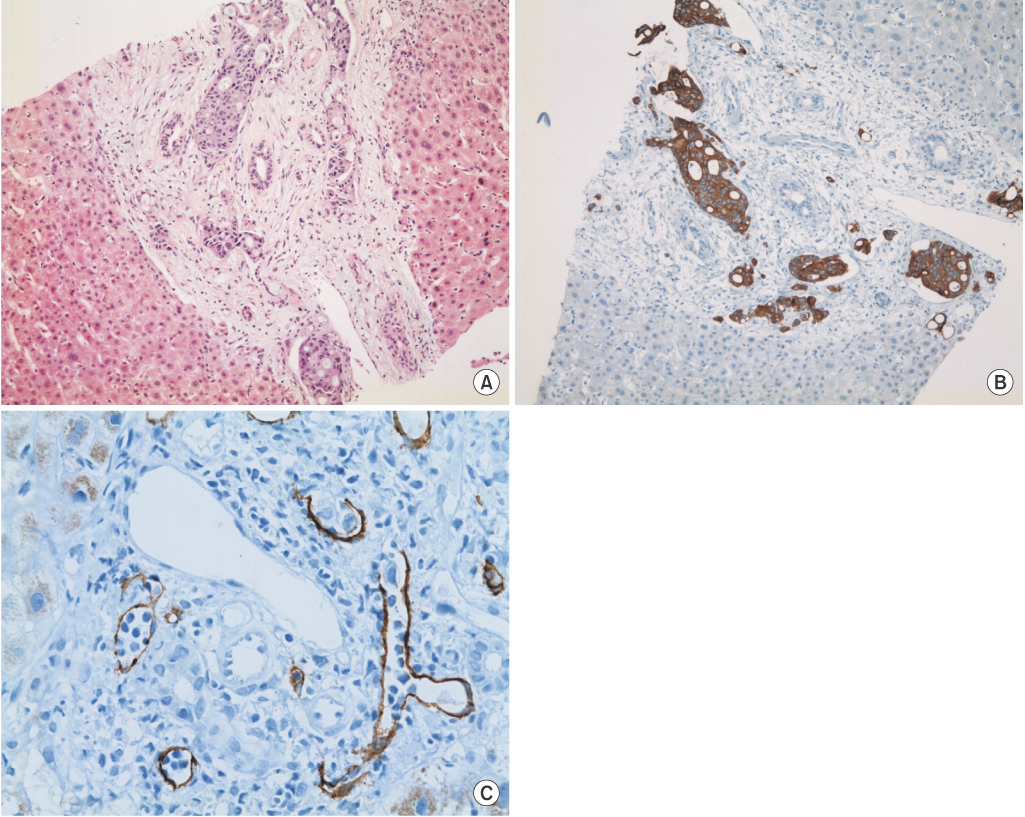
- A 56-year-old man was diagnosed with cancer of the ascending colon along with retroperitoneal lymph node and peritoneal metastases. After six cycles of palliative chemotherapy, he presented with acute-onset jaundice. Imaging examinations did not show abnormal liver findings other than a periportal linear hypoattenuating area, and endoscopic retrograde cholangiography revealed a tight stricture of the proximal common bile duct. Total bilirubin continued to increase after endoscopic sphincterotomy and biliary stent insertion. Blind liver biopsy revealed tumor infiltration along liver lymphatics, but ruled out tumor involvement of hepatic parenchyma and sinusoids. Tumor cells were predominantly confined to within the lymphatic vessels and were not observed in the arteries or veins. Although one loading dose of cetuximab and two fractions of palliative radiotherapy were administered, the patient succumbed to acute liver injury 30 days after the development of jaundice.
Keyword
MeSH Terms
-
Arteries
Bilirubin
Biopsy
Cetuximab
Cholangiography
Colon*
Colon, Ascending
Colonic Neoplasms*
Common Bile Duct
Constriction, Pathologic
Drug Therapy
Humans
Jaundice
Liver*
Lymph Nodes
Lymphatic Metastasis
Lymphatic Vessels
Middle Aged
Neoplasm Metastasis*
Radiotherapy
Sphincterotomy, Endoscopic
Stents
Veins
Bilirubin
Cetuximab
Figure
Reference
-
1. Moreau R, Arroyo V. Acute-on-chronic liver failure: a new clinical entity. Clin Gastroenterol Hepatol. 2015; 13:836–841.2. Hall J, Schmidt G, Kress J. Principles of critical care. 4th ed. Columbus, OH: McGraw Hill Professional;2015.3. Ihara N, Yashiro N, Kinoshita T, Yoshigi J, Ouchi T, Narita M, et al. Diffuse intrasinusoidal liver metastasis of small cell lung cancer causing fulminant hepatic failure: CT findings-a case report. Radiat Med. 2001; 19:275–277.4. Wandroo FA, Murray J, Mutimer D, Hubscher S. Acute myeloid leukaemia presenting as cholestatic hepatitis. J Clin Pathol. 2004; 57:544–545.5. Itoh T, Kanaoka M, Obara A, Furuta M, Itoh H. Lymphangiosis carcinomatosa of the liver. Acta Pathol Jpn. 1988; 38:751–758.6. Matsumoto S, Mori H, Ando Y, Miyake H. Lymphangiosis carcinomatosa of the liver deriving from gastric carcinoma with a unique branching calcification. Eur Radiol. 2004; 14:1519–1520.7. Tada H, Morimoto M, Shima T, Hirana H, Nakagawa Y, Shimamoto K, et al. Progressive jaundice due to lymphangiosis carcinomatosa of the liver: CT appearance. J Comput Assist Tomogr. 1996; 20:650–652.8. Lee Y, Lee JS, Kim CM, Jeong JY, Choi JI, Kim MJ. Area of paradoxical signal drop after the administration of superparamagnetic iron oxide on the T2-weighted image of a patient with lymphangitic metastasis of the liver. Magn Reson Imaging. 2008; 26:577–582.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver Metastasis of Colon Cancer
- Liver Metastasis Mimicking Cholangiocarcinoma from Colon Cancer
- The Prognosis and Recurrence Pattern of Right- and Left-Sided Colon Cancer in Stage II, Stage III, and Liver Metastasis After Curative Resection
- Liver Metastasis of Colon Cancer with a High Serum alpha-Fetoprotein Level: Report of a Case
- Acute Liver Failure Secondary to Hepatic Infiltration of Malignant Melanoma