Intest Res.
2016 Oct;14(4):297-304. 10.5217/ir.2016.14.4.297.
Irritable bowel syndrome and inflammatory bowel disease overlap syndrome: pieces of the puzzle are falling into place
- Affiliations
-
- 1Gastroenterology Unit, Faculty of Medicine, Universiti Teknologi MARA, Sungai Buloh, Malaysia.
- 2Gastroenterology Unit, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia.
- 3School of Medical Sciences, Universiti Sains Malaysia, Kota Bharu, Malaysia. yylee@usm.my
- KMID: 2354947
- DOI: http://doi.org/10.5217/ir.2016.14.4.297
Abstract
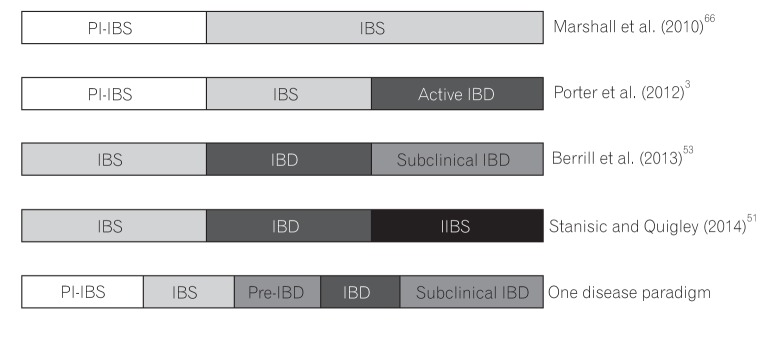
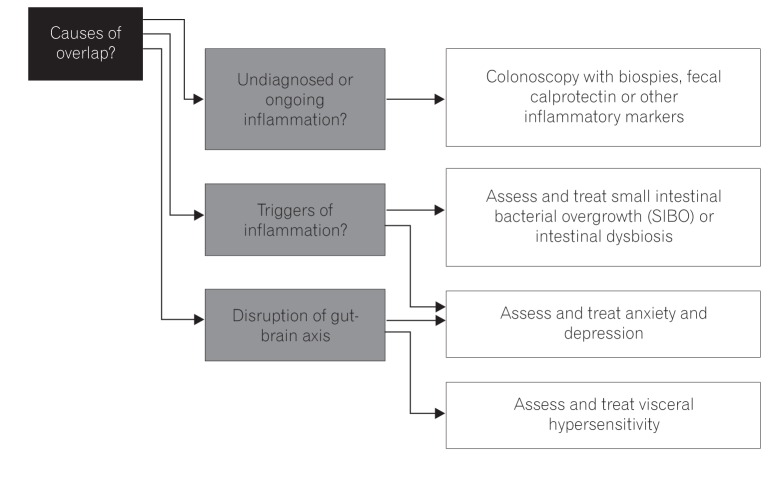
- Irritable bowel syndrome (IBS), a common gastrointestinal disorder involving the gut-brain axis, and inflammatory bowel disease (IBD), a chronic relapsing inflammatory disorder, are both increasing in incidence and prevalence in Asia. Both have significant overlap in terms of symptoms, pathophysiology, and treatment, suggesting the possibility of IBS and IBD being a single disease entity albeit at opposite ends of the spectrum. We examined the similarities and differences in IBS and IBD, and offer new thoughts and approaches to the disease paradigm.
Keyword
MeSH Terms
Figure
Reference
-
1. Halpin SJ, Ford AC. Prevalence of symptoms meeting criteria for irritable bowel syndrome in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2012; 107:1474–1482. PMID: 22929759.
Article2. García Rodríguez LA, Ruigómez A, Wallander MA, Johansson S, Olbe L. Detection of colorectal tumor and inflammatory bowel disease during follow-up of patients with initial diagnosis of irritable bowel syndrome. Scand J Gastroenterol. 2000; 35:306–311. PMID: 10766326.
Article3. Porter CK, Cash BD, Pimentel M, Akinseye A, Riddle MS. Risk of inflammatory bowel disease following a diagnosis of irritable bowel syndrome. BMC Gastroenterol. 2012; 12:55. PMID: 22639930.
Article4. Porter CK, Tribble DR, Aliaga PA, Halvorson HA, Riddle MS. Infectious gastroenteritis and risk of developing inflammatory bowel disease. Gastroenterology. 2008; 135:781–786. PMID: 18640117.
Article5. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.e42. PMID: 22001864.
Article6. Park SJ, Kim WH, Cheon JH. Clinical characteristics and treatment of inflammatory bowel disease: a comparison of Eastern and Western perspectives. World J Gastroenterol. 2014; 20:11525–11537. PMID: 25206259.
