Ann Surg Treat Res.
2016 Nov;91(5):247-253. 10.4174/astr.2016.91.5.247.
The natural course of pancreatic fistula and fluid collection after distal pancreatectomy: is drain insertion needed?
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. sunkim@snu.ac.kr
- 2Department of Surgery, Dankook University Hospital, Cheonan, Korea.
- KMID: 2356375
- DOI: http://doi.org/10.4174/astr.2016.91.5.247
Abstract
- PURPOSE
Postoperative pancreatic fistula (POPF) is one of the most common and clinically relevant complications after distal pancreatectomy. Some aspects of POPF management remain controversial. Therefore, the aim of this study was to determine the natural course of POPF and fluid collection after distal pancreatectomy and to reappraise the necessity of intraoperative abdominal drainage insertion.
METHODS
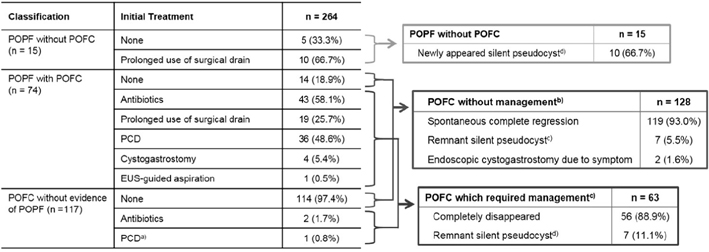
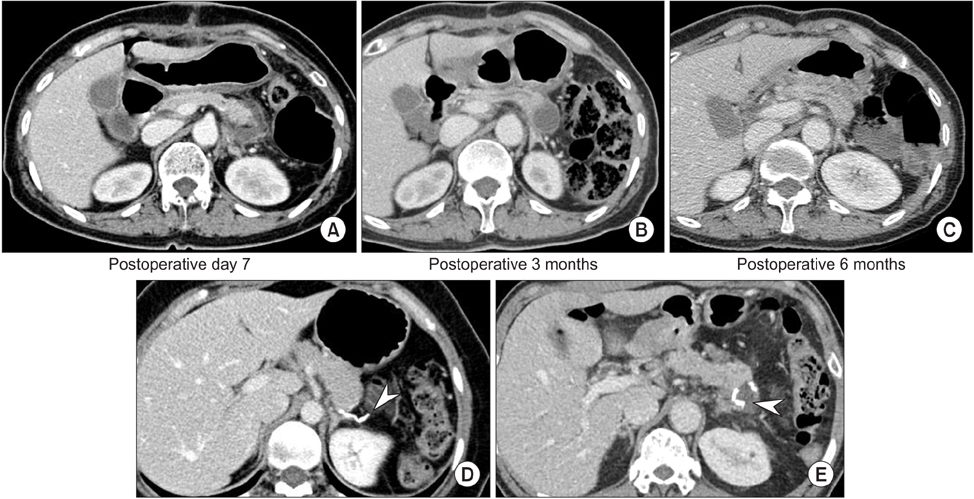
For recent 10 years, 264 distal pancreatectomies were performed at Seoul National University Hospital. Clinicopathologic data including POPF and postoperative fluid collection (POFC), and its treatment modality were reviewed retrospectively. During follow-up, the location, size, and clinical impact of the POFC were determined on the basis of CT images.
RESULTS
Clinically relevant POPFs were identified in 72 patients (27.3%). Therapeutic interventions were performed in 40 patients (55.6%), and conservative management was successful in 32 patients (44.4%). POFC was detected in 191 cases (72.3%) on the first postoperative CT. During follow-up, spontaneous regressions were observed in 119 cases (93.0%). Only thick pancreatic stump increased the risk of clinically relevant POPF (≥17.3 mm, P = 0.002) and the occurrence of POFC (≥16.0 mm, P < 0.001) in multivariate analysis.
CONCLUSION
Intraoperative abdominal drainage insertion could be selectively indwelled in patients with a thickness of pancreas ≥17.3 mm. Since radiologically-proven POFC after distal pancreatecomy showed a 93.0 rate of spontaneous regression, POFC without signs of infection can be safely monitored.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Bile duct segmental resection versus pancreatoduodenectomy for middle and distal common bile duct cancer
Naru Kim, Huisong Lee, Seog Ki Min, Hyeon Kook Lee
Ann Surg Treat Res. 2018;94(5):240-246. doi: 10.4174/astr.2018.94.5.240.
