Korean J Hepatobiliary Pancreat Surg.
2014 May;18(2):64-67. 10.14701/kjhbps.2014.18.2.64.
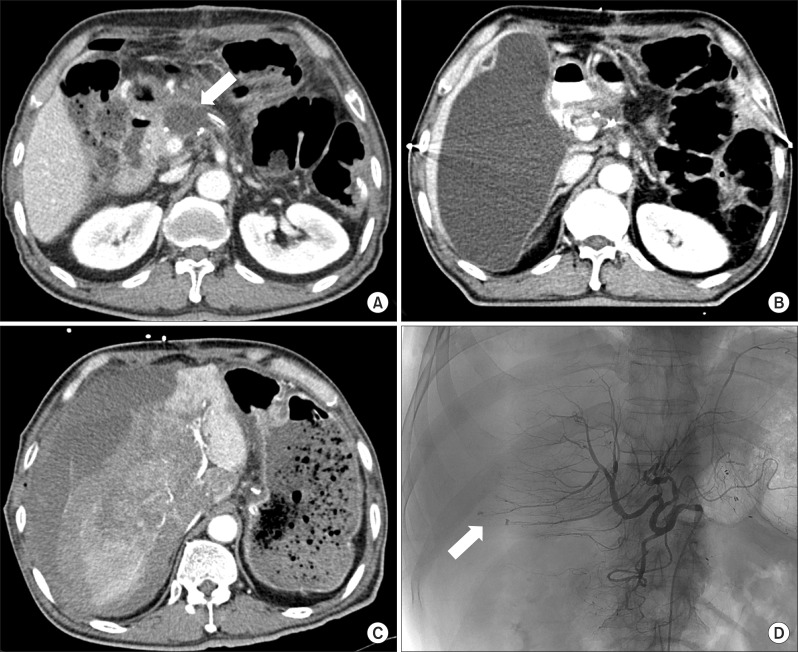
Fatal liver injury complicated by percutaneous catheter drainage after distal pancreatosplenectomy in a patient with pancreatic cancer
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. cmkang@yuhs.ac
- 2Department of Radiology, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea.
- 4Pancreaticobiliary Cancer Clinic, Institute of Gastroenterology, Severance Hospital, Seoul, Korea.
- KMID: 2305246
- DOI: http://doi.org/10.14701/kjhbps.2014.18.2.64
Abstract
- Postoperative pancreatic fistula (POPF) combined with postoperative fluid collection, bleeding and abscess formation is one of the most critical morbidities after distal pancreatectomy or pancreaticoduodenectomy. Percutaneous catheter drainage has been commonly used for managing for the postoperative management of abnormal fluid collection. Removal of the catheter is rarely associated with occurrence of life-threatening complication such as serious liver damage. Herein, we report a case of unexpected fatal liver injury complicated by percutaneous catheter drainage treatment after distal pancreatosplenectomy in a patient with pancreatic cancer. We suggest that prudent decision for timing of catheter removal and meticulous care during procedure can reduce the possibility of major liver injury in patients with percutaneous transhepatic catheter drainage.
Keyword
MeSH Terms
Figure
Reference
-
1. vanSonnenberg E, Wittich GR, Casola G, Brannigan TC, Karnel F, Stabile BE, et al. Percutaneous drainage of infected and noninfected pancreatic pseudocysts: experience in 101 cases. Radiology. 1989; 170:757–761. PMID: 2644662.
Article2. Aghdassi A, Mayerle J, Kraft M, Sielenkämper AW, Heidecke CD, Lerch MM. Diagnosis and treatment of pancreatic pseudocysts in chronic pancreatitis. Pancreas. 2008; 36:105–112. PMID: 18376299.
Article3. Ciftci TT, Akinci D, Akhan O. Percutaneous transhepatic drainage of inaccessible postoperative abdominal abscesses. AJR Am J Roentgenol. 2012; 198:477–481. PMID: 22268197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Port-site metastasis after laparoscopic radical pancreatosplenectomy in left-sided pancreatic cancer
- Percutaneous Catheter Drainage of Pancreatic Pseudocyst through the Kidney: A case Report
- Early percutaneous external drainage procedure in treatment of pancreatic pseudocyst
- Percutaneous Drainage of Pancreatic Pseudocysts: Analysis of 16 Cases
- Treatment of P yogenic Liver Abscess by Percutaneous Needle Aspiration and / or Percutaneous Catheter Drainage