Article7. Lee OY. Prevalence and risk factors of irritable bowel syndrome in Asia. J Neurogastroenterol Motil. 2010; 16:5–7. PMID: 20535320.
Article8. Gwee KA, Bak YT, Ghoshal UC, et al. Asian consensus on irritable bowel syndrome. J Gastroenterol Hepatol. 2010; 25:1189–1205. PMID: 20594245.
Article9. Lee YY, Waid A, Tan HJ, Chua AS, Whitehead WE. Rome III survey of irritable bowel syndrome among ethnic Malays. World J Gastroenterol. 2012; 18:6475–6480. PMID: 23197894.
Article10. Yao T, Matsui T, Hiwatashi N. Crohn's disease in Japan: diagnostic criteria and epidemiology. Dis Colon Rectum. 2000; 43(10 Suppl):S85–S93. PMID: 11052483.11. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.
Article12. Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol. 2008; 103:3167–3182. PMID: 19086963.
Article13. Lok KH, Hung HG, Ng CH, et al. Epidemiology and clinical characteristics of ulcerative colitis in Chinese population: experience from a single center in Hong Kong. J Gastroenterol Hepatol. 2008; 23:406–410. PMID: 17623033.
Article14. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280. PMID: 22497584.
Article15. Zhu X, Chen W, Zhu X, Shen Y. A cross-sectional study of risk factors for irritable bowel syndrome in children 8-13 years of age in Suzhou, China. Gastroenterol Res Pract. 2014; 2014:198461. PMID: 24899889.
Article16. Gwee KA. Irritable bowel syndrome in developing countries: a disorder of civilization or colonization? Neurogastroenterol Motil. 2005; 17:317–324. PMID: 15916618.
Article17. Gwee KA, Lu CL, Ghoshal UC. Epidemiology of irritable bowel syndrome in Asia: something old, something new, something borrowed. J Gastroenterol Hepatol. 2009; 24:1601–1607. PMID: 19788601.
Article18. Quigley EM. Overlapping irritable bowel syndrome and inflammatory bowel disease: less to this than meets the eye? Therap Adv Gastroenterol. 2016; 9:199–212.
Article19. Mikocka-Walus A, Pittet V, Rossel JB, von Känel R. Swiss IBD Cohort Study Group. Symptoms of depression and anxiety are independently associated with clinical recurrence of inflammatory bowel disease. Clin Gastroenterol Hepatol. 2016; 14:829–835.e1. PMID: 26820402.20. Fagundes CP, Glaser R, Hwang BS, Malarkey WB, Kiecolt-Glaser JK. Depressive symptoms enhance stress-induced inflammatory responses. Brain Behav Immun. 2013; 31:172–176. PMID: 22634107.
Article21. Johnson JD, O'Connor KA, Deak T, Stark M, Watkins LR, Maier SF. Prior stressor exposure sensitizes LPS-induced cytokine production. Brain Behav Immun. 2002; 16:461–476. PMID: 12096891.
Article22. Salazar G. Depression and IBD. J Pediatr Gastroenterol Nutr. 2014; 58:543–544. PMID: 24509306.
Article23. Mikocka-Walus AA, Turnbull DA, Moulding NT, Wilson IG, Andrews JM, Holtmann GJ. Controversies surrounding the comorbidity of depression and anxiety in inflammatory bowel disease patients: a literature review. Inflamm Bowel Dis. 2007; 13:225–234. PMID: 17206706.
Article24. Graff LA, Walker JR, Bernstein CN. Depression and anxiety in inflammatory bowel disease: a review of comorbidity and management. Inflamm Bowel Dis. 2009; 15:1105–1118. PMID: 19161177.
Article25. Lydiard RB. Irritable bowel syndrome, anxiety, and depression: what are the links? J Clin Psychiatry. 2001; 62(Suppl 8):38–45.26. Padhy SK, Sahoo S, Mahajan S, Sinha SK. Irritable bowel syndrome: is it "irritable brain" or "irritable bowel"? J Neurosci Rural Pract. 2015; 6:568–577. PMID: 26752904.
Article27. Jones MP, Dilley JB, Drossman D, Crowell MD. Brain-gut connections in functional GI disorders: anatomic and physiologic relationships. Neurogastroenterol Motil. 2006; 18:91–103. PMID: 16420287.
Article28. Zucchelli M, Camilleri M, Andreasson AN, et al. Association of TNFSF15 polymorphism with irritable bowel syndrome. Gut. 2011; 60:1671–1677. PMID: 21636646.