Reference
-
1. Butturini G, Marcucci S, Molinari E, Mascetta G, Landoni L, Crippa S, et al. Complications after pancreaticoduodenectomy: the problem of current definitions. J Hepatobiliary Pancreat Surg. 2006; 13:207–211.2. Melloul E, Raptis DA, Clavien PA, Lesurtel M. European-African Hepato-Pancreato-Biliary Association. Poor level of agreement on the management of postoperative pancreatic fistula: results of an international survey. HPB (Oxford). 2013; 15:307–314.3. Strasberg SM, Linehan DC, Clavien PA, Barkun JS. Proposal for definition and severity grading of pancreatic anastomosis failure and pancreatic occlusion failure. Surgery. 2007; 141:420–426.4. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13.5. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.6. Kleeff J, Diener MK, Z'graggen K, Hinz U, Wagner M, Bachmann J, et al. Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg. 2007; 245:573–582.7. Balcom JH 4th, Rattner DW, Warshaw AL, Chang Y, Fernandez-del Castillo C. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001; 136:391–398.8. Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, Yeo CJ. Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg. 1999; 229:693–698.9. Balzano G, Zerbi A, Cristallo M, Di Carlo V. The unsolved problem of fistula after left pancreatectomy: the benefit of cautious drain management. J Gastrointest Surg. 2005; 9:837–842.10. Kaminsky PM, Mezhir JJ. Intraperitoneal drainage after pancreatic resection: a review of the evidence. J Surg Res. 2013; 184:925–930.11. Williamsson C, Karlsson N, Sturesson C, Lindell G, Andersson R, Tingstedt B. Impact of a fast-track surgery programme for pancreaticoduodenectomy. Br J Surg. 2015; 102:1133–1141.12. Paulus EM, Zarzaur BL, Behrman SW. Routine peritoneal drainage of the surgical bed after elective distal pancreatectomy: is it necessary. Am J Surg. 2012; 204:422–427.13. van der Wilt AA, Coolsen MM, de Hingh IH, van der Wilt GJ, Groenewoud H, Dejong CH, et al. To drain or not to drain: a cumulative meta-analysis of the use of routine abdominal drains after pancreatic resection. HPB (Oxford). 2013; 15:337–344.14. Conlon KC, Labow D, Leung D, Smith A, Jarnagin W, Coit DG, et al. Prospective randomized clinical trial of the value of intraperitoneal drainage after pancreatic resection. Ann Surg. 2001; 234:487–493.15. Fisher WE, Hodges SE, Silberfein EJ, Artinyan A, Ahern CH, Jo E, et al. Pancreatic resection without routine intraperitoneal drainage. HPB (Oxford). 2011; 13:503–510.16. Vin Y, Sima CS, Getrajdman GI, Brown KT, Covey A, Brennan MF, et al. Management and outcomes of postpancreatectomy fistula, leak, and abscess: results of 908 patients resected at a single institution between 2000 and 2005. J Am Coll Surg. 2008; 207:490–498.17. Rieder B, Krampulz D, Adolf J, Pfeiffer A. Endoscopic pancreatic sphincterotomy and stenting for preoperative prophylaxis of pancreatic fistula after distal pancreatectomy. Gastrointest Endosc. 2010; 72:536–542.18. Frozanpor F, Lundell L, Segersvard R, Arnelo U. The effect of prophylactic transpapillary pancreatic stent insertion on clinically significant leak rate following distal pancreatectomy: results of a prospective controlled clinical trial. Ann Surg. 2012; 255:1032–1036.19. Wagner M, Gloor B, Ambuhl M, Worni M, Lutz JA, Angst E, et al. Roux-en-Y drainage of the pancreatic stump decreases pancreatic fistula after distal pancreatic resection. J Gastrointest Surg. 2007; 11:303–308.20. Okada K, Kawai M, Tani M, Hirono S, Miyazawa M, Shimizu A, et al. Isolated Roux-en-Y anastomosis of the pancreatic stump in a duct-to-mucosa fashion in patients with distal pancreatectomy with en-bloc celiac axis resection. J Hepatobiliary Pancreat Sci. 2014; 21:193–198.21. Pannegeon V, Pessaux P, Sauvanet A, Vullierme MP, Kianmanesh R, Belghiti J. Pancreatic fistula after distal pancreatectomy: predictive risk factors and value of conservative treatment. Arch Surg. 2006; 141:1071–1076.22. Goh BK, Tan YM, Chung YF, Cheow PC, Ong HS, Chan WH, et al. Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg. 2008; 143:956–965.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors of postoperative pancreatic fistula after splenectomy with or without distal pancreatectomy performed as a component of cytoreductive surgery for advanced ovarian cancer
- Does international study group on pancreatic fistula (ISGPF) classification need modification after distal pancreatectomy?
- Complication analysis of distal pancreatectomy based on early personal experience
- Fatal liver injury complicated by percutaneous catheter drainage after distal pancreatosplenectomy in a patient with pancreatic cancer
- Predictive value of post-operative drain amylase levels for post-operative pancreatic fistula