Article29. Swan C, Duroudier NP, Campbell E, et al. Identifying and testing candidate genetic polymorphisms in the irritable bowel syndrome (IBS): association with TNFSF15 and TNF-alpha. Gut. 2013; 62:985–994. PMID: 22684480.
Article30. von Stein P, Lofberg R, Kuznetsov NV, et al. Multigene analysis can discriminate between ulcerative colitis, Crohn's disease, and irritable bowel syndrome. Gastroenterology. 2008; 134:1869–1881. PMID: 18466904.
Article31. Casén C, Vebø HC, Sekelja M, et al. Deviations in human gut microbiota: a novel diagnostic test for determining dysbiosis in patients with IBS or IBD. Aliment Pharmacol Ther. 2015; 42:71–83. PMID: 25973666.
Article32. Quigley EM. Bacterial flora in irritable bowel syndrome: role in pathophysiology, implications for management. J Dig Dis. 2007; 8:2–7. PMID: 17261128.
Article33. Lee YY, Rao SS. Post-infectious irritable bowel syndrome. Biotascope. 2015; 2:10–16.
Article34. Spiller R, Lam C. The shifting interface between IBS and IBD. Curr Opin Pharmacol. 2011; 11:586–592. PMID: 22000604.
Article35. Spiller R, Campbell E. Post-infectious irritable bowel syndrome. Curr Opin Gastroenterol. 2006; 22:13–17. PMID: 16319671.
Article36. Rhodes DY, Wallace M. Post-infectious irritable bowel syndrome. Curr Gastroenterol Rep. 2006; 8:327–332. PMID: 16836945.
Article37. Joossens M, Huys G, Cnockaert M, et al. Dysbiosis of the faecal microbiota in patients with Crohn's disease and their unaffected relatives. Gut. 2011; 60:631–637. PMID: 21209126.
Article38. Sokol H, Seksik P, Furet JP, et al. Low counts of Faecalibacterium prausnitzii in colitis microbiota. Inflamm Bowel Dis. 2009; 15:1183–1189. PMID: 19235886.
Article39. Hedin CR, Stagg AJ, Whelan K, Lindsay JO. Family studies in Crohn's disease: new horizons in understanding disease pathogenesis, risk and prevention. Gut. 2012; 61:311–318. PMID: 21561876.
Article40. Bernstein CN, Singh S, Graff LA, Walker JR, Miller N, Cheang M. A prospective population-based study of triggers of symptomatic flares in IBD. Am J Gastroenterol. 2010; 105:1994–2002. PMID: 20372115.
Article41. Zhou Q, Souba WW, Croce CM, Verne GN. MicroRNA-29a regulates intestinal membrane permeability in patients with irritable bowel syndrome. Gut. 2010; 59:775–784. PMID: 19951903.
Article42. Akbar A, Walters JR, Ghosh S. Review article: visceral hypersensitivity in irritable bowel syndrome: molecular mechanisms and therapeutic agents. Aliment Pharmacol Ther. 2009; 30:423–435. PMID: 19493256.
Article43. Keszthelyi D, Jonkers DM, Hamer HM, Masclee AA. Letter: the role of sub-clinical inflammation and TRPV1 in the development of IBS-like symptoms in ulcerative colitis in remission. Aliment Pharmacol Ther. 2013; 38:560–561.
Article44. Keohane J, O'Mahony C, O'Mahony L, O'Mahony S, Quigley EM, Shanahan F. Irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease: a real association or reflection of occult inflammation? Am J Gastroenterol. 2010; 105:17881789–1794. PMID: 20389294.
Article45. Melchior CA, Aubry T, Gourcerol G, Leroi AM, Ducrotté P. Fecal calprotectin levels in IBS patients: results from prospective study. United European Gastroenterol J. 2013; 1(Suppl 1):A68.46. Jelsness-Jørgensen LP, Bernklev T, Moum B. Calprotectin is a useful tool in distinguishing coexisting irritable bowel-like symptoms from that of occult inflammation among inflammatory bowel disease patients in remission. Gastroenterol Res Pract. 2013; 2013:620707. PMID: 23476638.
Article47. Hod K, Ringel-Kulka T, Martin CF, Maharshak N, Ringel Y. High-sensitive C-reactive protein as a marker for inflammation in irritable bowel syndrome. J Clin Gastroenterol. 2016; 50:227–232. PMID: 25930973.
Article48. Zhou XL, Xu W, Tang XX, et al. Fecal lactoferrin in discriminating inflammatory bowel disease from irritable bowel syndrome: a diagnostic meta-analysis. BMC Gastroenterol. 2014; 14:121. PMID: 25002150.
Article49. Menees SB, Powell C, Kurlander J, Goel A, Chey WD. A meta-analysis of the utility of C-reactive protein, erythrocyte sedimentation rate, fecal calprotectin, and fecal lactoferrin to exclude inflammatory bowel disease in adults with IBS. Am J Gastroenterol. 2015; 110:444–454. PMID: 25732419.
Article50. Vivinus-Nébot M, Frin-Mathy G, Bzioueche H, et al. Functional bowel symptoms in quiescent inflammatory bowel diseases: role of epithelial barrier disruption and low-grade inflammation. Gut. 2014; 63:744–752. PMID: 23878165.
Article51. Stanisic V, Quigley EM. The overlap between IBS and IBD: what is it and what does it mean? Expert Rev Gastroenterol Hepatol. 2014; 8:139–145. PMID: 24417262.52. Villani AC, Lemire M, Thabane M, et al. Genetic risk factors for post-infectious irritable bowel syndrome following a waterborne outbreak of gastroenteritis. Gastroenterology. 2010; 138:1502–1513. PMID: 20044998.
Article53. Berrill JW, Green JT, Hood K, Campbell AK. Symptoms of irritable bowel syndrome in patients with inflammatory bowel disease: examining the role of sub-clinical inflammation and the impact on clinical assessment of disease activity. Aliment Pharmacol Ther. 2013; 38:44–51. PMID: 23668698.
Article54. Bercik P, Verdu EF, Collins SM. Is irritable bowel syndrome a low-grade inflammatory bowel disease? Gastroenterol Clin North Am. 2005; 34:235–245. PMID: 15862932.
Article55. Quigley EM. Irritable bowel syndrome and inflammatory bowel disease: interrelated diseases? Chin J Dig Dis. 2005; 6:122–132. PMID: 16045602.
Article56. Hilmi I, Hartono JL, Pailoor J, Mahadeva S, Goh KL. Low prevalence of 'classical' microscopic colitis but evidence of microscopic inflammation in Asian irritable bowel syndrome patients with diarrhoea. BMC Gastroenterol. 2013; 13:80. PMID: 23651739.
Article57. Erdogan A, Rao SS, Gulley D, Jacobs C, Lee YY, Badger C. Small intestinal bacterial overgrowth: duodenal aspiration vs glucose breath test. Neurogastroenterol Motil. 2015; 27:481–489. PMID: 25600077.
Article58. Rao SS, Lee YY. Approach to the patient with gas and bloating. In : Podolsky DK, Camilleri M, Fitz JG, Kalloo AN, Shanahan F, Wang TC, editors. Yamada's textbook of gastroenterology. Oxford: John Wiley & Sons;2015. p. 723–734.59. Keefer L, Taft TH, Kiebles JL, Martinovich Z, Barrett TA, Palsson OS. Gut-directed hypnotherapy significantly augments clinical remission in quiescent ulcerative colitis. Aliment Pharmacol Ther. 2013; 38:761–771. PMID: 23957526.
Article60. Rutten JM, Vlieger AM, Frankenhuis C, et al. Gut-directed hypnotherapy in children with irritable bowel syndrome or functional abdominal pain (syndrome): a randomized controlled trial on self exercises at home using CD versus individual therapy by qualified therapists. BMC Pediatr. 2014; 14:140. PMID: 24894077.
Article61. Triantafillidis JK, Merikas E, Gikas A. Psychological factors and stress in inflammatory bowel disease. Expert Rev Gastroenterol Hepatol. 2013; 7:225–238. PMID: 23445232.
Article62. Triantafillidis JK, Vagianos K, Rontos I. Psychotic reaction as a cardinal first clinical manifestation in a patient with Crohn's disease. J Crohns Colitis. 2013; 7:e76–e77. DOI: 10.1016/j.crohns.2012.07.003. PMID: 22854290.
Article63. Barbara G, Cremon C, Annese V, et al. Randomised controlled trial of mesalazine in IBS. Gut. 2016; 65:82–90. PMID: 25533646.
Article64. Iskandar HN, Cassell B, Kanuri N, et al. Tricyclic antidepressants for management of residual symptoms in inflammatory bowel disease. J Clin Gastroenterol. 2014; 48:423–429. PMID: 24406434.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammation and Overlap of Irritable Bowel Syndrome and Functional Dyspepsia
- Irritable bowel syndrome
- Overlap Syndrome of Functional Dyspepsia and Irritable Bowel Syndrome - Are Both Diseases Mutually Exclusive?
- Decreased Neuroplasticity May Play a Role in Irritable Bowel Syndrome: Implication From the Comorbidity of Depression and Irritable Bowel Syndrome
- Pharmacological therapy for irritable bowel syndrome